Bone exostosis or osteochondroma is the most common skeletal tumor. It accounts for about 20% of all cases of the formation of bone tumors and almost 40% of the development of all benign bone tumors. Most often it is detected before the age of 20, although it is usually asymptomatic. Only in isolated cases does pain and other disorders occur. Nevertheless, the formation of a growth on the bone necessarily requires consultation with a doctor, since malignancy or malignancy of osteochondroma is rare, but still possible.
What is bone exostosis
Osteochondral exostosis is a benign osteochondral formation on the outer surface of the bone. Most often, it is detected at a young age before the end of skeletal growth, including in children.
The formation of osteochondroma provokes a disruption of the natural processes of resorption (resorption) and the formation of new bone tissue (remodeling).
Exostosis is a growth formed by spongy bone and having a cortical layer (a strong, hard “shell”). It can grow on a stalk or be attached to a bone with a wide base. On the outside, the bone growth is covered with cartilage tissue, which has much in common with articular cartilage. Its thickness does not exceed 1 cm. The top layer of exostosis is also called a cartilaginous cap.
Osteochondroma is a consequence of impaired bone growth in the area of the epiphyseal plates, i.e., their displacement from the anatomically correct position with the “throwout” of cartilage tissue to the side. Subsequently, just like the metaphysis, it ossifies in the direction from the base to the apex, which leads to the formation of bone exostosis with a cartilaginous cap. At the same time, it continues to increase in size until the growth zones close, and can appear in absolutely any bone. The bony part of osteochondroma is formed from unevenly distributed bone beams. Between them there is adipose tissue with islets of hematopoiesis. Bone septa are formed due to enchondral ossification of cartilage. This raises the possibility of the presence of calcifications in the cancellous bone.
The metaphyseal areas of long tubular bones are most often affected:
- femoral (30%);
- shoulder (10-20%);
- tibial (15-20%).
Metaphysis (sometimes neck) is a small part of a tubular bone that is located between its epiphysis (head) and diaphysis (body). At 18-25 years of age, it stops growing and ossifies, which indicates the completion of bone formation.
Thus, articular exostosis is often observed - the formation of a growth on the upper (proximal) part of the tibia or lower (distal) part of the femur, i.e. the tumor is localized just below or just above the knee. Damage to flat bones, i.e. exostosis of the rib, scapula, pelvic bones, are less common. Osteochondromas of the bones of the fingers, toes, and clavicle are diagnosed even less frequently. The most rare occurrence is the formation of bone growths in the spine.
Also, bone exostosis can form on the lingual or buccal surface of the jaw. At the same time, it can take the form of a ridge, protrusion, mound, or take on bizarre shapes. In such cases, patients are advised to consult a dentist.
Treatment
The doctor chooses the optimal treatment method in a particular situation after a thorough diagnosis. It includes visual inspection, palpation, x-ray and microscopic examination.
Medication
It is impossible to completely eliminate the tumor with medication. The main goal of drug treatment is to stop its growth. It is also prescribed after surgical interventions to accelerate tissue regeneration.
The most commonly used antiseptic drugs are:
- Dimexide;
- Polycresulene;
- Chlorhexiine;
- Resorcinol.
All of the listed remedies are external, prescribed in the form of ointments, rinses, irrigations or applications.
It is impossible to completely eliminate a tumor with medications
Are traditional methods effective?
Folk remedies are effective only for preventing the development of infection, as well as for accelerating tissue healing after surgery. Among them, for example:
- Infusion of calendula, sage, chamomile, eucalyptus. 15 grams of the mixture is poured into a glass of boiling water and used for rinsing 4-5 times a day.
- A tablespoon of soda is dissolved in 0.5 liters of warm water. Rinse up to eight times a day.
- A tablespoon of iodized salt is dissolved in 0.5 liters of water until the crystals disappear. Use for rinsing three times a day.
Surgical treatment of epulis
The optimal method of treatment is removal of the tumor, which is performed using a surgical or laser scalpel. The doctor makes an incision and completely removes the tumor, often including the periosteum. The edges of the wound are closed, the area is treated and covered with a sterile napkin.
Sometimes adjacent teeth may also need to be removed. This situation occurs due to their increased mobility. During pregnancy, operations are usually not performed unless there are critical and urgent indications.
The optimal treatment method is removal of the epulis
Using laser
Recently, a laser scalpel is often used for dental operations, including the removal of epulis. This solution can be considered optimal for several reasons:
- the edges of the wound are cauterized directly during surgery;
- disinfection occurs at the same time;
- The time of the operation itself and the rehabilitation period are reduced.
