Implantation, the most successful and effective method of restoring a natural smile, is constantly being improved, as is dental treatment in general. Patients are offered innovative techniques that provide better results or reduce the duration and cost of treatment. One of the major achievements in recent years has been the barrier membrane, which is installed in conditions of bone tissue deficiency.
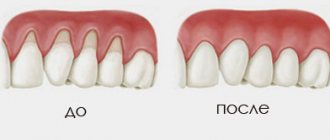
Alveolar ridge atrophy is almost inevitable in people who require implantation. Some people delay therapy for a long time, which is why the bone has time to dissolve, while others have congenital structural features of the jaw apparatus. In any case, performing dental implantation in the event of atrophic phenomena in the bone tissue becomes impossible. Such an error threatens the following adverse consequences:
- Loosening, retraction or even loss of the implant (sometimes its loss is quite traumatic, involving the patient’s bone tissue);
- Impossibility of performing bone grafting in the future due to excessive thinning of the bone (any intervention risks fractures).
Moreover, jaw bone resorption is so seriously detrimental to the patient that even without implantation, bone grafting remains a necessary surgical procedure.
Gradually progressive atrophy leads to the fact that the face becomes asymmetrical and ugly: wrinkles worsen, the functioning of facial muscles is disrupted, and so on. The chewing function of the jaws is significantly affected, which is why patients eat poorly and have problems with the gastrointestinal tract. In advanced situations, speech and swallowing are noticeably impaired, and breathing movements are less likely to suffer. Therefore, bone grafting with additional installation of a barrier membrane must be performed immediately after the problem is detected.
Bone grafting is a solution to the problem of atrophy
For quite a long time, bone grafting has been recognized as the most effective method of restoring the width and height of the alveolar process. The technique is constantly modified and becomes safer and less traumatic. In addition, dentists are trying to achieve conditions under which simultaneous implantation will be possible.
There are several basic bone grafting techniques:
- Sinus lift. Restoration of bone volume in the upper jaw in the area of the projection of the bottom of the maxillary sinus. The operation is performed more often than others, since it is here that bone resorption is predominantly observed. The essence of the surgical intervention is that the dentist, in one of the ways (closed or open), gains access to the mucous membrane of the maxillary sinus. He disconnects part of the membrane from the periosteum, and fills the resulting cavity with prepared material of natural or synthetic origin.
- Splitting of the alveolar ridge. An effective technique for correcting the width of any jaw. First, the alveolar ridge is cut and spread apart, after which the graft is placed inside. The advantage of the technique is that the structure is immersed in the spongy tissue of the jaw, where regeneration and replenishment of the bone block is actively taking place. That is why the use of expensive osteoplastic materials is not required here.
- Guided tissue regeneration. This type of bone grafting includes two components: a graft and a collagen membrane. These two components, interacting with each other, help restore the deficit of both the width and height of the alveolar process in any part of the jaws. The technique is rarely used with simultaneous implantation.
- Bone block grafting. This technique involves the use of a natural, preferably autogenous, graft, which is placed on the area where implantation is planned and where the bone tissue has atrophied. The disadvantage of this technique is that the graft is connected to an area of the bone where there are no blood vessels. Engraftment in such conditions occurs slowly.
Patients tend to be afraid of bone grafting, since it is a full-fledged surgical intervention on the teeth. However, all manipulations are carried out under local or general anesthesia, so they do not cause any discomfort. The risk of complications with this manipulation is minimal, and the benefits are undeniable. Even if the atrophy of the alveolar process does not allow immediate implantation, and patients have to wait six months for the implants to take root, it is still better to give preference to bone grafting rather than alternative methods of tooth restoration. Moreover, in modern conditions there are many designs that increase the benefit and effectiveness of bone grafting, for example, fixation of a barrier membrane.
The success of patient rehabilitation after dental implantation is determined by the sufficient amount of bone tissue in the implantation site.
Filling bone defects with bone substitutes is the procedure of choice for bone maintenance, but ingrowth of connective tissue from the mucosa can disrupt the process of fusion of the bone substitute to the walls of the defects.
