Take the first step
make an appointment with a doctor!
Pregnancy is a happy time in the life of every woman, but, unfortunately, it is often overshadowed by various diseases. These include hepatosis in pregnant women, the symptoms of which most often begin to appear in the third trimester. Just a few years ago, this disease was very rare in medical practice; only one out of 16,000 expectant mothers suffered from it. But recently, an increasing number of pregnant women are faced with this unpleasant disease. Hepatosis in pregnant women is a degenerative liver lesion, manifested in impaired bile formation and bile flow.
Causes of hepatosis in pregnant women
Doctors turned their attention to this disease relatively recently, so experts are still arguing about what causes its appearance. Most medical minds agree that hepatosis in pregnant women is caused by certain genetic characteristics or disorders and can be transmitted through the female line. These genetic abnormalities may not manifest themselves in any way throughout life. But sometimes pregnancy, which brings with it an increase in body weight, hormonal imbalances and an increased load on the body in general and on the liver in particular, gives impetus to the development of hepatosis. The liver is also very susceptible to the influence of pregnancy hormones. For example, estrogen.
The main factors that increase the risk of this disease include:
- Incorrect intake of vitamins. Vitamins are always an additional burden on the liver. Many vitamin complexes contain increased amounts of various components, which cause liver dysfunction, so they need to be taken correctly, taking into account age, body weight, dosage and stage of pregnancy.
- Dietary disorder. Overeating and eating salty, fried, smoked, fatty foods, as well as foods rich in chemical additives, overload the liver and impair its functioning.
- Insufficient physical activity. If the expectant mother moves little, then little energy obtained from food is consumed, and the metabolism, which is already slowed down by pregnancy, slows down.
Take the first step
make an appointment with a doctor!
When to worry
If there is a thin layer of whitish coating on the tongue, but the pregnant body feels well, no accompanying abnormalities are observed, the period of bearing the baby is not complicated in any way, there is no need to worry. If a dense white plaque is visualized, which is accompanied by an unpleasant odor or even pain or discomfort, this indicates a fungal infection of the oral cavity - candidiasis. Also, a dense white coating can appear as a result of insufficient hygiene measures, caries, and gingivitis. In such situations, visiting a doctor is a necessity.
Diagnosis of hepatosis and its signs
Hepatosis in pregnant women is a disease that is sometimes very difficult to diagnose. By this time, the uterus already occupies the entire abdominal cavity, which makes palpation of the liver impossible. This disease is often confused with gallstone disease, because their symptoms are very similar. The most common signs of hepatosis include:
- skin itching;
- yellowing of the skin and whites of the eyes, the appearance of vascular networks on the face and hands, redness of the palms (they seem to be covered with red spots from the inside);
- nausea, vomiting, abdominal discomfort, bitterness in the mouth, stool disorders, loss of appetite;
- pain in the right hypochondrium;
- lightening of stool and darkening of urine (from orange to dark brown);
When the bile duct is disrupted, a large amount of bile accumulates in the liver. Unable to escape, bile begins to break through into the lymphatic system, and from there into the general bloodstream. If you conduct a blood test, it will show an increase in the level of transaminases, alkaline phosphatase, bilirubin and cholesterol, a decrease in hemoglobin, as well as red blood cells and platelets. A urine test will reveal the presence of bile acids and increased secretion of urobilin.
When bile enters the bloodstream, it causes itching, which intensifies in the evening and at night. Most often, pregnant women with this disease consult a doctor with complaints of an acute and irresistible desire to scratch. It drives you crazy, disrupts sleep, leads to fatigue and irritation. As a rule, the arms, legs and stomach itch the most. Filling the liver with bile causes overstretching of its capsule, the surface of which has a large number of pain receptors. This causes constant dull pain in the right side.
If hepatosis is suspected, the doctor at the antenatal clinic should carefully examine the patient, try to palpate the liver area, prescribe extensive blood and urine tests, as well as an ultrasound examination of the liver, gall bladder and neighboring organs.
