For many people, rotten wisdom teeth pose a real and very serious threat to the health of the entire oral cavity - problematic third molars or, as they are also called, “eights” cause a lot of trouble for their owners. They erupt much later than the rest of the dentition (at about 20-25 years) and often become a problem already at the eruption stage.
What complications can wisdom teeth cause?
Difficulties arising from third molars are primarily associated with the late timing of their eruption and some anatomical features of the jaw structure:
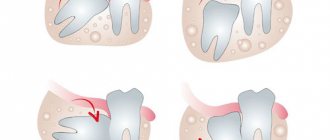
- Lack of space for normal eruption. By the time the “eights” begin to cut, a person’s dentition is usually already fully formed, and there may simply not be enough space for the third molars. In addition, during evolution, the human jaw has decreased by about 1 cm, which also does not contribute to the normal growth of “eights”. In this case, tooth extraction is indicated to prevent displacement of the entire dentition.
- Incorrect position in a row (dystopia). Leads to soft tissue injuries, destruction and displacement of adjacent teeth.
- Incomplete eruption (retention). Impacted “eights” cause a lot of problems and discomfort - often such a wisdom tooth causes inflammation of the gums and diseases of the “neighbors” in the dentition.
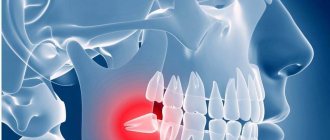
- Pericoronitis. An inflammatory disease characterized by swelling of the gums near the wisdom tooth followed by suppuration. When teething is difficult, a so-called hood of mucous membrane is formed around the figure eight, which is the optimal place for the accumulation of food debris and the proliferation of bacteria. In this case, the wisdom tooth is cut and hurts due to inflammation of the hood. If nothing is done, gum inflammation develops not only next to the tooth, but throughout the entire jaw - this will require long-term and costly treatment of the gums.
- Deep caries of wisdom tooth. Third molars, as a rule, begin to deteriorate quickly, often at the eruption stage. Why do wisdom teeth crumble? This is due to both the peculiarities of its structure and its position: it is simply impossible to clean the “eights” well with paste and a brush, so food debris and bacteria necessarily accumulate there, creating favorable conditions for the development of infectious processes.
In all the described situations, it is better to remove wisdom teeth immediately, without waiting for serious complications to develop, and you will have to spend a lot of time and money on treating nearby teeth, as well as inflamed gums.
Is it necessary to place an implant instead of a removed figure eight?
Theoretically, a dental implant can be placed in place of an extracted wisdom tooth that has been affected by caries. But in practice this is not done for a number of reasons. Firstly, the anatomical location of the tooth makes such implantation extremely difficult. Secondly, the load on the eighth tooth will sooner or later lead to loosening of the rod on which the implant is attached. Food will get into the gaps formed and microbes will multiply, which can lead to inflammation. Thirdly, even with proper installation of the implant, there will still be a joint between the gum and the crown, in which bacteria will accumulate if hygiene is difficult.
And finally, replacing a removed figure eight with an implant does not make practical sense, especially if a person’s other chewing teeth function normally. Also, the absence of these teeth does not impair the quality of life and does not affect human health. Therefore, after removing the third molar, there is no need to install an implant in its place.
Can third molars be treated?
Wisdom teeth, like any other teeth, can be treated. But only if they erupt correctly, do not threaten the health and position of the rest of the dentition, and there is confidence that the treatment will be successful. If the specified conditions are met, it makes sense to preserve the “eight” for the following indications:
- If the sixth and seventh teeth are sick or severely damaged and must be removed, in this case the wisdom tooth is left as “the best of the worst” in order to provide the patient with at least some conditions for chewing, and the doctor - the basis for future prosthetics.
- If the six and seven have already been removed and it is necessary to preserve the abutment tooth for installation of prosthetic structures.
- In the presence of an antagonist tooth, completely healthy and subject to preservation.
In case of curved roots that complicate endodontic intervention, severe tissue destruction, dystopia or retention, no competent dentist will undertake to treat the “eights” - he will definitely recommend removal.
To treat or remove a tooth?
Today, dental organizations and doctors are divided into two camps.
