The formula will help determine the condition of the mouth
To determine the condition of the oral cavity in medicine, there are about 80 different hygiene indices, based on the principle of staining the enamel with a special solution and identifying dental plaque.
According to the parameters they define, indices can be classified into 4 groups, assessing:
- area affected by plaque;
- thickness of plaque on teeth;
- mass of plaque;
- other parameters of dental plaque (chemical, physical and microbiological).
Fedorov-Volodkina hygienic index
To assess a person’s independent oral hygiene, they use this index. It is best suited for children under six years of age. To calculate the index, the surface of six teeth from the lips is examined. A special composition paints the enamel, allowing plaque to be found. The probe allows you to detect stone formations of various types. To calculate the index, you need to add up all the resulting numbers and divide by the number of surfaces examined. Then they are folded.
Fedorov-Volodkina hygienic index
CPU in dentistry
Dentists should use these calculations during the initial examination of the patient. So, for example, the average values of the indices KPU, kp. KPU+KP of teeth and cavities in dentistry allows you to determine the intensity of carious lesions. These abbreviations contain the following meanings:
- K – carious permanent teeth;
- P – permanent teeth in which a filling is installed;
- U – extracted molars;
- j – temporary teeth affected by caries;
- p – filled temporary teeth.
- According to the World Health Organization, the average CP index for children 12 years old should be from 2.7 to 4.4, and for citizens aged 35-44 years 6.3-12.7.
Assessing the condition of the gums using clinical methods
The periodontal index allows you to assess the health of the gums and bone tissue of the alveoli. It is placed on each tooth separately. Special indicators are used: for gum pathological processes they are relatively low, for pathologies of the tooth alveoli - vice versa. The data for an individual tooth is added together. Then the number must be divided by how many teeth there are in the mouth. The data obtained allow us to talk about the course of periodontal diseases. Causes of diseases and types are not taken into account.
Periodontal index
Simplified index (IGR-U)
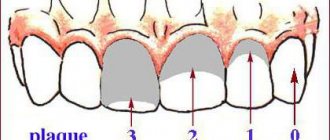
The Green Vermillion Hygiene Index measures plaque and tartar on the surfaces of the 2 upper first molars, 2 lower first molars and 2 upper incisors.
Ratings are given as follows:
- 0 – no plaque;
- 1 – no more than 1/3 of the tooth surface is covered with plaque;
- 2 – plaque affects from 1/3 to 2/3 of the tooth;
- 3 – dental plaque covers more than 2/3 of the surface.
The simplified hygienic index is calculated by adding the plaque index and tartar index on 6 teeth.
Silness-Lohe method
In periodontics, preference is often given to the Silness-Lohe technique, which is based on determining the amount of soft plaque in the gingival zone. The essence of the method is simple: the dentist runs the end of the probe along the neck of the tooth, capturing the gingival groove. If the instrument does not capture plaque at all, a score of 0 is given. If the amount of plaque is small - 1. If a thin layer of plaque is noticeable near the neck of the tooth, and a significant amount is retained on the probe - 2. If a large amount of plaque and food is visually determined in the area where the gum adjoins the tooth. residues - Z. The indicators of all teeth are added up, the result is divided by the number of teeth.
Up to contents
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
PMA – papillary-alveolar-marginal index
When calculating the PMA index, a solution of iodine or Lugol is used, which is applied to the gums and the degree of tissue inflammation is determined by the reaction to the irritant.
The evaluation criteria are:
- 1 – if the papilla (P) is inflamed;
- 2 – in case of inflammation of the marginal edge (M);
- 3 – inflammation of the alveolar part of the gum (A).
Formula RMA = Sum of points/n*3 (in percentage), where n is the number of teeth (up to 6 years – 20 teeth; 6–12 years – 24 teeth; 12-14 years – 28 teeth; over 15 years – 30 teeth) .
If the value is less than 30%, then the degree of damage is mild, 31-60% is moderate, 61% or more is severe.
Iodine index of enamel remineralization.
The active permeability of iodine in tooth tissue is known. Remineralization index (RI), which characterizes the effectiveness of the remineralization therapy used. It is assessed using a four-point system:
1 point – no staining of the tooth area;
2 points - light yellow coloration of the tooth area;
3 points - light brown or yellow staining of the tooth area;
4 points - dark brown staining of the tooth area.
The calculation is carried out according to the formula:
IR = IRNP x number of teeth with hypersensitivity / n,
where IR is the remineralization index;
RRI—remineralization index of one non-carious lesion;
n is the number of teeth being examined.