The problem of jaundice in pregnant women in modern obstetrics
Jaundice refers to the yellow coloration of the skin, sclera and mucous membranes as a result of tissue impregnation with bile pigment - bilirubin. Jaundice in pregnant women occurs with a frequency of 1 in 1500 births and is a symptom of diseases of various etiologies and pathogenesis. In pregnant women, jaundice is most often caused by liver pathology (so-called hepatic jaundice), subhepatic (obstructive) and suprahepatic (hemolytic anemia) jaundice are less common. Jaundice in pregnant women is usually divided into two large groups: I - jaundice caused by pregnancy pathology; II - jaundice associated with concomitant diseases, both acutely occurring during pregnancy and preceding it.
Classification of jaundice in pregnant women
First group. Jaundice caused by pregnancy pathology:
- intrahepatic cholestasis of pregnancy;
- acute fatty liver degeneration in pregnant women;
- jaundice due to gestosis (preeclampsia, eclampsia);
- jaundice due to excessive vomiting during pregnancy.
Second group . Jaundice caused by various concomitant diseases encountered during pregnancy:
- diseases that occur during pregnancy: acute viral hepatitis (caused by hepatitis A, B, C, D, E viruses, as well as yellow fever, Epstein-Barr, herpes simplex types I and II viruses, cytomegalovirus and some others), medicinal, toxic (alcohol, etc.); obstruction of the common bile duct (obstructive jaundice); some bacterial, parasitic infections, sepsis;
- diseases preceding pregnancy: chronic liver diseases of various etiologies, hemolytic anemia, familial non-hemolytic hyperbilirubinemia and some others.
Intrahepatic cholestasis of pregnancy ( ICP) (previously used terms - “cholestatic hepatosis of pregnancy”, “benign recurrent cholestasis of pregnancy”, “adiopathic jaundice of pregnancy”, “pruritus of pregnancy”) is the second most common cause of jaundice in pregnant women (after acute viral hepatitis). , causing up to 20–25% of its cases. The etiology of ICP is unknown; it is assumed that the disease is based on a genetic predisposition to an unusual cholestatic reaction to estrogens produced during pregnancy. ICP is characterized by: onset, usually in the third trimester (less often in the second trimester); an increase in clinical manifestations before childbirth and their disappearance immediately after childbirth; recurrent in nature (not always) with repeated pregnancies; often the presence of skin itching during pregnancy in mothers and sisters. The main clinical manifestation of ICP is itching of the skin, which precedes the appearance of jaundice (jaundice may not develop). Jaundice, as a rule, is not intense, accompanied by darkening of the urine and lightening of the stool. The general condition of the patients does not suffer. Characterized by no more than a 5-fold increase in serum bilirubin levels, an increase in alkaline phosphatase (ALP) levels by 7–10 times, gamma-glutamyltransferase (GGT), and bile acids; a slight increase in the ratio of aspartate aminotransferase and alanine aminotransferase (AST/ALT). Histological changes in the liver represent simple cholestasis. The prognosis of the condition is favorable, however, the frequency of premature births increases, due to impaired absorption of vitamin K, hypoprothrombinemia and an increased risk of postpartum hemorrhage are possible.
Diagnosis of ICP, as a rule, does not cause great difficulties, especially if there is anamnestic evidence of the recurrent nature of cholestasis or hereditary predisposition. The range of conditions for which a differential diagnosis should be made is limited to diseases characterized by cholestasis syndrome: obstructive jaundice, cholestatic form of acute viral hepatitis, drug-induced hepatitis, and some forms of chronic liver diseases. Obstructive jaundice is excluded based on the clinical picture (absence of abdominal pain syndrome in ICP) and the results of ultrasound examination of the biliary tract. Acute viral hepatitis helps to exclude insignificant changes in cytolysis parameters (AST/ALT) and the absence of serum viral markers in ICP. The greatest difficulties are presented by the differential diagnosis of ICP with the onset during pregnancy of previously latent chronic liver disease (CLD) (primary biliary cirrhosis, primary sclerosing cholangitis, chronic hepatitis with cholestasis syndrome). Often, the diagnosis of CKD can be established only after resolution of pregnancy on the basis of the persistence of clinical and laboratory signs of cholestasis, which is uncharacteristic for ICP, and on the basis of a morphological examination of the liver. Carrying out a liver biopsy during pregnancy in such cases, as a rule, is not required, since it does not affect the management of the pregnant woman (in both ICP and chronic liver disease, termination of pregnancy in the third trimester is not indicated; a reduction in the manifestations of cholestasis can be achieved by prescribing cholestyramine).