The first solve patients' problems in quick and radical ways. These are dentists from public and poorly equipped clinics who cannot provide quality treatment due to a lack of material resources or level of knowledge.
The latter are looking for all sorts of ways to maintain a full bite. They evaluate patients’ problems from the standpoint of “can they be restored or cured,” rather than offering immediate tooth extraction as the only correct solution.
Why are “rescuer” doctors the best option for patients? It's simple. Restoration work:
- guarantee long-term dental health;
- do not force you to think about implants, crowns;
- minimize pain;
- maintain the natural attractiveness of a smile;
- provide the correct bite or restore it.
Frequent concerns of patients on the topic of “treating or removing” a tooth concern:
- enamel cracks;
- fillings that burst along with the crown;
- third “wise” molars;
- resorcinated teeth.
Four problems are the “stumbling blocks” on which the opinions of dentists of the old and new schools differ. The most reasonable way in this case is to go to a well-equipped clinic or get several independent dental consultations.
Only then will the patient find answers to all his questions: is it possible to restore a cracked tooth, whether to remove wisdom teeth and resorbed teeth, or to cure them.
Why are wisdom teeth needed?
Why does our body need third molars at all? In fact, these are rudiments that not all people today erupt - approximately a third of the entire population of the planet does not even have the rudiments of third molars, although a few thousand years ago absolutely all adults grew wisdom teeth. They practically do not perform the chewing function, since the rest of the healthy teeth usually cope with it.
Today, “eights” are needed only as a “backup option” in case the first and second molars fall out or are severely damaged, and also as a factor preventing the loosening of neighboring teeth. They can also serve as a support for prosthetics - but, again, in all these cases we are talking about healthy and correctly erupted “eights”. In the same case, when a person has rotten wisdom teeth in his mouth, they will not be able to perform any of the indicated functions and it is better to remove them so as not to expose the rest of the dentition to the risk of infection.
Indications for removal
Healthy, well-positioned third molars with good oral access for possible treatment do not need to be extracted. There are clear indications for such an operation, and if they exist, it should be removed without waiting for complications:
- Deep caries of the wisdom tooth, as well as lack of normal access for full treatment.
- Chronic inflammatory processes caused by third molars, including in cases where the wisdom tooth caused inflammation of the gums.
- Chronic injuries to the oral mucosa due to incorrectly positioned “figure eight”.
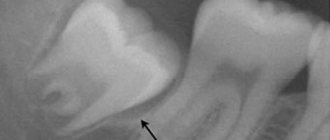
- Impacted or dystopic teeth.
- The need for orthodontic treatment of bite defects if the doctor believes that the “eights” will prevent the dentition from occupying the correct position.
In all of these situations, it is recommended to remove the “eights” without delay.
In addition to location, dentists classify caries according to the depth of the pathology:
- The spot stage is considered the mildest. This type is easy to clean and saves the tooth from further damage.
- The superficial type of caries is characterized by the process of demineralization of tooth enamel with further destruction.
- Deep caries is characterized by irreversible destructive effects on the tooth due to the development of carious microflora. During the examination of the affected tooth, you can see a layer of dentin located between the pulp and the bottom of the carious cavity.
Based on the types of anatomical location, caries of dentin, enamel and cement is distinguished.
Removal Features
As a rule, operations to remove third molars are always considered difficult, since these are the teeth that usually cause more problems. The operation can be simple, provided that the “figure eight” is located on the upper jaw and does not have pronounced developmental abnormalities. In all other cases (as well as in situations where the tooth is in the upper jaw, but has strong, curved and branched roots), the operation is considered complex and must be performed by a qualified dental surgeon.
Before performing an intervention, the doctor determines possible contraindications for a particular patient, examines an x-ray of the problem area and determines the optimal tactics for the operation. The duration of the procedure ranges from 1-10 minutes for simple removal and up to 20-120 minutes for complex removal, requiring a series of manipulations and suturing of the hole.
Should resorcinated teeth be removed?