Dark brown and light brown staining indicates demineralization of the tooth area with non-carious lesions; light yellow - indicates a certain level of remineralization processes in this area of the tooth, and the absence of staining or its slightly yellow color demonstrates a good level of the remineralization process of a particular non-carious tooth lesion.
Php Index
Scientists Podszadlej and Haley developed an oral hygiene performance index. First, a dye solution is applied to the teeth, then the patient rinses his mouth with water, and 6 teeth are examined. In this case, their surface is divided into 5 sections: medial, distal, mid-occlusal, central, mid-cervical. The absence of staining is determined by zero, and the presence - by one.
When calculating, use the formula: IG = ZN/n, where ZN is the sum of codes for all teeth; n – number of teeth examined. With a value of 0, the condition of the oral cavity is considered excellent, and with a value of 1.7 or more, it is considered unsatisfactory.
Indices used in dental examination
The prevalence of caries is expressed as a percentage. To do this, the number of people who were found to have certain manifestations of dental caries (except for focal demineralization) is divided by the total number of people examined in this group and multiplied by 100.
In order to assess the prevalence of dental caries in a particular region or compare the value of this indicator in different regions, the following assessment criteria for the level of prevalence among 12-year-old children are used:
Intensity level
LOW - 0-30% MEDIUM - 31 - 80% HIGH - 81 - 100%
To assess the intensity of dental caries, the following indices are used:
a) intensity of caries of temporary (baby) teeth: index kp (z) - the sum of teeth affected by untreated caries and filled in one individual;
index kp (n) - the sum of surfaces affected by untreated caries and filled in one individual;
In order to calculate the average value of the indices kp(z) and kp(p) in a group of subjects, one should determine the index for each person examined, add up all the values and divide the resulting amount by the number of people in the group.
b) intensity of caries of permanent teeth:
index KPU(z) - the sum of carious, filled and extracted teeth in one individual;
index KPU (n) - the sum of all surfaces of the teeth on which caries or a filling is diagnosed in one individual. (If a tooth is removed, then in this index it is considered 5 surfaces).
When determining these indices, early forms of dental caries in the form of white and pigmented spots are not taken into account. In order to calculate the average value of indices for a group, you should find the sum of individual indices and divide it by the number of people examined in this group.
c) assessment of the intensity of dental caries among the population. To compare the intensity of dental caries between different regions or countries, the average values of the KPU index are used.
WHO distinguishes 5 levels of intensity of dental caries:
Periodontal indices. CPITN Index
To assess the prevalence and intensity of periodontal diseases, almost all countries use the index of need for the treatment of periodontal diseases - CPITN . This index was proposed by specialists of the WHO working group to assess the condition of periodontal tissues during epidemiological surveys of the population. Currently, the scope of the index has expanded, and it is used to plan and evaluate the effectiveness of prevention programs, as well as calculate the required number of dental personnel. In addition, the CPITN index is currently used in clinical practice to examine and monitor the periodontal condition of individual patients. In this regard, the CPITN index can be considered a screening test at both the population and individual levels. This index registers only those clinical signs that may undergo reverse development: inflammatory changes in the gums, which are judged by bleeding, tartar. The index does not record irreversible changes (gingival recession, tooth mobility, loss of epithelial attachment), does not indicate the activity of the process and cannot be used to plan specific clinical treatment in patients with developed periodontitis. The main advantages of the CPITN index are the simplicity and speed of its determination, information content and the ability to compare results. To determine the CPITN index, the dentition is conventionally divided into 6 parts (sextants), including the following teeth: 17/14 13/23 24/27 34/37 43/33 47/44.
The periodontium is examined in each sextant, and for epidemiological purposes only in the area of the so-called “index” teeth. When using the index for clinical practice, the periodontium is examined in the area of all teeth and the most severe lesion is identified. It should be remembered that a sextant is examined if it contains two or more teeth that cannot be removed. If only one tooth remains in the sextant, it is included in the adjacent sextant, and this sextant is excluded from the examination. In the adult population, starting from 20 years of age and older, 10 index teeth are examined, which are identified as the most informative: 17/16 11 26/27 47/46 31 36/37.