Acute fatty liver disease of pregnancy (AFLP) - Sheehan's syndrome (previously called "acute fatty liver disease of pregnancy") is a rare complication of pregnancy, occurring with a frequency of 1 in 13,000 births. Etiology unknown; Sometimes there is an association with the use of tetracycline. It usually develops in young primiparous women in the third trimester of pregnancy (from 30 to 38 weeks). Characterized by a sudden onset with vomiting and abdominal pain, then jaundice and fever appear, the development of fulminant hepatic and acute renal failure, blood coagulation disorders (disseminated intravascular coagulation syndrome (DIC) in 75% of patients), gastrointestinal and uterine bleeding; the condition is often combined with gestosis. Laboratory tests are characterized by: leukocytosis up to 20–30 thousand, a significant increase in the level of uric acid in the blood serum, severe hypoglycemia, a significant decrease in albumin levels, a moderate increase in the levels of bilirubin, serum aminotransferases. Histologically, small-lobed obesity of hepatocytes without significant necrosis and inflammation is revealed, however, liver biopsy is usually impossible due to severe blood coagulation disorders. The condition is characterized by high mortality for mother and fetus; the prognosis can only be improved by the earliest possible diagnosis of the condition and delivery (caesarean section under epidural anesthesia). The disease may progress within 1–2 days after delivery, then the condition improves. Repeated pregnancies are not contraindicated, since relapses of AFDP are not observed.
The most important differential diagnosis is with the fulminant form of acute viral hepatitis, since management tactics for these diseases are different. The differential diagnosis is based on the clinical and laboratory features of AFDP (characteristic are the time and symptoms of the onset of the disease, leukocytosis and high levels of uric acid in the blood serum with relatively low levels of bilirubin and AST/ALT), the absence of serum viral markers. Ultrasound examination (ultrasound) of the liver can be useful, revealing a picture of steatosis and a reduced liver size. This study also allows us to exclude the obstructive nature of jaundice, the presence of which may be suspected on the basis of severe abdominal pain and dyspeptic syndromes, leukocytosis.
Jaundice with preeclampsia, eclampsia . In severe gestosis, liver damage is observed, the cause of which is microangiopathy as part of generalized vascular disorders. Histologically, fibrin thrombi are detected in the sinusoids, mainly centrilobular necrosis and hemorrhage; there is no inflammatory reaction.
The appearance of signs of liver damage against the background of a detailed clinical picture of gestosis is typical. As a rule, only laboratory changes are observed (increased alkaline phosphatase, AST/ALT, slight thrombocytopenia). In severe cases, moderate jaundice develops (hyperbilirubinemia within 5-6 times the norm due to conjugated and unconjugated bilirubin), combined with the development of disseminated intravascular coagulation syndrome, intravascular hemolysis, thrombocytopathy, the so-called HELLP syndrome (according to the first letters of the main manifestations - haemolyas , elevated liver enzymes, low platelet colint). Maximum changes in laboratory parameters are observed in the first two days after birth. Clinically, the condition manifests itself, in addition to the symptoms of preeclampsia and eclampsia, by abdominal pain syndrome (in 65–90% of patients), nausea and vomiting (up to 50%), complications of disseminated intravascular coagulation syndrome and may resemble CVD. The condition can sometimes be combined with ACDP, which is proven morphologically by the detection (in addition to the characteristic fibrin thrombi, necrosis and hemorrhage) of small-droplet obesity of hepatocytes. A rare and very severe complication of liver damage in eclampsia is the formation of a subcapsular hematoma with liver rupture and the development of intra-abdominal bleeding.