The use of a dental membrane as a barrier is indicated in the scientific literature as the most acceptable solution to this problem.
Guided bone regeneration (GBR) is a technique that is based on the concept of separating bone from soft tissue, that is, preventing apical migration of gingival epithelium and connective tissue within the defect with a membrane as a barrier. The use of a membrane promotes the proliferation of cells capable of regeneration and their differentiation into the desired tissue type.
For directed bone regeneration, five conditions are necessary:
- Use of an appropriate membrane;
- Achieving primary healing of soft tissues;
- Creation and maintenance of an area protected by a membrane;
- Adaptation and stabilization of the membrane with the surrounding bone;
- Quite a long healing period.
According to Hardwick et al., the main purpose of the membrane is to create suitable conditions under which the natural biological potential for functional regeneration is maximized.
Properties and types of membranes for dentistry
Creating and pre-preparing the site where the blood clot is located, preventing inflammation that may result from bacterial penetration, isolating the regeneration space from unwanted tissue, and ensuring mechanical stability and compactness of the organized coagulate are just a few of the factors for successful bone regeneration.
It is worth mentioning their role in preventing the penetration of epithelial cells into the bone material, as well as in enhancing the fixation of the bone substitute used.
Mandatory properties of a membrane for dentistry:
- Full biological compatibility;
- Barrier activity (prevention of soft tissue proliferation);
- Ensuring appropriate integration of surrounding tissues;
- The ability to preserve a site for the growth of new alveolar bone;
- Immunological inertia;
- Easy to use.
The membrane must resist chewing forces and reduce tissue tension.
In this case, the ability of the membrane to integrate with the preservation of surrounding tissues and effectively suppress epithelial migration is critical.
Based on clinical and histological studies of various barrier materials, no one has been shown to be ideal for every clinical situation. Each material has certain characteristics, advantages and limitations.
Depending on the response to their biological environment, membranes can be grouped as non-resorbable and resorbable.
Non-resorbable membranes for dentistry
retain structure and shape in the tissues, and to remove them it is necessary to perform another operation; this increases trauma, prolongs wound healing, and increases the cost and duration of the entire treatment.
Resorbable membranes
does not need to be removed after placement, which significantly improves practicality and optimizes treatment costs as well as the risk of surgical complications.
Due to the nature of resorbable membranes, it is impossible to accurately determine the duration of their destruction. The degradation process begins immediately after placement.
Data from the literature regarding the desired duration of membrane persistence in vivo indicate that it varies from 4 weeks to several months.
Due to biological degradation, resorbable membranes cause tissue reactions that can negatively affect wound healing and impair regeneration.
An ideal bioresorbable membrane for guided bone regeneration has the following characteristics:
- Biocompatibility;
- Lack of inflammatory response;
- Complete resorption, degradation and elimination;
- High technological effectiveness of the material;
- Optimal resorption time.
Such a dental membrane should be easy to handle, including delineating the shape of the defect and maintaining the required shape and configuration. It must be simply and reliably fixed, and be resistant to bacterial adhesion and colonization.
The most important requirement for membranes is the resorption time, which must correspond to the formation of new bone tissue.
Two materials are used to produce resorbable membranes: synthetic aliphatic polyester and collagen from various animal sources, including bovine tendon, bovine dermis, calf skin or porcine dermis.
Collagen membranes for dentistry
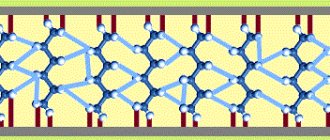
Collagen is an insoluble fibrous protein that is an important natural component of connective tissue.
Collagen's ability to stimulate adhesion, chemotaxis, and physiological degradation of progenitor cells along with its potential for degradation makes it an ideal material for creating membranes for dentistry.
There are at least 16 types of collagen found in interstitial tissues, bone matrix, cartilage, epithelial, blood vessels, and the vitreous body of the eye. Types I, II and III collagen make up 80–90% of the body's collagen.
Collagen products available on the market consist mainly of collagen types I and III.
Collagen is weakly immunogenic, activates hemostasis and can increase tissue thickness. During wound healing, clinically significant interaction of collagen with various cell types occurs.