When examining each pair of molars, only one code characterizing the worst condition is taken into account and recorded. For persons under 20 years of age, 6 index teeth are examined during an epidemiological survey: 16, 11, 26, 36, 31, 46
CODE 1 : bleeding observed during or after probing. Note: bleeding may appear immediately or after 10-30 seconds. after probing. CODE 2 : tartar or other plaque-retaining factors (overhanging edges of fillings, etc.) are visible or felt during probing. CODE 3 : pathological pocket 4 or 5 mm (the edge of the gum is in the black area of the probe or the 3.5 mm mark is hidden). CODE 4 : pathological pocket 6 mm deep or more (with the 5.5 mm mark or black area of the probe hidden in the pocket). CODE X : When only one or no teeth are present in the sextant (third molars are excluded unless they are in place of second molars).
To determine the need for periodontal disease treatment, population groups or individual patients can be categorized based on the following criteria. 0: CODE 0 (healthy) or X (excluded) for all 6 sextants means that there is no need for treatment for this patient. 1: A CODE of 1 or higher indicates that this patient needs to improve his oral hygiene status. 2: a) CODE 2 or higher indicates the need for professional hygiene and the elimination of factors that contribute to plaque retention. In addition, the patient needs training in oral hygiene. b) CODE 3 indicates the need for oral hygiene and curettage, which usually reduces inflammation and reduces pocket depth to values equal to or less than 3 mm. 3: Sextant with CODE 4 can sometimes be successfully treated with deep curettage and adequate oral hygiene. In other cases, this treatment does not help, and then complex treatment is required, which includes deep curettage. The prevalence and intensity of periodontal disease in the population is assessed based on the results of a survey of 15-year-old adolescents.
Gingivitis Index (GIA)
To assess the severity of gingivitis (and subsequently record the dynamics of the process), the papillary-marginal-alveolar index (PMA) . Various modifications of this index have been proposed, but in practice the PMA index as modified by Parma (1960) is more often used.
The RMA index is assessed using the following codes and criteria:
0—no inflammation; 1 - inflammation of only the gingival papilla (P); 2 - inflammation of the marginal gum (M); 3 - inflammation of the alveolar gum (A).
The PMA index is calculated using the formula: sum of PMA = ———————- x 100% 3 x number of teeth The number of teeth (while maintaining the integrity of the dentition) is taken into account depending on age: 6 – 11 years – 24 teeth, 12 – 14 years - 28 teeth, 15 years and older - 30 teeth.
Note: if there are missing teeth, then divide by the number of teeth present in the oral cavity. Normally, the PMA index is 0. The higher the digital value of the index, the higher the intensity of gingivitis.
Evaluation criteria for the RMA index:
30% or less - mild gingivitis; 31-60% - moderate severity; 61% and above—severe degree.
Oral hygiene assessment
Fedorov-Volodkina hygienic index (1971)
The index is recommended to be used to assess the hygienic state of the oral cavity in children under 5-6 years of age. To determine the index, the labial surface of six teeth is examined: 43, 42, 41, 31, 32, 33. These teeth are stained using special solutions (Schiller-Pisarev, fuchsin, erythrosine) and the presence of plaque is assessed using the following codes: 1 - plaque not identified; 2 - staining one quarter of the surface of the tooth crown; 3 - staining half the surface of the tooth crown; 4 - staining three quarters of the surface of the tooth crown; 5 - staining the entire surface of the tooth crown. Determination of supra- and subgingival tartar is carried out using a dental probe.
Codes and criteria for assessing dental calculus
O —tartar is not detected; 1 - supragingival tartar, covering no more than 1/3 of the tooth surface; 2 - supragingival tartar, covering more than 1/3, but less than 2/3 of the tooth surface, or the presence of individual deposits of subgingival tartar in the cervical area of the tooth; 3 - supragingival calculus covering more than 2/3 of the tooth surface, or significant deposits of subgingival calculus around the cervical area of the tooth.
The calculation of the index consists of the values obtained for each component of the index, divided by the number of surfaces surveyed, followed by the summation of both values.
Formula for calculation:
IGR-U stone values = ———————————- + ——————————— quantity. number of surfaces surfaces
Evaluation criteria
a) IGR-U values: Level of oral hygiene 0, 0 - 1, 2 good 1, 3 - 3, 0 satisfactory 3, 1 - 6, 0 poor
b) Values of plaque or tartar indicators: 0.0 - 0.6 good 0.7 - 1.8 satisfactory 1.9 - 3.0 bad
Oral Hygiene Performance Index (OHP) Podshadley, Haley, (1968)
To quantitatively assess dental plaque, 6 teeth are stained: 16, 26, 11, 31—vestibular surfaces; 36, 46 - lingual surfaces.