As with AFDP, the most important differential diagnosis is acute viral hepatitis, which can be excluded by a clear connection of the condition with the progression of gestosis, the absence of a prodromal period, as a rule, a lower level of increase in AST/ALT, and the absence of serum viral markers. Differential diagnosis of severe liver damage in preeclampsia, eclampsia with AFDP can be extremely difficult (especially given the possibility of a combination of these conditions), but it has no practical significance, since in both cases the management of the pregnant woman is the same and consists of urgent delivery .
Jaundice due to excessive vomiting in pregnant women is associated with transient functional changes in the liver caused by malnutrition, protein catabolism, and dehydration. The mechanism of hyperbilirubinemia is not entirely clear. There are no specific histological changes in the liver during vomiting of pregnancy. The development of jaundice is observed in the first trimester of pregnancy against the background of a long period of daily repeated vomiting, weight loss, and dehydration; characterized by a slight increase in the levels of bilirubin (both conjugated and unconjugated), AST/ALT, alkaline phosphatase, a decrease in the level of albumin in the blood serum with a rapid normalization of indicators after cessation of vomiting and restoration of nutrition. The condition usually has a good prognosis and does not require termination of pregnancy. With a typical clinical picture, diagnosing the condition does not cause difficulties. However, with pronounced abnormalities in liver tests, it is necessary to exclude acute viral hepatitis or an exacerbation of unrecognized chronic hepatitis that preceded pregnancy. In difficult cases, when a combination of vomiting of pregnancy and exacerbation of chronic hepatitis is suspected, a puncture biopsy of the liver is indicated, the result of which may affect the management of the pregnant woman (determining indications for termination of pregnancy, for the treatment of CKD).
Among intercurrent liver diseases that occur during pregnancy, the main role in the development of jaundice belongs to acute viral hepatitis (AVH), which causes up to 40–50% of cases of jaundice in pregnant women. AVH can be observed at any stage of pregnancy; its clinical picture is extremely diverse (from anicteric clinically latent forms to severe fulminant hepatitis), which makes differential diagnosis difficult and the need to differentiate AVG from all etiological forms of jaundice found in pregnant women. At the same time, correct and timely diagnosis of OVH is especially important due to the peculiarities of management tactics for pregnant women with this condition. It is known that termination of pregnancy and childbirth aggravate the course of OVH, so management should be aimed at prolonging pregnancy and preventing premature birth.
In the diagnosis of AVH, epidemiological data (risk factors for infection), the presence of a clear prodromal period, a very high level of serum aminotransferases characteristic of AVH, identification of serum markers of hepatitis viruses characteristic of acute infection: anti-HAV IgM in AVH-A may be important; HBsAg, HBcAb total and IgM, HBeAg, HBV DNA in ARV-B; anti-delta IgM, HDVRNA for OVH-D; HCVRNA in AVH-C, anti-HEV in AVG-E (the diagnostic value of anti-HEV has not yet been sufficiently studied), serum and tissue markers of other hepatotropic viruses. It is important to carefully exclude all other possible causes of jaundice in pregnant women.
Chronic liver diseases (chronic hepatitis and liver cirrhosis of various etiologies - viral CKD, autoimmune hepatitis, drug and alcohol liver damage, primary biliary cirrhosis, liver damage due to primary sclerosing cholangitis, Wilson-Konovalov disease and some others) can be latent for a long time or appear only extrahepatic syndromes, which often makes their timely diagnosis difficult. It is not uncommon to observe during pregnancy the manifestation of a preceding but unrecognized CKD.
Primary biliary cirrhosis and primary sclerosing cholangitis are characterized by exacerbation or the first appearance of clinical signs of cholestasis (itching, jaundice) during pregnancy, which is caused by the action of estrogens. Differential diagnosis is carried out with ICP, drug-induced hepatitis, cholestatic form of AVH. In contrast to the cholestatic form of jaundice in some CKD, which is not associated with a risk to the life of the pregnant woman, non-cholestatic (hepatocellular) jaundice during exacerbation of CKD of viral etiology, autoimmune hepatitis indicates severe damage to the liver parenchyma and is an unfavorable prognostic sign (the possibility of developing liver failure , coma). Differential diagnosis is carried out with OVH, ACDP, hemolytic jaundice and other diseases.