Patients of Soviet dentistries are aware of what resorcinol fillings are. Beginning in 1912 and for almost 100 years, caries was resorcinolized - eliminated using the resorcinol-formalin filling method. At the same time, the dentists did not inform the patients that subsequently the teeth turn yellow, decay, become increasingly fragile, and cannot be refilled.
Times have changed, and seemingly harmful fillings can be replaced with modern filling compounds. However, this turned out to be practically impossible - it is impossible to clean the channels from the resorcinol-formalin mixture. During the hardening process, the filling acquires the density of glass and is soldered to the walls of the root canal. The verdict of most doctors when dealing with resorcinated teeth is the same - removal.
But there is no need to rush in this case either. Today, modern dental equipment allows you to drill out and remove even the strongest glassy material and bring the tooth into excellent condition. Yes, not all clinics have the necessary equipment, but it is there. And finding “your” doctor after several consultations will completely solve this problem.
Removal of wisdom teeth under general anesthesia
Many patients are afraid to remove problematic “eights” because they fear that the process will be painful. However, you should not postpone the operation because of your own fear: modern methods of anesthesia allow the removal to be performed as painlessly and comfortably as possible for the patient.
Doctors usually recommend performing the intervention under local anesthesia, which will be sufficient to ensure the patient is comfortable during the operation. If for some reason a person is not satisfied with the methods of local anesthesia, there is always the possibility of having a wisdom tooth removed under anesthesia. It should be remembered that this option of pain relief is not available to everyone - there are certain contraindications:
- Decompensated diabetes mellitus and cardiovascular diseases.
- Post-infarction or post-stroke periods for up to 6 months.
- Acute inflammatory diseases of internal organs, including the respiratory system.
- Epilepsy.
- Severe thyroid disease.
- Bronchial asthma.
- Alcohol or drug intoxication.
The presence of at least one of the listed positions makes the removal of wisdom teeth under general anesthesia impossible. Before the operation, the patient must be examined to identify any contraindications to the use of anesthesia. In addition, you need to remember that certain preoperative preparation will be required, and the clinic itself, in which the wisdom tooth will be removed under anesthesia, must have all the necessary equipment, as well as a team of specialists who will treat and monitor the patient’s condition (anesthesiologists, resuscitators, trained nursing staff).
Treatment or removal during pregnancy
In cases where a wisdom tooth is cut and hurts, causing constant discomfort to the pregnant woman, it can and should be treated regardless of the gestational age. If there is no acute pain and treatment can be postponed, then it is advisable to carry it out in the second trimester of pregnancy or after childbirth.
It is worth remembering that wisdom tooth removal, especially under anesthesia, is definitely contraindicated for pregnant women. Removing third molars is strongly not recommended due to the complexity of such an operation and the risk of developing postoperative complications. As for anesthesia, it cannot be used either for removal or for treatment - during pregnancy, only local anesthesia can be used, and the drugs should be selected very carefully and taking into account the patient’s condition.
Despite their name, wisdom teeth do not bring their owners increased intellectual abilities, but they can cause a number of very unpleasant problems with oral health. Typically, third molars “lead with them” swelling of the gums, purulent inflammation, the development of caries of neighboring teeth, as well as severe pain. Therefore, in modern dentistry they prefer to remove them, without waiting for serious complications to arise and longer and more expensive treatment to be required. In many European countries today, a common practice is to remove the “eights” immediately after their appearance, regardless of their condition and the correctness of eruption.
What to do if there is a hole in your tooth?
If you notice the development of at least the first stage, immediately go to a visit to the dentist. The hole is the last stage of carious damage, which can be very difficult to get rid of. Professional treatment of holes is carried out only in a dental clinic. The standard work plan of a specialist usually includes:
- Treatment of the oral cavity (plaque and tartar on the diseased tooth are removed, normal hygiene procedures are carried out).
- Anesthesia of the hole site (if the disease is of significant complexity).
- Removal of areas of dental tissue affected by caries, treating them with an antiseptic drug.
- Drilling the required shape to install a filling in it; if necessary, a therapeutic pad is applied to provide an anti-inflammatory effect on the nerve.
- Sealing the treated cavity with filling material, the color of which fully matches the color of the tooth. After this, the filling is adjusted according to the bite, ground and polished.