1 - medial 2 - distal 3 - mid-cervical 4 - central 5 - mid-occlusal
Codes and criteria for assessing dental plaque
O - no staining 1 - staining detected
The index is calculated by determining the code for each tooth by adding the codes for each section. Then the codes for all examined teeth are summed up and the resulting sum is divided by the number of teeth:
The index is calculated using the following formula:
sum of codes of all teeth RNR = —————————————————— number of teeth examined
Evaluation criteria
Index value Hygiene level 0 excellent 0.1 - 0.6 good 0.7 - 1.6 satisfactory 1.7 or more unsatisfactory
Dental aesthetic index NC Cons et al., (1986)
A special dental aesthetic index is used to assess the condition of the bite. In the clinic, the index is used at the individual level and when conducting epidemiological surveys of the population. This index determines the position of the teeth and the state of the bite in the sagittal, vertical and transversal directions. Recommended for use from 12 years of age in key age groups. The examination is carried out visually and using a button probe. The index includes the definition of the following components: • lack of teeth; • crowding in the incisal segments; • gap in the incisal segments; • diastema; • deviations in the anterior part of the upper jaw; • deviations in the anterior region of the lower jaw; • anterior maxillary overlap; • anterior mandibular overlap; • vertical front gap; • anteroposterior relationship of molars. Lack of teeth. The number of incisors, canines and premolars on the upper and lower jaws is counted (from 15 to 25 and from 35 to 45) and the number of missing teeth in this group is determined.
Teeth are not considered removed if: 1. with a missing tooth, the space is closed; 2. the baby tooth is in the dentition, but the permanent tooth has not yet erupted; 3. The space is restored with a bridge. Crowding in the incisal segments. Each segment consists of 4 incisors. Crowding is a condition of the dental arches when the space between the right and left canines is not enough to accommodate all 4 incisors in a normal position. The teeth may be rotated or out of line with the arch.
Codes and evaluation criteria
O - no crowding 1 - crowding of one segment 2 - crowding of two segments
Spacing in incisal segments. Gap is a condition where the space located between the right and left canine teeth is greater than the space required to accommodate all 4 incisors in their normal position. If one of the incisors has proximal surfaces without interproximal contact, the segment is considered to have a spacing. If the bite is mixed, you should not consider the space from a recently fallen temporary tooth to be empty if it is obvious that the permanent tooth will erupt soon.
Codes and criteria:
O - no gap in segment 1 - one segment with a gap 2 - two segments with a gap. If in doubt, evaluate to a lower score. Diastema is the space between the two permanent upper central incisors. Measurements are taken with a button probe at any level between the mesial surfaces of the teeth and expressed in mm.
The largest deviation between adjacent teeth is measured. To do this, the tip of a button probe is placed on the labial surface of the tooth most deviated in the lingual direction or rotated around its axis at an angle of 90° to the normal line of the dental arch. Registered in mm. Anterior maxillary overlap. The measurement is carried out in central occlusion. The working part of the periodontal probe is placed parallel to the occlusal plane and the distance (in mm) from the labial-incisal edge of the most protruding upper incisor in relation to the labial surface of the lower incisor projected onto it is assessed. This index component is not taken into account if all the upper incisors are missing and/or in a lingual position (crossbite). If the incisors close to the edge, then you can put code 0. Anterior mandibular overlap. This sign is assessed when either lower incisor is advanced anteriorly or vestibular to the opposing upper incisor. The greatest forward movement of the tooth (in mm) is recorded. Measurements are carried out in the same way as on the upper jaw.
If there is no occlusion on the first molars due to the absence of one or two teeth, incomplete eruption or disruption of their shape due to caries or filling, then the relationship of the canines or premolars is determined.
Codes and criteria:
O - norm 1 - displacement by 1/2 of the tuberosity mesially or distally in relation to the norm 2 - displacement by the size of the tuberosity mesially or distally in relation to the norm.
The dental aesthetic index allows you to analyze each of the components of the index or group them by anomalies of the dentition and bite.
CPITN (periodontal disease treatment need index)
This method covers 10 teeth, allowing the dentist to see the condition of the gums of the upper and lower jaws. Grades are given as follows:
- 0 – no disease symptoms;
- 1 – gums are bleeding;
- 2 – tartar was found above and below the gum;
- 3 – gum pocket 4-5 mm deep;
- 4 – gum pocket more than 6 mm.
It may come as a surprise to many that the condition of teeth can be determined using a formula, but this is the truth. Therefore, do not neglect maintaining oral hygiene, so as not to be a poor student in this calculation.
The iOrtho clinic network provides high-quality services for correcting malocclusion with Invisalign aligners, sign up for a consultation now!