CKD can be suspected on the basis of anamnesis, retrospective assessment of some symptoms that could be a manifestation of liver disease unrecognized at the time of pregnancy (AVG, episodes of jaundice in history, the presence of articular syndrome, relapses of vascular purpura or other most common extrahepatic manifestations of CKD), detection of increased dense liver, splenomegaly, signs of portal hypertension characteristic of liver cirrhosis during ultrasound, esophagogastroscopy. In difficult differential diagnostic cases, especially when the result of the study may affect the management of the patient, a puncture biopsy of the liver is indicated to clarify the diagnosis of CKD.
Subhepatic jaundice in pregnant women is most often a consequence of obstruction of the common bile duct; other causes (tumors, strictures) are extremely rare. During pregnancy, bile becomes more lithogenic, and emptying of the gallbladder becomes more difficult; There are observations of the formation of gallstones during pregnancy. Despite this, symptoms of gallstones are relatively rare during pregnancy. Choledocholithiasis accounts for no more than 6% of the causes of jaundice in pregnant women. Obstructive jaundice in cholelithiasis most often develops after an attack of acute pain in the upper abdomen, often accompanied by vomiting and fever; a blood test reveals leukocytosis; there is no stercobilin in the feces or the reaction is weakly positive (with incomplete obturation); bilirubin (bile pigments) is determined in the urine; in the very first days, an increasing biochemical syndrome of cholestasis is noted; cytolytic syndrome (increased AST/ALT) can be pronounced. The development of cholestatic jaundice during pregnancy (even in the absence of a typical clinical picture of biliary colic) always requires the exclusion of the mechanical nature of cholestasis through the immediate use of ultrasound.
Enzymatic hyperbilirubinemias are rarely a problem during pregnancy. In the most common form of enzymatic hyperbilirubinemia, Gilbert's disease, characterized by an increase in the level of unconjugated bilirubin, a decrease in the level of bilirubinemia is observed during pregnancy. This is explained by the induction of hepatic glucoronyltransferase by estrogens. In rare cases, when unconjugated hyperbilirubinemia is first detected during pregnancy, the differential diagnosis should be made with inactive chronic hepatitis, an erased form of hemolytic anemia. Other forms of familial non-hemolytic bilirubinemia are extremely rare in pregnant women. Of these, only in Dubin-Johnson syndrome, characterized by increased levels of conjugated and unconjugated bilirubin, bilirubinemia increases towards the end of pregnancy, and latent forms may first manifest as jaundice during pregnancy. The diagnosis is reliable only when confirmed by liver biopsy data (the structure of the lobules is preserved, in the hepatocytes there are deposits of dark brick-colored pigment).
Prehepatic jaundice (hemolytic anemia) often occurs during pregnancy. Differential diagnosis from other forms of jaundice, as a rule, is not difficult, based on the presence of anemia of varying severity, signs of irritation of the red line of the bone marrow with reticulocytosis, hyperbilirubinemia due to an increase in the level of unconjugated bilirubin (the level of conjugated bilirubin may be slightly increased), dark color of stool due to stercobilinogen, unchanged levels of cholestasis and cytolysis. One should keep in mind the possibility of autoimmune hemolytic anemia against the background of autoimmune hepatitis, primary biliary cirrhosis, and the possibility of developing hemolytic crises in Wilson-Konovalov disease.
Ursodeoxycholic acid is used as the main pathogenetic agent for intrahepatic cholestasis.
Ursodeoxycholic acid is a naturally occurring, non-toxic, hydrophilic bile acid that is part of the human bile acid pool. The mechanisms of action of ursodeoxycholic acid are diverse and not fully understood. The main ones are cytoprotective and choleretic effects caused by changes in the pool of bile acids with ursodeoxycholic acid displacing toxic primary bile acids (such as chenodeoxycholic, deoxycholic, lithocholic), the absorption of which in the intestine is inhibited. In addition, ursodeoxycholic acid has an immunomodulatory effect. It has been shown that its use leads to a decrease in the expression of HLA class I and II antigens on hepatocytes, biliary epithelial cells, and to a decrease in the production of proinflammatory cytokines. Ursodeoxycholic acid also has anti-apoptotic and antioxidant effects. By inhibiting the absorption of cholesterol in the intestine, suppressing its synthesis in the liver and reducing secretion into bile, ursodeoxycholic acid reduces the saturation of bile with cholesterol; it increases the solubility of cholesterol in bile and reduces the lithogenic index of bile.