Collagen is made from animal skin or by-products. The material is first isolated and purified with enzymes and chemicals, then processed in various ways.
The most common chemical modification of collagen forms cross-links, usually by exposure to an aldehyde, which reduces water absorption, affects meltability, degradation rate and stability.
This modified material is called cross-linked collagen.
Collagen membranes are degraded by macrophages and polymorphonuclear neutrophils, and the rate of uptake varies depending on the source and modifications of the collagen.
Resorption of the collagen membrane begins with the action of the enzyme collagenase (matrix metalloproteinase), which divides the collagen molecule at a certain position. The resulting parts are denatured and converted into gelatin, which is then broken down into amino acids by gelatinase and another proteinase.
During enzymatic digestion, it is incorporated into the flap to support the attachment of new connective tissue. This can result in an increased thickness of the flap, which protects and allows for further bone formation.
Collagen Cross-Linking: Pros and Cons
The stability of the structure, increased by cross-linking, slows down the degradation process.
The essence of this process is the creation of various mutual bonds between specific amino acids, as well as between amino acids and carboxylate groups, under the influence of chemical and physical agents.
Cross-linking of collagen is achieved by ultraviolet and gamma radiation, hexamethylene glutaraldehyde, diphenylphosphorylase and ribose.
This treatment reduces the in vivo rate of resorption of collagen material and improves mechanical properties. In the Western scientific world, there is still controversy over whether to use cross-linked or non-cross-linked collagen membranes for NRC.
Many studies have proven that cross-linking prolongs the biodegradation of the collagen membrane and that this shows a positive, although limited, effect on NRC in various types of experimental defect models. Other studies suggest that their use is associated with an initial foreign body reaction and impairs tissue integration and transmembrane vascularization.
Despite all the discrepancies, membrane vascularization has been shown to improve 2 weeks after submucosal implantation in a rat model. This is likely due to the fact that the initial hyperemia in the adjacent tissue drives angiogenesis towards the experimental membrane.
In 2006, Schwarz et al. investigated the angiogenesis model in natural and cross-linked collagen membranes because previous tests showed that vascularization in cross-linked membranes is weaker.
The researchers concluded that the rate of angiogenesis when using different types of membranes does not have statistically significant differences.
In studies conducted by researchers at the Belgrade Military Medical Academy, defects covered with cross-linked collagen membranes showed better levels of vascularization compared to non-cross-linked membranes and empty defects.
In 2012, Thoma et al. studied differences in cross-linked collagen using different degrees of cross-linking material in mouse soft tissue.
Histopathological and histomorphometric analyzes performed 3 and 6 months after the intervention showed that the degree of cross-linking of the material is inversely proportional to tissue integration, the degree of collagen biodegradation and the rate of vessel formation.
Collagen with the lowest degree of cross-linking exhibits better surrounding tissue integration, stability, and angiogenesis.
Despite several negative characteristics, many authors have suggested that the use of cross-linked collagen membranes has many advantages in targeted bone regeneration.
Efficiency of collagen membranes
Some periodontal microorganisms produce collagenase, an enzyme that can lead to premature membrane degradation. These are, in particular, Porphyromonas gingivalis and Bacteroides melaninogenicus.
Bacterial colonization can lead to early degradation of collagen membranes, compromising the procedure. Both cross-linked and non-cross-linked dental membranes are equally susceptible to lysis by bacterial proteases, although cross-linked membranes are somewhat more resistant to proteolysis.
Therapeutic concentrations of antibacterial agents, including chlorhexidine, minocycline, and doxycycline, partially inhibit enzymatic membrane degradation.
Collagen membranes vary in microarchitecture (the space between collagen molecules, fibers, bundles and layers) and cross-linking.
Microarchitecture and cross-linking determine membrane characteristics such as tensile strength, ease of use, flexibility, tissue integration, and biodegradation.
Membranes with a higher degree of cross-linking remain intact for a longer period of time. Research has shown that premature membrane resorption or removal can result in incomplete bone healing, so it is recommended that dental membranes used in NRC have a degradation period of 3 to 9 months for complete bone formation.