Exostosis in a child
It is in children that osteochondroma is most often first diagnosed, which is due to its formation from cells of the epiphyseal plate that is present only until the end of the growth period, which is adjacent to the metaphysis. It is also called the bone growth zone, since it is a hyaline cartilage whose cells are in constant miotic division. As a result, new chondrocytes (cartilaginous tissue cells) are formed, forming the epiphyseal plate, and the old ones are shifted to the metaphysis and subsequently replaced by osteoblasts (bone tissue cells).
In infants, violation of the rules for the prevention of rickets, in particular excessive use of vitamin D preparations, increases the likelihood of the formation of exostoses.
After puberty, the growth plates gradually close and are replaced by bone tissue, transforming into a thin epiphyseal line. If hormonal imbalances occur during this period, it is possible that the growth zones may remain open, which creates the preconditions for the formation of osteochondromas.
Usually, until the age of 7-8 years, bone exostosis does not manifest itself in any way in a child and makes itself felt only during the period of intensive growth, i.e., at 8-16 years, since it also begins to grow actively. In young children, such growths are present in the metaphysis area immediately near the epiphyseal plate, but subsequently move away from it and approach the diaphysis. Therefore, by how far the bone exostosis in children is from the epiphysis, the time of its formation is determined.
The growth of the neoplasm continues until the end of the growth period.
Why does exostosis occur on the gums after tooth extraction?
The cause of the growth is excessive growth of bone tissue. This mechanism is triggered when they are damaged, which occurs during the extraction of teeth or a jaw fracture. Usually bones are injured during complex operations to extract molars. After wisdom tooth removal, exostosis is diagnosed more often than other cases.
Factors that provoke pathological bone growth:
- hereditary predisposition;
- infections, inflammation in the oral cavity;
- injuries during dentofacial operations;
- endocrine disorders.
After tooth extraction, the patient may feel small nodules with his tongue. Over time, they increase in size and cause concern.
Types and stages of development
Exostosis can be present only on one bone, i.e., be solitary, or affect all metaphyses of the bones of the skeleton. In the second case, they talk about a generalized form of the disease, which is more common in men and is mainly hereditary. It is also called multiple exostotic chondrodysplasia. In this case, several bones or the vast majority of them are affected, but the formations have different shapes and sizes.
Depending on the shape and direction of growth, there are:
- hilly;
- linear;
- spherical exostoses.
Single exostoses have a narrow or wide base, while multiple ones are usually spherical or oval growths measuring 2-12 cm, sometimes more.
In its development, any osteochondroma goes through 3 successive stages:
- the formation of cartilaginous exostosis, which is not determined by palpation (palpation);
- ossification and active growth of growth;
- stopping the growth of the bone part of the neoplasm while maintaining the possibility of increasing the size of the cartilaginous cap.
Bone exostoses can already be felt during examination and can lead to discomfort, pain during physical activity and other symptoms.
Based on the nature of development and clinical picture, osteochondromas are divided into the following types:
- With normal growth rate. The osteochondral formation grows slowly, and there is a correspondence between the growth rate of the cartilage and the affected bone. Such osteochondromas have the most favorable prognosis, since after the end of the growth period they do not tend to continue to grow and almost never become malignant.
- With a high growth rate. An increase in the size of the growth occurs due to the proliferation of cartilage tissue and can also continue after the completion of the formation of the skeleton due to the preservation of the growth zone. In such cases, removal of exostosis is indicated, since there is a fairly high risk of malignancy.
- Malignant exostosis has the most unfavorable prognosis. Most often, osteochondral neoplasms of the ribs, pelvic bones, scapula and spine degenerate into chondrosarcoma or osteogenic sarcoma.
Kinds
Tumors are classified depending on their etiology, size, and structure.
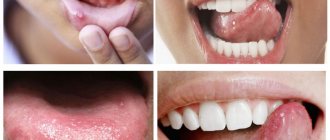
Fibrous epulis
The fibrous formation usually has a hard consistency and is distinguished by the presence of a wide base. The color is most often identical to the gingival tissue; bleeding does not occur spontaneously and can only appear due to mechanical damage (for example, with a hard toothbrush).
The surface has no characteristic features - it can be flat and smooth or bumpy and rough. The most common location is the vestibular surface in the premolar area. There is no pain, the tumor grows in size very slowly.
giant cell
This type most often occurs in elderly patients. Its main manifestations:
- localization – alveolar ridge;
- bleeding on palpation;
- painful sensations;
- color – bluish with a brown tint;
- loosening of adjacent teeth;
- dense, elastic consistency.
This type of tumor is more prone to malignancy than others.