The use of ursodeoxycholic acid in the third trimester of pregnancy not only relieves itching and improves the mother's condition without causing side effects, but also significantly improves the prognosis for the fetus.
Thus, jaundice during pregnancy can be caused by diseases that differ not only in etiology, but also in severity and, accordingly, prognosis for the mother and fetus. The differential diagnosis of jaundice in pregnant women is extremely important, since management and treatment tactics that ensure a successful pregnancy outcome for the mother and fetus are different for various diseases that occur with jaundice.
Literature
- Kuzmin V.N., Adamyan L.V. Variants of the clinical course, diagnosis and treatment tactics of acute fatty hepatosis in pregnant women // Obstetrics and Gynecology. 2009, No. 1, p. 25–29.
- Kuzmin V.N., Serobyan A.G. Acute fatty hepatosis in pregnant women // Issues of gynecology, obstetrics and perinatology. 2008, vol. 7, no. 1, p. 83–87.
- Sherlock S., Dooley J. Liver during pregnancy. In the book: Diseases of the liver and biliary tract. M., 1999, p. 540–549.
- Shekhtman M. M. Extragenital pathology and pregnancy. Medicine, 1987. 295 p.
- Aggarwal R., Ranjan P. Preventing and treating hepatitis B infection // BMJ. 2004. Vol. 329. P. 1080–1086.
- Gambarin-Gelwan M. Hepatitis B in pregnancy // Clin Liver Dis. 2007 Nov; ll(4):945–63.
- Riely CA Liver disease in pregnant patient // Am. J. Gastroenterol. 1999. Vol. 94. P. 1728–1732.
- Steven MM Pregnancy and liver disease // Gut. 1981. Vol. 22. P. 592–614.
- Lorente S., Montoro MA Cholestasis of pregnancy // Gastroenterol Hepatol. 2007, 30 (9), p. 541–548.
- Pusi T., Beuers U. Intrahepatic cholestasis in pregnancy // Orphanet. J. Rare. Dis., 2007, 2, p. 26.
V. N. Kuzmin , Doctor of Medical Sciences, Professor
MGMSU, Moscow
Contact information about the author for correspondence
Painful attacks during hepatosis
In the most difficult cases of hepatosis, the patient sometimes experiences attacks characterized by severe pain in the right hypochondrium. Often the pain is felt in the abdomen, at the level of the navel and is mistaken for an exacerbation of gastritis. Such attacks may be accompanied by continuous and painful vomiting without relief, headache, tinnitus, rapid heartbeat, darkening of the eyes and shortness of breath. They are very similar to severe poisoning syndrome, only in this case the stool practically does not change, and the food eaten is vomited.
Most often, such attacks are caused by eating harmful foods (fried, spicy, fatty, alcohol) and begin 40-60 minutes after eating or by a sudden movement, for example, a quick turn, bend or fall. Painful attacks can last up to 20-40 minutes, they begin suddenly and recede just as sharply. Often after an attack, quite severe residual pain remains in the right hypochondrium for several days. A big mistake during such attacks is taking paracetamol, because it only aggravates the situation, negatively affecting liver activity. It is allowed to take antispasmodic drugs such as No-Shpa.
Take the first step
make an appointment with a doctor!
Signs of pregnancy while breastfeeding
Many women mistakenly believe that it is impossible to get pregnant while breastfeeding. This is wrong.
Let's look at the signs that may indicate that a nursing mother is pregnant again.
If your baby refuses to breastfeed for no apparent reason, consider purchasing a pregnancy test. The fact is that a new pregnancy provokes a change in the taste of breast milk, which acquires a bitter taste and becomes less sweet.