Biodegradation of collagen membranes
Rothamel et al. studied the biodegradation over time, tissue response, tissue integration and vascularization of commercially available collagen membranes as well as experimental products using rat models.
Histological and histometric studies were performed at 2, 4, 8, 16 and 24 weeks after membrane placement. It was concluded that cross-linked bovine and porcine type I and type III collagens prolong the biodegradation process but reduce tissue integration and vascularization.
In addition, when using these products in experiments, a foreign body reaction occurs, which is characteristic of cross-linked membranes.
This study highlights these differences between cross-linked and non-cross-linked membranes, proving that non-cross-linked membranes have better vascularization and tissue integration. The rate of absorption directly correlates with the degree of cross-linking - the higher the level of connections, the greater the rate of resorption.
In 2006 and 2008, Tal et al. clinically and histologically studied the duration of membrane barrier function and biointegration in sites that were treated with cross-linked and non-cross-linked collagen membranes.
Particular attention was paid to spontaneous perforations of the mucosa through barrier membranes. It was shown that the cross-linked membranes were more resistant to tissue degradation and that they maintained their integrity for a longer period.
Disadvantages of collagen membranes for dentistry
Compared to non-resorbable membranes, collagen membranes do not have the ability to maintain volume. The use of space-preserving bone graft tends to improve the outcome of guided bone regeneration.
Enlargement of the alveolar bone can be expected if the space under the collagen membrane is created and maintained strictly during the appropriate period while new bone is being formed.
It is therefore advisable to use materials that will provide support to prevent the barrier from collapsing due to the pressure generated by masticatory forces.
Today, dental membranes are commonly used with a variety of bone grafts and fillers. When bioresorbable membranes are used in this combination, the results of NRC are much more favorable, and comparable to non-resorbable membranes.
This is especially true when treating localized horizontal defects.
However, osteoplastic materials themselves are less effective than a combination of an auxiliary material and a barrier. The combination of membranes with bone material helps to achieve good results in the treatment of vertical defects of the alveolar process, since one of the main disadvantages of the collagen membrane is the inability to achieve the vertical height of the bone.
To solve this problem, the mentioned combination was used. The membranes in these cases require additional stabilization using mini-screws.
Effect of membrane thickness on bone regeneration
Until now, not enough studies have been published on the effect of resorbable membrane thickness on bone regeneration.
An attempt to use a thicker membrane was first published in 2005 by Busenlechner et al. The goal of their study was to question the ability of a slowly resorbing prototype three-layer membrane to regenerate bone tissue.
The model was a procedure used to increase the alveolar process after extraction of the first and second molars in the lower jaw of a monkey. Experimental animals were sacrificed after 9 months.
The study results support the use of a slowly absorbing three-layer membrane because the best bone regeneration achieved was achieved with this membrane and bone graft.
The membrane was made by adding a polylactide layer between the collagen layers to increase biodegradation time as well as barrier function.
Fragments of polylactides were detected in histological studies even 9 months after surgery.
Improving the design of the three-layer membrane can be an important step in improving the stability of the membrane at a certain impact rate.
The same prototype three-layer membrane was studied by von Arx et al. Their research looked at a prototype three-layer membrane in combination with various materials.
Differences were analyzed histopathologically and histomorphometrically after four and a half months. The prototype three-layer membrane combined with autograft demonstrated better bone regeneration.
In 2009, Kozlovsky et al. conducted a histological comparison of the biodegradation of Bio-Gide® membrane (a non-crosslinked collagen membrane) that was used in one or two layers with mechanical defects created on the jaws of rats.
Application of a second layer of Bio-Gide® membrane (double-layer technique) resulted in a significant increase in the residual amount of collagen.
There was also more barrier material left in the fabric, indicating that the barrier function of the membranes was longer lasting, and also that a single-layer membrane could not achieve similar barrier function over a longer period of time.
Thus, a two-layer membrane for dentistry significantly improves bone tissue regeneration and does not affect ossification. It should be noted that the second layer helps reduce micro-movements and increases the stability of the material.