The tumor grows in size very slowly
Angiomatous
Most often develops in children and adolescents. Characteristic features:
- localization – in the area of the tooth neck;
- the tumor is riddled with blood vessels and has a bright red tint;
- the base is wide;
- bleeds when pressed;
- education is soft.
This type is characterized by rapid growth in a short time, and relapses occur frequently. If epulis forms in babies, it can cause delayed teething or the formation of an abnormal bite.
Acanthomatous
Epulis in this form is typical for dogs and cats, but it rarely occurs in people. This is a benign formation that arises from tooth buds, usually on the lower jaw. It looks like small bubbles on the mucous membrane, prone to reappear after removal.
In most cases, formations are benign in nature
Causes of exostosis
There is still no consensus on the reasons for the appearance of exostoses. A number of authors believe that they are of a tumor nature. But most agree that they are a consequence of disorders of enchondral ossification processes that arise as a result of dysembryogenesis (disorders of embryonic development). Therefore, today the main theory of the formation of bone exostoses is the displacement of the epiphyseal plate during intrauterine development of the fetus. It is a bone growth zone located directly below the epiphysis and is responsible for its lengthening. Therefore, the disease is considered congenital, and its development continues throughout the entire period of growth.
The following can increase the risk of osteochondroma:
- ionizing radiation (in 10% of cases the disease develops in patients who underwent radiation therapy in childhood);
- disturbances in the functioning of the endocrine system, taking hormonal drugs;
- smoking and alcohol abuse of parents.
The disease can also be hereditary and transmitted to the child from one of the parents. Especially often, multiple bone lesions due to exostoses are genetically determined.
The acquired nature of the disease cannot be ruled out. The following can provoke the appearance of neoplasms:
- bone injuries;
- microtraumas caused by excessive physical activity, which is typical for professional sports;
- infectious diseases and chronic inflammatory processes of any localization (for example, a heel spur often develops against the background of plantar or plantar fasciitis);
- pathologies of the periosteum, degenerative-dystrophic diseases of cartilage, ankylosing spondylitis;
- microcirculation disorders in soft tissues;
- muscle dystrophy;
- obesity;
- severe forms of allergic diseases;
- compression of the limbs, including an incorrectly applied plaster cast or tourniquet.
Wearing improperly selected clothing and shoes, in particular frequent hypothermia of exposed areas of the body, increases the risk of developing bone tumors.
Of particular importance in the development of osteochondroma is hormonal imbalance in children during puberty. Often the formation of bone exostoses is observed against the background of increased synthesis of sex hormones in adolescents. This can provoke the growth zones to remain open, which can subsequently cause gigantism. Also, an increase in the size of osteochondral exostoses can continue after the closure of growth plates in women as a result of hormonal changes.
Causes
The question of the etiology of osteochondromas remains open to this day. A number of authors do not recognize the tumor nature of osteochondromas, but consider it as a violation of the process of enchondral ossification (as a result of dysembryogenesis ). Many authors are inclined to believe that the appearance and development of osteochondroma is associated with a congenital pathology, the development of which continues throughout the entire period of bone growth (that is, the epiphyseal plate is displaced during the formation of the child’s bones even during the intrauterine formation of the skeleton).
Factors that increase the risk of its development include:
- Ionizing radiation.
- Severe bone bruises and fractures.
- Disruptions in the endocrine system.
- Infectious diseases.
Symptoms
The clinical picture depends on the form of the disease, location, size, shape of exostoses, and the degree of their influence on surrounding tissues. Single neoplasms are usually immobile and their growth is slow. Therefore, in most cases they are asymptomatic and there is no pain. The condition of the skin with solitary exostoses is usually not changed.
But in some cases, there is active growth and acquisition of large osteochondromas. They can mechanically compress blood vessels, nerves, and joints passing near them and provoke the development of reactive bursitis and myositis. This is accompanied by the appearance of pain of varying severity, swelling, redness of the tissues, and sometimes a feeling of numbness. If joint exostosis is present, the range of motion may be limited.
What symptoms exostosis will have depends largely on its location. With multiple exostoses, often the first signs of the disease are stunted growth, valgus deformity of the knee joints and clubhandedness. Fractures of the osteochondroma pedicle may also occur.
Diseases in which a lump on the gum is accompanied by pain
But the situation is much more complicated when the appearance of periodontal compaction is accompanied by severe pain. In such cases, we are talking about more serious diseases. If a tooth hurts and a lump appears on the gum: what could be the reason?
