Those who are familiar with severe lumbar pain or have serious problems with the spine know firsthand what a blockade is. This difficult procedure is considered today to be practically the only method of quickly relieving pain that arises in the back due to deformities or other pathologies of the vertebral arch. The blockade does not serve as a method of treatment and cannot be one. But an injection can relieve pain in a matter of minutes. What a blockade is, for what indications and how it is done, and what contraindications or complications this procedure may have is useful to know.
Blockade for lower back pain
Why blockade relieves pain
To understand the mechanism of action of the blockade, it is necessary to understand how pain occurs and how it affects.
Prices for painkillers for back pain
How pain occurs
Pathological phenomena in the spinal column are the reason why the spinal nerves become pinched. When a nerve is compressed, it transmits pain to a limb or neck, lower back, and so on. The location of pain depends directly on the location of the pinched nerve.
Pinched nerve in the lower back
Important! If the painful sensation occurs once or not often, it is relieved by a single dose of drugs that affect the source of pain. But if the symptom becomes chronic, a centralized inflamed pain focus forms in the cerebral cortex. It cannot be removed using standard treatment methods.
In cases where lower back pain becomes severe and constant, they resort to a blockade as the only way to relieve it. The injection turns off (disables) one of the links in the chain of movement of the pain reflex, which is why the entire movement of pain is interrupted, and the impulse does not reach the limbs and organs.
This procedure is not a method of treating back diseases, but only a way to relieve pain.
In some cases, a blockade injection is used for diagnostic measures to establish the true cause of pain.
Products for the treatment of injuries, muscle and joint pain
What is a blockade injection
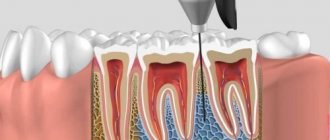
What is this procedure? Through the injection, the nerve conduction of the fibers that transmit pain to the organs is reduced/switched off. For this purpose, local anesthetics are used, which act by inhibition to block sodium channels.
The pain syndrome goes away in almost a minute or two, and if this does not happen, a thorough diagnosis and search for other causes of pain are necessary.
For blockade, local anesthetics are used that block cell conduction by inhibiting voltage-gated sodium channels
The blockade injection is performed exclusively in the clinic, and only by doctors who have professional clearance for this procedure. A specialist needs not only medical knowledge, but also topographical and anatomical knowledge. Most often, specialists who meet the necessary requirements work in traumatology or neurosurgery in clinics and hospitals. Therefore, the procedure is carried out there.
Carrying out the blockade, photo
What is the difficulty of implementing a blockade? In the insecurity of the spinal cord. It would seem that, enclosed in a durable shell of the vertebral arch, the spinal cord remains one of the most vulnerable organs, which is afraid of the slightest penetration of bacteria. Viral infection of the spinal cord can lead to death of the patient. Therefore, the blockade is performed only under sterile conditions, where surgical operations are usually performed. The specialist wears gloves.
The procedure is carried out under sterile conditions
By the way. The procedure is reminiscent of taking puncture lumbar fluid, only during the blockade the patient is positioned differently, and the injection can be given not only in the lower back (depending on the location of the pain).
Advantages of blockade as an analgesic method
This method of relieving the patient of lower back pain has many advantages.
GV and anesthesia
The Association of Anaesthetists (UK) has published new recommendations on the use of anesthesia and sedation in breastfeeding mothers “Guideline on anaesthesia and sedation in breastfeedingwomen 2020” (Anaesthesia 2022, 75, 1482–1493). I will not write much about the arguments on various issues, but will simply give a short list of recommendations that should hang in the office of every obstetrician-gynecologist in the form of a large poster.
Women should be encouraged to breastfeed as usual after surgery.
There is no need to express and throw away breast milk.
Anesthetics and non-opioid pain medications pass into milk in excessively small quantities. For other drugs that are used during surgery, there is no reliable data on harm to the newborn.
Medicines like opioids and benzodiazepines should be used with caution, especially after multiple doses and in the presence of a baby under 6 weeks of age (adjusted for gestational age). In this situation, the newborn should be observed for abnormal somnolence and depressed breathing, especially in women who show signs of sedation.
Codeine should not be used by women who are breastfeeding due to the potential for excessive sedation in newborns due to differences in metabolism.
Any woman with a child under 2 years of age should be asked whether she is breastfeeding in preparation for surgery.
Non-opioid pain management techniques are preferred for hepatitis B. Local and regional anesthesia have advantages in this regard and have the least impact on a woman's ability to care for her baby.