Transmembrane vascularization was evident histologically as early as 4 weeks after implantation and became clearly visible across all layers of the membrane by 9 weeks after implantation.
Despite the difference in thickness of the double-membrane preparations, the same degree of degradation of 80% for both membranes was achieved after only 9 weeks.
Since transmembrane blood vessel formation is necessary for collagen resorption, it appears that the vascularization of the bilayer membrane was not impaired by its increased thickness.
It has been argued that increasing the density of cross-links between collagen molecules negatively affects biocompatibility, membrane integration, vascularization, and also inhibits the attachment and proliferation of fibroblasts and osteoblasts.
The use of a second layer of resorbable cross-linked membrane avoids these disadvantages, increasing the durability of the dental membrane.
The effectiveness of double-layer membranes in bone graft applications in terms of bone resorption was analyzed in studies in rabbits.
Bone blocks of the parietal bones were taken from one side and placed on the other, where they were covered with membranes. Histological and histomorphometric analyzes were performed 2, 4 and 6 months after surgery.
The results of the study show that the use of double membranes significantly reduces bone resorption of the graft compared to a single layer.
Another study, conducted by the Belgrade VMA, looked at the effects of collagen membranes of different thicknesses. The results showed that the best results were achieved with thicker dental membranes.
The results of a series of studies regarding membrane thickness show that thicker membranes, whether they are arranged in several layers or a single layer, exhibit a greater barrier function and remain in the tissue longer because they degrade slowly and promote better ossification of the bone defect.
Although the explanation for this finding remains elusive, it is suggested that the significant increase in membrane thickness and durability leads to an increase in angiogenesis and the cellular population of the collagen matrix, causing cell proliferation, differentiation and active ossification.
Collagen membranes of human origin
Particular attention should be paid to the absorbable collagen membrane for human dentistry.
The role of human resorbable demineralized membrane in guided bone regeneration and guided tissue regeneration is not well understood.
A number of European studies examining the influence of the thickness and origin of resorbable membranes on bone regeneration have yielded conflicting results.
Resorbable human demineralized membrane (RHDM) was obtained from cadaveric skull bone by a combination of physical and chemical methods, namely demineralization of cortical bone followed by removal of lipoproteins.
Experiments have shown that RHDM provides a higher rate of bone tissue regeneration compared to other membranes, especially when thicker membranes are used.
Combining growth factors
and membranes for dentistry
Recently, the inclusion of growth factors and differentiation factors in the membrane has attracted keen interest from researchers.
There is ample evidence that certain growth factors and similar mediators can influence the regeneration of many tissues, including bone regeneration.
An example is the development of combination membranes that can control the release of transforming growth factor (TGF-β).
Local delivery of a wide range of growth factors, such as platelet-derived growth factors (PDGFs) and bone morphogenetic proteins, which are osteoinductive growth factors, has already been successfully used in dentistry.
These substances have the ability to further stimulate cell migration, proliferation and differentiation. Numerous in vitro, animal and human studies have demonstrated the benefits of these factors in combination with collagen membranes.
Such innovations could lead to major changes in the results of guided bone regeneration without significant additional costs.
Conclusion
This article reviews the basic principles of using dental membranes in guided bone regeneration.
Significant progress has been made since the original non-resorbable polytetrafluoroethylene (e-PTFE) membrane was used.
Synthetic and natural biomaterials have been used in dental practice with great clinical success for more than 20 years; their mechanical properties and biodegradation rates are constantly being improved.
It is expected that the next generation of membranes will contain new functional molecules that improve the results of targeted bone regeneration.
What are barrier membranes?
The barrier membrane is one of the most modern and successful inventions in dental practice. Such designs are actively used in almost all surgical interventions. Barrier membranes for bone grafting during implantation can prevent atrophic phenomena in the alveolar process and contribute to the immediate successful fixation of artificial roots. The membrane affects the regenerative abilities of the bone, increasing them, does not allow osteoclasts that are dangerous to bone cells to enter, and minimizes the risk of penetration of pathogenic agents. Thanks to the barrier membrane, graft engraftment is accelerated, as is the overall treatment of the patient.
