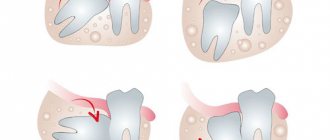
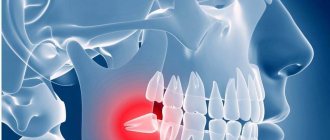
Wisdom teeth (eights, third molars) are the last units on each side of the dentition. They are the last to erupt, when the dental system is fully formed. And in most cases, their appearance causes a lot of problems. Since they often do not have enough space in a row, they grow incorrectly: at an angle, to the side, horizontally, they interfere with neighboring units, and injure the mucous membranes of the cheeks and tongue.
Whether wisdom teeth need to be removed depends on the clinical situation. The doctor will not remove third molars “just in case.” There must be medical indications for this. The anatomy of eights is more complex; these are the largest units in a row with a developed root system. Although they belong to the chewing group of teeth, they do not take part in the chewing process; this function is weakened or absent in units. The main function of third molars is to keep the teeth in the row from moving apart.
What problems may arise
- almost 80% of cases
, the eruption of third molars is accompanied by various purulent-inflammatory processes.
A mucous hood
is formed over the erupting unit , a pocket is created around it, where bacterial plaque and food debris accumulate, which leads to purulent inflammation -
pericoronitis
. - Often, figure eights grow towards the tongue, cheek, palate, constantly injuring the mucous membrane, causing a lot of painful and uncomfortable sensations. Chronic injury to soft tissues
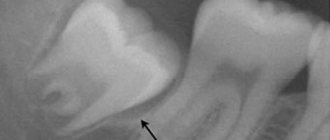
can lead to the formation of ulcers, erosions, and the development of leukoplakia (hyperkeratosis) - the mucous membrane in the injured area becomes denser. If the cause (traumatic tooth) is not eliminated, there is a risk of neoplasm (including malignant). - Between 8 and 7 (on contact surfaces) a carious cavity is formed
where food is constantly clogged, contributing to the rapid development of caries. The carious process affects not only the number eight, but also the 7th molar, which is important for the dental apparatus. In case of interdental caries, it is necessary to remove the wisdom tooth and properly treat the seventh molar. - Sometimes the figure eight, positioned horizontally in the gum, rests on the root of a neighboring tooth, injuring it, causing the formation of a cyst
. In the worst case scenario, such a pathology can even lead to resection of the jaw bone. As a result of a long asymptomatic period, cysts can acquire significant sizes and damage the surrounding bone tissue and neighboring units. - Wisdom teeth can put serious pressure on adjacent units, moving them out of place. This pressure is transmitted to all teeth, causing row deformations
, malocclusion, and periodontal disease.
In what cases is wisdom tooth removed?
The most common indication for surgical removal of third molars is their abnormal position.
or
difficult eruption
. In many cases, they remain inside the jawbone for a very long time, breaking through to the surface with difficulty, causing many problems. In such clinical situations, the maxillofacial surgeon performs a rather complex operation to extract the tooth from the bone tissue.
There are many reasons why wisdom teeth are removed. A direct indication for surgical extraction of the figure eight is:
- hygiene of third molars is difficult or impossible;
- caries, destruction of the coronal part;
- impacted molar (unerupted partially or completely);
- displacement of teeth in a row due to the growth of eights;
- dystopia (incorrect placement of 8s in a row) or traumatic occlusion;
- difficult access when treating adjacent units;
- location at an angle, promoting curvature and destruction of neighboring units;
- eruption beyond the boundaries of the dentition;
- germination of wisdom tooth roots into the maxillary sinus;
- the eruption of the figure eight caused complications (facial neuralgia);
- incomplete eruption with the presence of a hood of gingival mucosa.
Often, extraction of wisdom teeth is carried out for orthodontic indications, when, due to their abnormal position, the entire row begins to shift - the quadruples and incisors shift, forming crowding of the anterior group of dental units. With braces, wisdom teeth are removed to shorten the correction period and eliminate complications if figure eights begin to erupt during treatment.
Recommendations after removal
Regardless of the method by which the tooth was removed, in the first 2 days the patient must observe a special diet, activity and hygiene. This is necessary to preserve the blood clot in the wound, which helps maintain the sterility of bone tissue and promotes its regeneration.
In the first 48 hours after removal you cannot:
|
Failure to comply with these recommendations most often causes the clot to fall out of the socket and the development of alveolitis or bleeding.
After tooth extraction it is recommended:
- make oral baths from chamomile and sage decoctions (the decoction prepared according to the instructions is taken into the mouth and held there for 10 minutes, without rinsing or moving the tongue) 2-3 times a day;
- take non-steroidal anti-inflammatory drugs (especially after atypical removal, when the tissue is severely damaged and swelling occurs) - nimesulide, diclofenac sodium, ibuprofen, paracetamol, etc. (it is important that the medicine does not reduce blood clotting).
Sometimes patients need preliminary preparation for removal. People taking aspirin and other medications that impair blood clotting should stop taking them a week before the procedure. For those who suffer from increased excitability and anxiety, you can start taking valerian or motherwort 1-2 weeks before removal, having previously agreed with your dentist and your therapist.
Even if the removal was painless and quick, you should not ignore the doctor’s advice. The right approach to rehabilitation will help you avoid complications and recover faster.
Why remove wisdom teeth
Third molars are rarely preserved - they are destroyed early or removal is necessary for the proper functioning of the dentition. Most dentists prefer to remove pathological 8 even before they can seriously harm the health of the jaw (especially the lower one) of the entire row.