If possible, day surgery (in day hospitals) is preferable so as not to disrupt the woman's routine activities. A woman having surgery as a day hospital is advised to have a responsible adult nearby for the first 24 hours after surgery. She should be careful about sleeping with the baby or sleeping in a chair while feeding the baby as she may not be as adequate as normal.
Breastfeeding support should be available to women undergoing surgery and medical procedures.
Patient information leaflets and additional resources should be available that provide information on the compatibility of anesthetics and analgesics during breastfeeding, as well as recommendations for perioperative breastfeeding support.
RETURN to Blog Dr. Elena Berezovskaya
Share link:
- Click to share on WhatsApp (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Skype (Opens in new window)
- Send this to a friend (Opens in new window)
- Click to print (Opens in new window)
By
What types of blockades are divided into?
There are many types of blockades. They are classified mainly by the location of the pain. But injections have not only a direct targeted effect. For example, a blockade in the neck, in the area of vertebrae 1-7, can relieve pain from the entire back, along the entire spine.
Table. Types of blockades by area of effect.
| Variety | Scope |
| It is done in the area of the six upper vertebrae belonging to the cervical segment and the seventh transitional segment. Relieves pain in the head and neck, and throughout the spine. Eliminates pain in the hands. |
| Thoracolumbar | It relieves pain in the lower back, legs, and also relieves pain in the intestines. |
| Blocks pain in the spine responsible for the lower back. |
| Combats pain at the lumbosacral level. It is often used (like the lumbar) for diagnostic purposes. |
| Level 1-12 thoracic vertebrae is the site of a thoracic blockade, which relieves pain syndromes in the upper extremities, torso, internal organs and throughout the back. |
| The difference between this type is that the injection is placed in a branch of the nerve without affecting the entire spinal cord. In this way, half of the body or a specific organ is anesthetized. This is enough to relieve narrow-point pain syndrome or perform a diagnostic procedure. An anesthetic substance is injected into the area of the paravertebral level (transverse vertebral processes). |
Blockades are also divided into types according to the point of administration and the drugs used.
The injection can be given:
- into the soft tissues surrounding the painful area of the spine;
- into biologically active segments of the muscular and ligamentous apparatus, as well as into tendons and active skin points;
- into nerve fibers;
- into nerve plexuses and nodules.
Depending on the drug used, injections are divided into:
- therapeutic (with the administration of a treatment drug, such as steroids);
- lidocaine (pain relief);
- novocaine (pain relief, diagnostics).
Injectable medications
Compositions for blockade injections are most often multicomponent. The main elements they contain are lidocaine and novocaine. These drugs are able to interrupt the process of nerve impulse transmission by inhibiting sodium passage.
Is it possible to use local anesthesia during dental treatment while breastfeeding?
In fact, it is not worth neglecting “dental” problems, leaving their solution until the end of lactation. Because even seemingly harmless symptoms may indicate an inflammatory process or caries, untimely treatment of which can lead to serious complications, including tooth extraction.
To prevent this, a woman should consult a dentist as soon as possible at the first discomfort in the oral cavity.
IMPORTANT. At the very beginning of the appointment, you should definitely warn the doctor that the woman is breastfeeding.
One of the biggest fears among breastfeeding mothers is the use of anesthesia during dental treatment. In fact, the need for its use is largely exaggerated and is subject to discussion with the doctor in each specific case. By examining the oral cavity, the dentist will identify problems and indicate the likelihood of solving them without anesthesia. Indeed, sometimes for successful tooth treatment it is enough to endure the painful sensations for only a few seconds.
However, some procedures require the use of local anesthesia:
- opening of canals;
- tooth extraction;
- cyst cleaning;
- installation of pins.
In this case, it is important to find out from the dentist how quickly treatment is needed, and whether it can be postponed until breastfeeding is completed. If the problem requires an immediate solution, and the doctor insists on using local anesthesia, you should not refuse.
Sometimes after treatment or removal, the dentist prescribes a course of antibiotics. In this case, it would be useful to remind the doctor once again that the woman is breastfeeding, so that the doctor can select a drug that is most compatible with lactation. If this is not possible, while taking antibiotics, the baby should be fed pre-expressed (frozen) milk, and the mother herself should continuously maintain its production through regular expression.
IMPORTANT. Delaying treatment only aggravates dental problems, and chronic toothaches can provoke psycho-emotional stress, which has a detrimental effect on the production of breast milk.