Assessment of plaque deposits in young children
Characteristics are given to absolutely all children's teeth. The procedure can be done from the moment the first teeth appear up to three years. You can make an assessment “by eye” or using tools.
Even if there are few teeth in the baby's mouth, an analysis should be carried out.
Criteria:
- 0 – no plaque;
- 1 – there is plaque.
Assessment of plaque deposits in young children
General overview
Periodontal indices are a quantitative (in percentage or coefficients) expression of pathological processes occurring in the periodontium.
In comparison with clinical diagnostic methods, the index assessment is relative and does not claim absolute accuracy.
However, it has a number of advantages that clinical diagnostics lack. With its help it is convenient:
- conduct epidemiological studies for any segment of the population;
- monitor the dynamics of pathological processes;
- compare the results of different studies;
- evaluate the effectiveness of treatment and prevention.
Evaluation of indicators
To determine the degree of caries infection, doctors use three indicators. To determine them, the total number of people with a given problem is divided by the total number of patients examined and multiplied by 100.
To compare regions in terms of oral health, they resort to assessing this criterion in adolescents aged 12 years.
| Prevalence | Index |
| up to 30% | short |
| up to 80% | average |
| up to 100% | high |
The intensity of infection is determined from the number of dental elements affected by caries. Based on the KPU indicators, 5 degrees are distinguished:
| Index | Intensity levels |
| Children | |
| up to 1.1 | very low |
| up to 2.5 | low |
| up to 4.5 | moderate |
| up to 6.5 | high |
| more than 6.5 | very high |
| Adults | |
| less than 1.5 | quite low |
| up to 6.2 | low |
| up to 12.6 | moderate |
| up to 16.3 | high |
| more than 16.4 | very high |
These studies allow us to study the state of health and develop an individual treatment plan for each patient individually.
An increase in the incidence of a disease is determined by the same patient over a certain period of time. The change in value during inspection is the intensity.
WHO survey
Epidemiology is a special branch of medicine that studies the nature of the manifestation and spread of pathologies among various segments of the population. It is also applicable in dentistry.
Epidemiological research takes place in 3 stages:
- Preparatory. Planning is done for upcoming research, defining objectives, methods and research dates.
The place of execution and the necessary equipment for this are being prepared. A group of junior medical staff and trained doctors is being created.Population groups differing from each other in living conditions are identified, with an equal number of men and women.
- Examination. A registration card is created in which the research data will be entered (for children and adolescents under 15 years of age its form is simplified).
It is prohibited to make corrections or additions to this document. All entries are recorded in coding, with each code indicating a specific symptom or its absence.To obtain an accurate picture of health, information about the extraoral zone and mucous membrane is also taken.
- Evaluation of the results obtained. Data is calculated - the degree of prevalence of caries, the threshold for the incidence of periodontitis, etc. The result is displayed as a percentage.
Such an examination helps to analyze the dental situation in a certain region, find out the dependence of oral health on social class or environmental living conditions, and track the degree of change in these data with a person’s age.
It is important to determine the most common diseases, their intensity by region and age. Based on the results obtained, preventive actions are developed and hygiene training is provided.
The video provides additional information on the topic of the article.
How is the procedure performed?
The essence of the Schiller-Pisarev test is to lubricate the gums with a solution of iodine and potassium. As a result, areas with deep connective tissue lesions become stained - this is due to the accumulation of large volumes of glycogen in areas of inflammation. The tests are repeated from time to time - if the treatment is carried out correctly, the condition of the gums will improve, and the inflammation will subside or disappear altogether. That is, if the therapy is correct, then repeated tests should be weakly positive or negative.
Gum staining is due to the high amount of glycogen. When the inflammation passes, there is less glycogen, and the tissues cease to be intensely stained. In this way, the intensity and degree of development of the disease is determined.
Composition of the solution
To take Schiller-Pisarev samples, the composition of the solution is used in the following proportions:
- crystalline iodine – 1.0;
- potassium iodide – 2.0;
- distilled water – 40.0.
Before using therapeutic and prophylactic toothpaste (Parodontax, Parodontol paste), the gum mucosa is lubricated with a special solution, then the degree of staining is determined, and the data obtained is recorded in the disease history. Control – after 1, 2, 3, 6 and 12 months.
conclusions
The listed periodontal indices contain information about the hygienic situation in the oral cavity, the intensity of the spread of inflammation and the destructive process in the periodontium.
The examinations are simple to perform, do not cause pain to the person, and do not require the doctor to undergo special training.