Cannot be deleted
wisdom tooth in the absence of the 6th and 7th molars. A contraindication to extraction is inflammation of the periodontium, root, bone or gum, since there is a danger of spread and aggravation of the pathological process against the background of a postoperative wound. The limitations to surgical extraction of third molars are:
- location 8 in the area of malignancy;
- pregnancy;
- hypertension stage II-III;
- suffered a heart attack or stroke less than 3 months ago.
All operations, including dental ones, in these cases are carried out after consultation with the patient's attending physician.
Smells
What smell do neither patients nor doctors like? These are negative smells. The aroma of burnt bone, pus, unwashed body. Aggressive odors of drugs (including alcohol).
In addition, the same scent of perfume can be pleasant to some and disgusting to others.
The solution is simple - the clinic should be as neutral as possible. It is necessary to avoid obsessive smells of perfumes and air fresheners in the halls. Perhaps the smell of freshly brewed coffee is one of those few smells that is favorably received by the maximum number of people, and this smell creates comfort in the clinic lobby.
When can they not be removed?
Modern dentistry clearly formulates its attitude towards figure eights - you don’t have to remove wisdom teeth provided:
- there is enough space for them to cut through;
- erupted molars occupy an anatomically correct position and do not harm neighboring units;
- nothing prevents the treatment of the eight;
- third molars do not impede hygienic care of teeth and gums;
- A wisdom tooth is needed as a support for fixing a bridge or other orthopedic system (if 7 is missing).
If the third molars are affected by caries, they somehow interfere with other units in the row or the chewing process, or regularly injure the mucous membrane - they must be removed. In this matter, world dentistry is ruthless; the presence of eights is allowed exactly as long as they do not harm the health of the dental system and do not disrupt its functionality.
Awareness/lack of awareness of the process
It is important to find out in a preliminary conversation what type a particular person belongs to. Some people feel calm, knowing in detail what will be done to them, while others are only more alarmed by the details, and they prefer to abstract themselves from the process as much as possible, believing in “magic,” if you will.
You can compare these reactions with the experiences of passengers during air travel. Some people feel calm until they know all the processes in aircraft systems. And others suffer from aerophobia, and they are helped by various information materials that cover the details of the work. At the same time, for the first category, such knowledge can be dangerous and destroy their peace of mind and faith in the divinity and reliability of air transportation.
Is it possible to remove several wisdom teeth at once?
It is possible to remove two wisdom teeth at once, but this is a certain stress for the body. More often, this operation is performed when it is necessary to remove the eights from one side (1 upper, 1 lower). This is done to maintain normal nutritional function. During surgical extraction, powerful anesthesia is used, so the operation is painless.
But after removing a large molar, a fairly large wound remains. Until it heals, the load on the operated area should be minimized; accordingly, you can chew on the side opposite the hole. If you remove both figure eights on the upper or lower jaw, eating will become problematic. And this affects the digestive system, immune system, and general health.
Visual background
The patient does not really understand the difference between an installation for 2 million and for 200 thousand. But he immediately sees the untidiness. Dirty floor, shabby, protruding wires, dripping faucet, sparking wiring, dried blood stains (including on the clothes of doctors) and a broken window.
Excessive pretentiousness both in the interior and in the appearance of health workers can also increase anxiety - “Am I overpaying for all this tinsel?”
The most optimal is a neat, clean office with a minimum of visual noise. With neat, tidy employees (but no frills). Such a visual background usually coincides with the patient’s expectations and allows him to relax a little before the upcoming torture.
During the appointment, it is also recommended to use darkened glasses (reduce anxiety) or virtual reality glasses with headphones (distract from the ongoing manipulations, which has a beneficial effect on the course of the procedure).
Treatment of complications with the growth of figure eights
The most common complication with the growth of figure eights is pericoronitis
(formation of a gum hood). When a molar erupts, it is forced to overcome many obstacles: the jaw bone, periosteum, and periodontal tissue. During long, complex eruption, a specific mucous canopy (hood) is formed over the molar. Bacteria and food particles penetrate under it, which causes inflammation.
If coronary artery disease is not treated, the consequences will be serious, the inflammation will spread to the periosteum and jaw bone. This is fraught with the development of periostitis, osteomyelitis, tissue suppuration with the formation of phlegmon, cysts, and fistula tracts. Nearby tissues may be affected, and inflammatory ENT pathologies (otitis media, sinusitis) may occur.
Treatment of pericoronitis is surgical and involves excision of the mucous hood. The operation opens access to the growing eight. The doctor removes the affected tissue, carefully treats the surgical area, and evaluates the clinical picture. According to the situation, he decides whether to remove the eights or help the molar to erupt completely, taking the correct place in the row.
Leadership and Communication
As I said, patients are living people. And many who come to us are leaders who are accustomed to the fact that they decide, and not for them. The doctor’s task is to remain a leader within the office. A different situation can be disastrous for the patient himself. My favorite example is the cartoon “The Greedy Rich Man,” about what happens when a professional follows the lead of the customer. The doctor's job is to let the patient know that he knows what he is doing and the patient is in good hands. By the way, competent irony can relieve tension.
Physicians themselves must exude calm and reliability, both verbally and non-verbally. Calmness, friendliness, warm look, smile. Any gestures and touches towards the patient should be smooth and confident. Without unnecessary movements, fuss. It is good if all the necessary tools are prepared in advance, and dialogues between the doctor and the assistant are minimized or absent altogether. An interesting fact is that the measured chatter between the doctor and the assistant on abstract topics during surgery makes some patients distract themselves from their worries and “prick up their ears” in anticipation of the “story.”