Periostitis
If periodontitis is not treated on time, the pus, instead of coming out through the fistulous tract, can go into the bone, causing its inflammation - periostitis (popularly known as gumboil). This disease has a more severe course: the temperature rises, swelling of the oral mucosa spreads to the soft tissues of the cheeks and lips, the lymph nodes become inflamed, and the person experiences acute, twitching pain. Such a lump can also form as a result of tooth extraction.
Attention!
Flux is a dangerous purulent disease, which, if delayed, can lead to inflammation of the jaw bone, phlegmon and sepsis. At the first signs characteristic of periostitis, you need to urgently contact a dental clinic!
Periodontitis
Periodontitis is a rapidly developing gum disease that leads to the destruction of the tissues that support the tooth. The reasons are the formation of tartar, lack of vitamins in the food consumed, and improper load on the teeth when chewing. The gums begin to bleed, itching appears, the teeth become loose, and gaps form between them. Then, in advanced cases, periodontal pockets appear between the tooth and the tissue, bad breath due to the release of purulent exudate, the necks of the teeth become exposed, and pain occurs when eating cold, hot, sour and salty foods. Due to the accumulation of pus in the pockets, the gums become covered with light-colored small bumps - a breeding ground for pathogenic bacteria. The appearance of such symptoms is a good reason to urgently contact a dental clinic: delay will lead to tooth loss.
Gingivitis
If bright red bumps appear on the gums, small in diameter, the gums bleed and are slightly hyperemic, we may be talking about hypertrophic gingivitis - the initial form of the inflammatory process of periodontal tissues. The disease occurs due to poor quality oral care and, in the absence of timely treatment, leads to serious complications, including periodontitis.
Important! Any pathology associated with the oral cavity can lead to serious health consequences. You should visit a dentist not only for treatment, but also for disease prevention!
Exostosis of the knee joint
It may be caused by the formation of a growth at the end of the tibia and or femur. Exostosis of the tibia provokes severe deformation of the knee joint and is easily detected with the naked eye. Upon palpation, it is possible to detect a dense but painless formation under the skin, which can be either smooth or rough. Reaching large sizes, it provokes pain in the knee when walking (especially often in women who tend to wear high-heeled shoes). In this case, exostosis of the joint tends to injure the adjacent soft tissues, which provokes the development of tendonitis (inflammation of the tendons) and bursitis (inflammation of the synovial bursa).
Damage to the femur in the early stages of development is asymptomatic. But when the tumor reaches a large size, pain in the thigh and dysfunction of the affected limb may occur. Often there are many areas of deformation up to the covering of its entire surface. Since the femur is located deep in the soft tissues, it is difficult to detect exostoses during palpation.
PREPARATION
Surgical intervention is the only option for removing a growth of bone or cartilage tissue from the surface of the jaw row, and therefore requires careful preparation to ensure a favorable outcome.
During the patient’s initial appointment, the dentist clarifies his complaints and conducts a visual examination of the oral cavity in order to identify visible pathologies. At this stage, a number of concomitant diseases are often identified: caries, gum or periodontal inflammation, which require treatment.
To determine the exact location of the growth, its shape, size and nature, the specialist sends the patient for an x-ray examination. The completed image is the basis for making an accurate diagnosis and drawing up a treatment plan.
At the stage of preparation for surgery, the dentist directs the patient to undergo tests, which can be used to identify additional diseases that impede the procedure. Thus, mandatory steps include checking blood for clotting and sugar levels, assessing the balance of hormones and the functioning of the adrenal glands.
At the preparatory stage, the specialist also decides on the option of administering an anesthetic drug.
Surgery to remove exostosis is often performed using local anesthesia, but in some situations general anesthesia may be required.
Before administering it, the specialist checks with the patient for the presence of an allergic reaction and previous experience with pain relief.
Exostosis of the calcaneus (calcaneal spur)
This is a well-known type of osteochondroma. The growth can take on different shapes, which determines the characteristics of the symptoms that arise. With a spherical or mushroom-shaped neoplasm, after it reaches a size of 3-4 cm, pain appears when walking and the inability to fully step on the foot. Since the growth is located in an area that is constantly subject to friction from shoes, the skin in its projection gradually becomes coarser and thickens. A characteristic symptom is an increase in pain in the morning and a gradual decrease in its severity during the day. In the evening, swelling of the lower extremities is often observed.
Reasons for appearance
The causes of a tumor are both external influences and internal processes in the body. The most common:
- injury to the mucous membrane by an overhanging filling or fragments of teeth;
- tartar in advanced form;
- defect of the denture, lack of timely correction;
- soft tissue bruise;
- uncorrected malocclusions;
- chemical, thermal burns.