They help to assess the general condition of periodontal tissues and formulate conclusions about the effectiveness of therapeutic and preventive measures.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags gums periodontal indices
Did you like the article? stay tuned
Mouth rinse
Many patients ask: “What should I rinse my mouth with?” If your gums are inflamed, you can use antimicrobial (antiseptic) and anti-inflammatory agents. Antiseptic drugs act on pathogenic bacteria that cause suppuration. Anti-inflammatory drugs have virtually no effect on viruses, but they can slow down the development of the disease.
So what should you rinse your mouth with if your gums are inflamed? Doctors recommend:
- For periodontitis or gingivitis, use both types of products, although antimicrobial ones will be more effective.
- When the socket of an extracted tooth becomes inflamed, antiseptic agents, for example, Chlorhexidine, should be used.
If you always wash your hands before eating and brush your teeth and tongue afterward, you will have a sparkling smile for many years to come.
Advantages and disadvantages
An important component of implantation at all stages is an accurate index assessment of the condition of peri-implant tissues, implants and supported prostheses. The Schiller-Pisarev test is quite effective and allows you to diagnose a wide range of conditions - gum inflammation, periodontal destruction, the amount of tartar, plaque, the need for certain therapeutic measures and their volume.
The relationship between the elements of the implant and adjacent tissues and its difference from a natural tooth may make complex periodontal studies impossible.
The Schiller-Pisarev test is quite accurate and objective and has two interpretation options. The first is visual, based on the nature of the gum staining, the second is numerical, that is, index. The main problem of the technique is that dental indices from 30-50 years ago do not meet the current needs of modern implantology.
That is, they can be used, but when interpreting the results, it will be necessary to take into account the full list of current changes and improvements in the field of prosthetics. At the same time, it is the Schiller-Pisarev test that is considered the most informative of all similar diagnostic methods and allows the results to be most successfully adapted to the conditions of endosseous implantation. However, the convention of numerical values still does not disappear anywhere, since diagnostics are carried out using markers, and not high-precision digital equipment. Modern researchers say that the Schiller-Miller test is still relevant, but should be used with certain modifications and clarifications.
Papillary bleeding (PBI) according to Saxer and Miihiemann
The periodontal bpe index (PBI) is needed to determine the degree of gum inflammation. A probe is used to make a groove along the interdental papillae and observe for 30 seconds.
The severity of gingivitis is 4 points:
- 0 – no blood;
- 1 – appearance of only blood spots;
- 2 – pinpoint blood appearances along the line of the furrow;
- 3 – blood fills the triangle between the teeth.
- 4 – intense bleeding.
The study of the papillae - PapillaBleeding - is carried out in the following quadrants: the gums of the 1st and 3rd quadrants from the lingual surface and the 2nd and 4th quadrants - from the vestibular side (the vestibular side is the vertical wall of the tooth from the lips and cheeks). First, each quadrant is counted, then the arithmetic mean is derived.
Observation of children
By calculating the Green-Vermilion index, doctors can create dispensary groups for monitoring children:
- Group 1 – children who have no pathologies;
- Group 2 – actually healthy babies with a history of any chronic or acute disease that does not affect the function of the most important organs;
- Group 3 – children with chronic illnesses with a balanced, sub- and decompensated course.
There are three phases in the dental examination of children:
- In the first phase of the examination, each child is individually recorded, an additional examination is carried out in the hospital, then an outpatient observation group is determined, the endurance of each child is assessed and the order of examinations is determined.
- In the second, a contingent is formed according to supervision groups, uniform conditions for phasing and continuity of study are assigned, dispensary patients are proportionally divided between doctors, and the needs of the examined contingents in inpatient and outpatient treatment are met.
- In the third, doctors determine the frequency and nature of active supervision of each child, adjust diagnostic and treatment measures in accordance with changes in health status, and evaluate the effectiveness of supervision.
Of great importance is the organization of educational work to prevent dental diseases in children and create motivation to care for newly emerging teeth.
Cliche
The calculation formula is attached as follows:
IGR-u = sum of plaque values/number of planes + sum of stone values/number of surfaces.
The interpretation of the index (the IGR value at the level of medicine) is proposed as follows:
- 0.0-1.2 - flawless;
- 1.3-3.0 – acceptable;
- 3.1-6.0 – low.
The Green-Vermilion index has the following values for dental plaque standards:
- 0.0-0.6 – impeccable;
- 0.7-1.8 – tolerable;
- 1.9-3.0 – bad.