The consistency of the milk itself may change, as well as its quantity (up to its complete disappearance).
You should also pay attention to persistent hypersensitivity, as well as soreness of the nipples, especially if such signs were not previously observed during breastfeeding.
Darkening of the skin around the nipples may also indicate pregnancy.
The absence of menstruation, provided that it has already occurred after childbirth, can also be a sign of pregnancy.
The danger of hepatosis during pregnancy
The affected liver is not able to cleanse the body of harmful substances, which leads to intoxication of the mother and a deterioration in her well-being. Surprisingly, from the very first day after birth, the disease begins to quickly recede and soon leaves no trace behind. After 1-2 weeks, blood counts return to normal. Even if hepatosis recurs in several pregnancies in a row, it does not make any visible changes in the woman’s liver. However, this does not mean that this disease is harmless. It disrupts the metabolism between mother and fetus, thereby adversely affecting the child. It has been proven that hepatosis increases the likelihood of perinatal mortality by 5%, and in 35% of pregnancies occurring against the background of this disease, hypoxia, prematurity and delay in fetal development were observed.
External signs of pregnancy
A change in a woman’s appearance already in the early stages may indicate pregnancy.
Acne during pregnancy
A sharp hormonal change in the body of a pregnant woman and increased activity of the sebaceous glands can trigger the appearance of acne, even if the woman has not previously encountered this problem.
Most often, the rash goes away after the baby is born and does not require any treatment.
If a pregnant woman decides to deal with rashes before delivery, then she should remember that during this period it is forbidden to use drugs that contain retinoids and salicylic acid. In addition, removal of rashes using laser, deep peeling, or mechanical cleaning is contraindicated. Phytotherapeutic procedures should also be treated with caution.
Facial redness during pregnancy
Such an early sign of pregnancy as facial redness is associated not only with hormonal levels, but also with increased blood circulation during this period.
Many pregnant women experience the so-called “pregnant mask”, which is characterized by the appearance of age spots localized in the forehead, cheeks and nose. You should not be afraid of such spots, since after childbirth they will go away on their own over time.
Veins during pregnancy
The onset of pregnancy may be marked by the appearance of venous patterns (or spider veins) on the chest, neck, arms and legs. Such spider-like patterns of dark red or bluish color, like skin pigmentation, will disappear on their own with the birth of the child.
Edema during pregnancy
In the early stages of pregnancy, slight puffiness of the face may be observed. In addition, your hands may swell, which is especially noticeable if you clench your hand into a fist.
It should be remembered that swelling in the first months of bearing a child is not normal and may indicate that the expectant mother has kidney disease or cardiovascular disease. Therefore, if this symptom appears, you should consult a doctor.
Breast enlargement during pregnancy
Many women, due to the absence of menstruation, may suspect pregnancy in the first weeks of conception due to breast enlargement by 1 - 2 sizes. Moreover, this sign can be observed even if a woman loses her appetite and loses weight.
Breast enlargement may be accompanied by pain and tingling in both mammary glands.
Important! During pregnancy, both breasts increase in size exactly the same. Enlargement of one mammary gland or any part of it should alert you, as it may signal the presence of serious diseases.
Nipple changes during pregnancy
Early signs of pregnancy are darkening and swelling of the nipples, as well as the appearance of Montgomery tubercles - small outgrowths localized in the nipple area. Outwardly, such formations resemble small warts that are filled with a sebaceous substance.
There is no need to worry about the appearance of such tubercles, since they in no way disrupt the functioning of the sebaceous glands and do not affect the health of the expectant mother, much less the fetus.
Pain and burning sensations that occur when touching the nipples may also indicate pregnancy.
Discharge from the breast during pregnancy
An early (albeit rare) sign of conception may be clear fluid released from the nipple when pressure is applied to it.
Sometimes, in early pregnancy, colostrum may begin to be released, which indicates galactorrhea, a condition in which there is increased production of the hormone prolactin.
In general, the appearance of colostrum is more typical in the second and third trimesters of pregnancy.