The membrane for bone grafting is a very thin and fairly elastic plate that is attached to the bone with titanium pins. In this way, the gums are separated from the bone material during the formation of natural jaw tissue.
Types of membranes
There are two types of barrier membranes that are widely used in dentistry:
- Resorbable. This structure gradually dissolves. It does not require separate removal, that is, additional surgical intervention, which means it causes less trauma.
- Non-resorbable. Membranes of this type do not dissolve on their own, which is why patients need an additional stage of treatment - removal of the structure. In most cases they are made of titanium. Such membranes are attached in the presence of a serious deficiency of bone tissue, filled with granules of osteogenic material. Once the alveolar bone and soft gum tissue have recovered, the barrier membrane is removed.
The dentist independently selects the optimal membrane for a specific clinical case. He must take into account that resorbable structures do not fix the grafts well enough, so they are used only for minor atrophies.
Types of resorbable membranes
Resorbable membranes are called absorbable membranes, for the production of which the following materials are used.
- Polymers that can retain their properties for several months. Their advantages include a low risk of developing allergies and inflammation.
- Material of animal origin, characterized by high biocompatibility with human jaw tissue. Such membranes are used less frequently, as they can cause allergies.
Before installing barrier membranes, the patient undergoes a thorough examination to eliminate the risk of complications.
Why and when to install a membrane?
The barrier membrane performs several functions at once that contribute to the patient’s recovery. The design reliably fixes the osteogenic material in the place and position where the dentist installed it. Also, the membrane does not allow bone-destroying cells - osteoclasts - to pass through, which are normally responsible for the balance of metabolic processes in the alveolar process. An additional function of the membrane is protection against infection. In the case of sinus lifting, the membrane is installed under the bottom of the maxillary sinus and reduces the risk of penetration of osteoplastic material into the sinus through perforations in the mucous membrane.
Indications for use of barrier membrane:
- Preventing the resorption of bone tissue in the alveolar ridge after tooth extraction (if treatment is not performed immediately and the patient will have to remove the load from this area for some time);
- Any type of bone grafting (retention of bone grafting material);
- Dental implantation with one-stage bone grafting (reinforcing function);
- Performing flap surgical interventions for periodontitis.
Barrier membranes appeared not so long ago, and therefore their cost remains high. Dentists make decisions based on the patient's financial status and may sometimes refuse to use them. In general, the use of a barrier membrane allows for better control of the outcome of bone grafting and reduces the likelihood of adverse treatment outcomes.
Why else is plasma lifting done in dentistry?
In addition to osteoplasty, plasma lifting in dentistry is used in the following cases:
- generalized or localized chronic periodontitis and periodontal disease, gingivitis, resistant to other conservative dental treatment methods;
- traumatic extraction of teeth or during reposition of jaw bone fragments as a result of trauma to the maxillofacial area;
- prevention of peri-implantitis, alveolitis and periodontal inflammation;
- to accelerate tissue regeneration after vestibulo- and gingivoplasty.
How to install a barrier membrane?
The innovative method of using a barrier membrane requires certain experience from the dentist, as well as clear knowledge of the technique of performing the stage. The structure is fixed as follows:
- Performing local or general anesthesia with the addition of sedatives (the last point is not always necessary);
- An incision in the outer soft tissues of the gums and moving them away from the bone of the alveolar process;
- Replenishment of the required amount of bone tissue using one of the previously selected methods;
- Fixing a modern structure made of collagen or metal with special titanium screws to adjacent teeth or to the jaw bone itself;
- Repositioning the soft gum tissue and securing it with surgical sutures.
When using a membrane that does not dissolve, after a certain time almost all steps are repeated to remove the structure.
A prerequisite for the patient’s successful recovery is careful oral care in the postoperative period. A person must maintain personal oral hygiene and follow all recommendations of the dentist. It is also important to quit smoking a few days before surgery and for the entire rehabilitation period.
Characteristics and purpose
Collagen is a substance that has the ability to completely resorb. Thanks to this characteristic, the product is used in different areas of dentistry.
The membrane performs a protective function and acts as a barrier to the apical entry of epithelial fragments into the organ. The device helps ensure self-reproduction of bone in the area of augmentation.
