Stomatitis
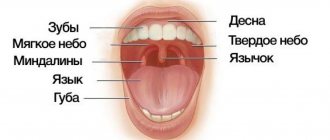
This is a group of diseases characterized by inflammation of the oral mucosa with hyperemia, swelling, and an increase in the amount of mucus in the oral cavity.
Depending on the severity and depth of the lesion, even ulcers or foci of necrosis may form in the oral cavity, sharply disrupting the general condition - fever, weakness, anxiety, refusal to eat. There are many causes of the disease: mechanical, chemical, thermal, bacterial factors. Often the cause of the disease in infancy is contaminated nipples, toys and other objects that fall into the child’s mouth. Stomatitis often develops as a result of infectious diseases (measles, scarlet fever, influenza, whooping cough, etc.). The mucous membrane of the oral cavity acquires a bright red color, becomes swollen, and tooth marks are visible on the mucous membrane of the cheeks and tongue. Saliva becomes viscous and viscous. The mucous membrane is covered with a whitish coating. The tongue is dry, swollen, often with a brown tint, chewing is painful. The duration of the disease is from 1 to 3 weeks, the prognosis is favorable.
A general preventive rule for children and adults is to maintain good oral hygiene.
Thermal injuries of the oral mucosa in children.
They are rare in children, but are possible when eating hot food, especially milk and broth. The mucous membrane of the lips, the tip of the tongue, and the anterior part of the hard palate is mainly affected. It becomes swollen, hyperemic, and painful when touched. Less commonly, superficial intraepithelial vesicles form, which immediately burst. Upon examination in this case, fragments of white epithelium are visible on a hyperemic base. Prescribing antiseptics is unnecessary, since there is no deep defect in the epithelium, and therefore no conditions for secondary infection. For pain, painkillers are indicated: applications of a 0.5% solution of novocaine, lysozyme, 5–10% suspension of anesthesin in oil.
Gingivitis
An inflammatory process that causes swelling and tenderness of the soft tissues. If not treated in a timely manner, the problem worsens and becomes chronic.
The main causes of gingivitis:
- insufficient oral hygiene;
- thermal or chemical burns;
- use of certain medications;
- unbalanced diet (insufficient amount of vitamins in food)
- smoking;
- some infectious diseases;
- gastritis;
- ulcerative processes in the digestive system;
- caries.
Forms and types of gingivitis
Depending on the clinical situation and the nature of the development of the disease, acute and chronic gingivitis are distinguished. Acute gingivitis
manifests itself in the form of classic signs of the disease: redness, swelling and bleeding of the gums.
Chronic gingivitis
develops more quietly, without pronounced signs, but gradually leads to the growth of gum tissue (hyperplasia), which entails partial and complete coverage of the surface of the tooth crown by the gum.
Prevention measures
By following simple rules you can reduce the likelihood of serious oral diseases:
- Brushing your teeth at least 2 times a day after eating;
- Using dental floss and mouthwash;
- Balanced diet;
- Rejection of bad habits;
- Visit the dentist at least once every six months.
Leukoplakia of the oral cavity: causes of the disease
The reasons causing the development of the disease include:
- Smoking. When using tobacco, the oral cavity is exposed to various irritants, including thermal (incoming smoke has a temperature of about 60 degrees Celsius) and chemical (nicotine, tar and combustion products). No less dangerous is chewing tobacco, which is also a provoking factor.
- Eating either very hot or very cold food on a regular basis for a long time.
- Mechanical trauma (bad bite, sharp edges of teeth, orthopedic structures installed with violations).
- Metal seals that cause galvanic currents.
- Inhalation of vapors of gasoline, benzene, varnishes and paints, as well as other resins.
- Hormonal imbalance, constant stress and lack of retinol.
Periodontitis
Periodontitis is an inflammation of periodontal tissues, which includes the teeth, ligaments, cementum and gums. Periodontitis as a disease is a consequence of gingivitis - a minor inflammation of the gums, the main cause of which is neglect of oral hygiene. If with gingivitis the inflammation spreads exclusively to the soft mucous membranes, then with periodontitis the ligaments that hold the teeth in the sockets are affected. This is why in 90% of cases when this disease is diagnosed, tooth mobility is observed, which eventually leads to their loss.
The most common causes of the disease are the following:
1. Improper or irregular oral care
. Dental plaque, which is present on the surface of the teeth and in the spaces between teeth, is not as safe a substance as it might seem at first glance. Soft and easily removed at the beginning, it goes through certain cycles of “development”. The result is the mineralization of plaque and its transformation into hard tartar. This process in most cases is observed in those who do not pay due attention to daily oral care or use an incorrectly selected toothbrush, toothpaste and mouthwash.
2. Poor blood supply to the gums
. Periodontitis is one of the most common problems among smokers. Substances contained in tobacco smoke lead to a narrowing of the blood vessels in the oral mucosa and their fragility, which impairs the blood supply to the gum tissue and supporting apparatus of the teeth. A slowdown in blood circulation and, as a consequence, the development of periodontitis is also facilitated by a lack of chewing load caused by eating habits (for example, the predominance of soft foods in the diet).