Stripe on the stomach during pregnancy
Many people believe that a brown line on the abdomen, running from the navel down, appears in late pregnancy. In fact, this line can be seen already in the first weeks of pregnancy, it will simply be white, whereas from the 12th week it will begin to acquire a brown tint.
Treatment of hepatosis in pregnant women
Treatment of hepatosis is complicated by the fact that almost all medications are contraindicated for pregnant women. Many medications can cause hypoxia and intrauterine growth retardation in the fetus, so the doctor must conduct a full examination of the patient and make sure the diagnosis is correct before deciding on a treatment method. It is very important to understand at what stage the disease is. In the mild stage, you can do without drug intervention by using a special diet. The expectant mother should exclude all heavy, fatty and high-calorie foods from her diet, and also stop taking vitamin complexes and other medications (if their withdrawal does not harm the pregnancy). Drugs designed to optimize liver function are also often prescribed (Hofitol, Essentiale Forte N and others). In many cases, diet is enough to remove toxins from the body and improve the patient's condition.
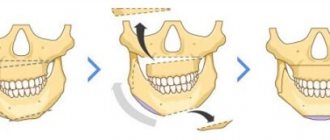
In more severe stages, the woman is sent to a hospital, where the issue of early delivery is decided. If there is no danger to the fetus, then labor can be delayed by purifying the blood using IVs. They are combined with taking large doses of the above-mentioned drugs and a strict diet. If this technique makes it possible to suppress the disease or at least keep it at the same level of development, and the condition of the fetus does not cause concern, then treatment is continued until 37-38 weeks, and childbirth is planned for this period. If the method does not give the desired result (or if the condition of the fetus worsens, hypoxia is clearly visible), consent to induced labor or Caesarean section is urgently signed. Often the child has a defensive reaction to the unfavorable situation created, and premature birth spontaneously begins. However, you should not rely only on nature. If serious indications arise, it is recommended to start the labor process in advance to minimize the risk of complications.
It is very important that a pregnant woman with severe hepatosis is under constant medical supervision. It is also necessary to carry out extensive blood tests every two days. It often happens that under the influence of IVs, blood counts suddenly drop significantly. Having decided that the disease has subsided, the doctor discharges the patient, and after a couple of days she is again admitted to the hospital with a sharp increase in transaminases.
Take the first step
make an appointment with a doctor!
Signs of the first and second pregnancy
Are the early signs of the first and second pregnancy different? We answer: everything is purely individual. There are many cases where the same woman’s first pregnancy occurred against the background of severe toxicosis, while bearing a second child did not cause any problems.
In general, gynecologists identify the same early signs of pregnancy, regardless of whether it is the first, second or third. However, pathologies such as hemorrhoids and varicose veins during the second and subsequent pregnancies become aggravated already in the first weeks of gestation.
Prevention of hepatosis in pregnant women
Although hepatosis is considered the result of certain genetic characteristics, there are a number of recommendations to avoid it or delay its appearance for a longer period:
- Dieting. If you have a tendency to overload the liver, then you must completely avoid everything fried, fatty, smoked, salty, spicy and sour. The diet should consist of fruits, vegetables (except potatoes, legumes, onions and garlic), low-fat dairy products, chicken breast meat, and low-fat fish. You should not eat chocolate and other cocoa-containing products, egg yolks, cheese, pastries (1-2 pieces of black bread per day are allowed).
- Physical activity. Movement is life, so you need to move more. This speeds up metabolic processes in the body, eliminates congestion, and facilitates the functioning of the liver.
- Refusal of oral hormonal contraceptives and antibacterial agents. They can cause great harm to the liver.
- Take vitamins carefully or avoid them. If possible, you should try to get all the substances the body needs from food, and not from vitamin complexes.
- Treatment of chronic gastrointestinal diseases.
- The use of hepatoprotectors and choleretic drugs. If pregnancy is not planned yet, then it is enough to carry out preventive courses with these drugs, and if pregnancy has already occurred, then they must be taken according to a special schedule agreed with the attending physician.
Hepatosis in pregnant women is a very insidious disease. If you suspect you have signs of it, be sure to tell your doctor so that he can order a blood test and make or rule out a diagnosis.