The participation of soft fragments in bone regeneration is limited.
Upon contact with moisture, the drug changes color and becomes transparent. The dense fibrous structure prevents the entry of gingival fibroblasts and promotes the growth of bone-forming fragments.
The material is durable and has low antigenic parameters.
Is it possible to do without a barrier membrane?
Since fixing a barrier membrane is not cheap, many patients are interested in the question of alternatives to this design. In general, the cost of different types and brands of such dental material varies significantly. But if surgical intervention requires the use of a serious and reliable design, then it is not recommended to purchase a cheap analogue, because it still will not bring the expected result.
Performing bone grafting with fixation of barrier membranes is not available to all dental clinics. Refusal to use such structures will increase the likelihood of any complications, but in general will not affect the course of the operation and the recovery stage. But if it is possible to use a barrier membrane for bone grafting during implantation, then it is better to agree to its installation.
Genoss Collagen Membrane
Genoss multilayer resorbable collagen membrane is made from bovine type I collagen.
Collagen Membrane, Genoss ideally stabilizes bone material, perfectly epithelializes in the open state, therefore it is widely used in all possible operations of directed bone regeneration.
Collagen Membrane GCM1520
Collagen Membrane GCM3040
Collagen Membrane GCM2030
Collagen Membrane GCM1020
Plasmapheresis - obtaining a membrane from blood plasma
For the plasmapheresis procedure, not blood from a vein is used, but plasma from centrifuged blood. When injecting autoplasma, the tissues of the oral mucosa are saturated with nutrients. The material is otherwise referred to as “platelet-rich plasma” containing platelet concentrate.
Effectiveness is ensured by plasma with a large number of platelets in 1 μl. To achieve such saturation of the biomaterial, plasmapheresis is necessary.
1. Up to 20 ml of blood is drawn from the patient's elbow.
2. To separate the blood into its constituent components and separate unnecessary elements, it is centrifuged twice in a test tube for 15 minutes.
3. The necessary components are removed - plasma and fibrin clot.
Platelets, fibrin and biologically active substances are saturated, transforming into autoplasma. An injection is given into the marginal gum, interdental papilla or gingival projection of the tooth root.
Also, the remaining fibrin clot (membrane from blood plasma) is used for surgical interventions - osteoplasty, stimulating the healing of the hole. The shelf life of the membrane is no more than a few hours. Plasmapheresis is performed exclusively on the day of surgery. Our specialists have all the knowledge and skills to ensure technically complex operations.
Indications and contraindications for the use of plasma lifting
Indications:
- increasing the rate of tissue healing during sinus surgery and bone addition;
- recession plastic;
- treatment of periodontal diseases;
- activation of growth factors in bone cells after tooth extraction;
- implantation simultaneously with the introduction of bone material;
- various surgical interventions.
Contraindications:
- malignant neoplasms;
- systemic diseases of the blood system that do not allow plasma to be isolated or used effectively;
- decreased immunity;
- diseases in the acute stage;
- taking antibiotics;
- mental illness.
Benefits of using blood plasma
The introduction of a platelet membrane naturally activates cellular growth factors of the jaw bone and periodontal tissues, increasing the rate of recovery. Regeneration and acceptance of implants or bone material by the body is much faster, and the likelihood of inflammation is significantly minimized.
Blood plasma membranes have a positive effect on:
- increase in the rate of cellular growth factor in the bone after implantation;
- absence of allergies that could occur when interacting with foreign materials;
- accelerated gum recovery after implantation or plastic surgery;
- prevention of inflammation around the implant;
- reduction of swelling and pain after surgical procedures;
- optimal tightening of the socket after tooth extraction;
- minimizing inflammation during gingival curettage and cleaning periodontal pockets.
What is platelet fibrin
Human blood contains formed elements, one of which is transparent, anucleate cells - platelets. They take part in the process of blood clotting and stopping bleeding. During the destruction of the walls of a blood vessel, platelets, disintegrating, release components that form blood clots. In the 80s, an effective function was discovered: to increase the rate of healing and tissue restoration. This process occurs due to the release of growth factors (hormonal components) that enhance the regeneration of old cells, as well as the growth and increase in the number of new cells.