3. Nutrient Deficiency
. The lack of fresh vegetables, fruits, herbs, a sufficient amount of fish, meat and dairy products in the diet quickly leads to a lack of essential substances in the gum tissue. If poor nutrition is a permanent habit, then over time the metabolic processes in the gums are disrupted, which creates the ground for inflammation and periodontitis. A deficiency of vitamins A, C and group B can lead to negative consequences.
Treatment of periodontitis
Professional teeth cleaning is an integral step in the treatment of periodontitis. This procedure removes physical obstacles (plaque and tartar) that prevent the gums from returning to their previous position and tightly covering the teeth.
Drug treatment - the use of antiseptics for topical use. This need is due to the high risk of spread of inflammation and infection to other tissues.
Surgery
At an advanced stage of periodontitis, when the inflammation has spread deep into the bone tissue, surgical intervention becomes necessary. Such manipulations include partial excision of the gums (gingivectomy), washing of periodontal pockets with medicinal solutions, removal of stones, and flap operations. In some cases, surgical treatment of periodontitis involves the implantation of bone tissue substitutes or the application of collagen or artificial membranes to restore the supporting apparatus of the tooth.
Compliance with oral care rules
Without regularly removing plaque and protecting the oral cavity from bacteria, it is impossible to achieve sustainable results in the treatment of periodontitis. Hygiene procedures twice a day with properly selected products, the use of dental floss and rinses will help make recovery faster.
Periodontal disease
Dental periodontal disease is a serious disease in which the last stage of gum inflammation occurs. This is often the cause of the development of infectious diseases, gastritis, stomach ulcers or cirrhosis of the liver. Even more often, the patient’s teeth simply fall out, and he cannot lead his usual lifestyle or eat his favorite food.
How to recognize periodontal disease
The signs of this dental disease are unclear and blurred. The patient is most often concerned about:
- exposure of the necks of the teeth;
- presence of tartar;
- burning gums;
- discomfort when eating.
There are 3 stages of periodontal disease:
- Easy. The patient has no complaints; very rarely there is a reaction to cold or hot food. The presence of periodontal disease can be determined during a dental examination. The mild stage of the disease is best treated.
- Average. The roots of the teeth are exposed by an average of 4-6 mm. The patient begins to experience a burning sensation in the mouth, and there is an acute reaction to eating hot, cold or sour foods.
- Heavy. The roots of the teeth are exposed by 8-10 mm. Chewing food causes severe pain.
Treatment methods
Diagnostics
Before starting treatment for periodontal disease, the dentist conducts an initial examination, during which he determines the extent of damage to the teeth and gums: which teeth can be restored and which will have to be removed. This is necessary in order to draw up an algorithm for further actions. The patient is then sent to the diagnostic room to take targeted and panoramic X-rays. Using them, the periodontist determines the depth of the pockets and the condition of the bone tissue.
Removing plaque and tartar
Inflammation of the gums, which is always observed with periodontal disease, mainly occurs due to soft plaque, subgingival and supragingival calculus. The main reason for their appearance is poor oral hygiene. Therefore, the specialist’s task is not only to treat the disease, but also to teach the patient proper hygiene.
General and local therapy
To increase immunity, the patient is prescribed a complex of vitamins and anti-inflammatory drugs. If the inflammation is minor, the dentist will prescribe a course of local therapy, which can be done independently at home.
Splinting teeth
An increase in tooth mobility indicates that the jawbone and soft tissue around them have begun to rapidly deteriorate. To prevent the teeth from changing position and falling out (for example, they may fan out), they are held together with fiberglass tape and filling material. This is also necessary before surgical treatment.
Surgical operations
If periodontal pockets reach 5-10 mm, it is impossible to prevent the progression of the disease without surgical intervention. First, the pockets are cleaned of granulations and food deposits. This procedure is called curettage. It comes in two types - open and closed.
Closed is carried out with special instruments, curettes. It is carried out only for periodontal disease at the initial stage (pockets reach 3 mm), when there is slight inflammation of the gums.
Open curettage is necessary in advanced stages of periodontal disease. With its help, all granulations and food deposits are completely removed. This operation is more difficult to perform. To completely clean out the pockets, incisions are made in the gum. Flaps of the mucous membrane are peeled away from the bone and the root surface is cleaned with curettes and an ultrasonic scaler. To restore bone tissue, the periodontist implants synthetic bone.
Next, the patient undergoes flap surgery to prevent receding gums. The doctor removes a 1.5 mm marginal strip of gum, since after prolonged inflammation the gum changes in such a way that it can no longer adhere normally to the tooth. After this, the mucous membrane flaps are pulled to the neck of the tooth.
Timely diagnosis and choosing the right treatment will help stop periodontal disease and maintain healthy teeth!