Platelet autoplasma is not only formed elements, but also saturated platelet fibrin. This is a yellowish liquid released when blood is processed in a special centrifuge.
It contains:
- platelets;
- fibrin;
- fats;
- hormones;
- nucleic acids;
- mineral components.
After the autoplasma is introduced into the jaw bone, growth factors are activated within a week. The tissues are intensively saturated with oxygen, and a dense capillary network is formed. The rate of restoration of jaw bone cells and their growth, as well as tissue nutrition, increases.
Human autoplasma is saturated with nutrients and is biocompatible with the body, because it is its own product. Consequently, engraftment is successful and side effects never develop. The restoration is proceeding as planned.
Algorithm for performing osteoplasty
Bone grafting consists of several stages, including preparation, surgery, rehabilitation, and osteosynthesis. Osteoplasty algorithm:
- preparation begins with a comprehensive examination of the patient. During this stage, the doctor collects anamnesis, identifies indications and contraindications, and visual and hardware diagnostics. All this allows the surgeon to make a diagnosis, determine the degree of atrophy and the characteristics of the clinical case. Based on the conclusions made, the doctor plans the type and course of surgical treatment;
- Sanitation of the oral cavity is a prerequisite for the operation. This complex includes dental and periodontal treatment (if necessary), professional dental cleaning;
- surgical stage – performed according to a developed protocol depending on the type of plastic surgery. General scheme: local anesthesia, gum incision to gain access to the operated area, preparation of a bed for laying the graft, fixation of bone material and growth stimulator, suturing of the surgical wound;
- the process of osteosynthesis (formation of new bone tissue). Lasts up to 6 months. The duration depends on the type of plastic surgery and the transplant materials used.
General recommendations for the rehabilitation period:
- do not eat or drink for 3 hours after surgery;
- do not brush the surgical area with a toothbrush for at least 10 days;
- food should not be hot or cold, it should be finely chopped during the entire time until the surgical suture heals;
- Do not drink through a straw or blow your nose (especially after a sinus lift);
- you should refrain from physical activity (including fitness) for at least 2 weeks after surgery;
- be sure to take medications prescribed by the doctor;
- it is necessary to monitor your well-being and the site of surgery. If inflammation, swelling, or temperature occur, immediately consult your doctor.
Expert advice: 2 hours before surgery you should refrain from eating. After surgery, it is necessary to meticulously adhere to the surgeon’s recommendations on nutrition, hygiene, and physical activity. stress, as well as taking prescribed antibiotics and other medications. Otherwise, postoperative complications are possible.
The dental network offers osteoplasty services. Our surgeons are highly qualified and improve their skills in famous clinics in Russia and Europe. The quality of surgical operations meets international standards. We have a system of family and cumulative discounts. We provide the necessary documents for filing a tax deduction. Convenient appointment schedule with specialists: daily without a break from 9 to 21 hours (Sunday from 10 to 16).
Branches of our orthodontic center are located in Moscow within walking distance from the metro:
- Art. Alekseevskaya (VDNKh district, etc. Mira), address: st. 3rd Mytishchiskaya house 3, building 2;
- Art. Shelepikha, address: Shelepikhinskaya embankment, address: building 34, building 1.
You can trust us with your health, come, we will solve any dental problem. Waiting for you!
Benefits of Collagen Membrane, Genoss
- the minimum period of epithelization in the open state is only 2-3 weeks (!),
- size (thickness 0.3 mm),
- resorbability in 8-10 months,
- rigidity is a guarantee of excellent barrier function and reliable stabilization of bone material,
- ease of use.
The excellent characteristics of the Genoss membrane have already been appreciated by many dentists, so today you can inexpensively buy a Genoss collagen membrane in the Dental Market online store.
The price of the Genoss collagen membrane at Dental Market is more than acceptable, especially considering the real opportunity to receive free consultation from a specialist, assistance in placing an order and fast delivery.
Call Dental Market by phone 8 (495) 118-76-20
.
Online store "Dental Market" - flexible prices, quick help in any situation!