Even with these factors present, not everyone develops epulis on the gums. Hormonal imbalance is considered a provoking prerequisite for its appearance, so the disease often occurs in adolescence, during pregnancy or menopause.
Spinal exostosis
The lesion can occur at any level, but the thoracic region is most often affected. The neoplasm is located in the area of the arches or processes of the vertebrae. It can grow towards the vertebral or spinal canal or in an anterior direction. The first option is more dangerous, since it is capable of mechanically compressing the spinal cord and the nerve roots extending from it. This provokes the development of the so-called radicular syndrome with sharp, severe pain, radiating in accordance with the level of damage to the body part, impaired sensitivity and mobility.
Reasons for the formation of bumps on the gums
To find out why a lump appeared on the gum, you need to make a correct diagnosis; only a specialist can do this. There are several reasons why swelling appears, but none of them are harmless. When diagnosing, the nature of the formation, color, density, presence or absence of pain, purulent exudate is taken into account, and the nature of the disease is clarified - infectious or other.
Important! Basically, most dental problems are associated with poor oral care. As a result, mucosal pathology develops with its own symptoms.
The reasons why a lump appears between the gum and cheek may be the following:
- irregular and illiterate oral care, resulting in infection affecting periodontal tissues;
- complications of untreated caries - infectious lesions of the roots (fistula, periostitis);
- periodontitis;
- complications resulting from dental implantation;
- improper wearing or manufacturing of orthopedic structures;
- cystic formations;
- gingivitis;
- periodontal trauma (hematoma);
- benign neoplasms (epulis, fibropapilloma);
- malignant tumors.
There is another reason for the occurrence of periodontal compaction. If a child has a white bump on his gum, this may indicate the eruption of a new tooth. Short-term swelling is not terrible, but if after a long time the tooth does not appear, you should consult a surgeon.
Attention!
Many are in no hurry to go to the doctor, since the growth does not hurt. The absence of discomfort does not indicate the absence of disease. Remember: if a lump appears on your gum, only a doctor will determine what to do and how serious the consequences will be!
Exostoses of the ribs
The formation of growths on the ribs is more often observed with curvatures of the spine, which also lead to deformation of the chest. Their growth causes fixation of the pathological position of the chest and limitation of the vital volume of the lungs. As a result, respiratory function disorders may occur, which provokes the appearance of signs of hypoxia (oxygen starvation). To a greater extent, the lack of oxygen affects the brain, which can be accompanied by dizziness, headaches and other disorders. The heart, liver, spleen, and other internal organs are also sensitive to changes in the gas composition of the blood.
Classification
The classification is based on several characteristics. Based on quantitative characteristics, solitary (single) and multiple (generalized) forms are distinguished.
According to the stages of osteochondroma formation:
- The neoplasm is formed from cartilaginous tissue and cannot be detected by palpation.
- Ossification of the growth and its increase. The bone tissue is covered with cartilage, and active growth continues.
- The growth of the bone part of the tumor stops, but the growth of the cartilaginous “cap” of the tumor may continue. Determined by palpation examination. During physical activity, it can manifest as pain and impaired limb function.
Based on the shape and direction of tumor growth, there are hill-shaped, linear and spherical exostoses.
Exostosis of the humerus
The humerus is one of the most common sites of osteochondroma. During its formation, the following may be observed:
- dull pain in the shoulder area that occurs when moving the arm with a large amplitude;
- a feeling of stiffness in movements, present mainly in the morning, until you manage to warm up;
- limited mobility of the upper limb in the shoulder;
- dystrophy of the muscles of the shoulder and forearm, which in difficult cases can be seen with the naked eye.
What it is
Epulis is a tumor-like neoplasm that develops on the alveolar process of the jaw. It also has other names - epulid, supragingival, giant cell granuloma. More often it is localized in the area of incisors, canines and small molars of the upper jaw, less often the tumor is detected in the lower jaw. The growth has a round or irregular shape and a wide stalk; the size of the formation varies from 3 mm to 5 cm.
Despite the fact that such a tumor looks frightening, it practically does not cause concern to the patient, unlike, for example, a burn, with the exception of a violation of aesthetics and the sensation of a foreign body in the oral cavity. Large tumors may cause difficulty chewing and swallowing food.
If epulis is accompanied by bleeding, infection may occur, which will lead to complications.
The disease mainly affects adults, but the neoplasm can also appear in children; in the latter, it occurs during teething. Studies have shown that women are more susceptible to developing epulis than men.
Complications
Cartilaginous exostosis in children has a dangerous negative impact on the condition of the growth plates, which can result in shortening of the lower leg, thigh, forearm, shoulder, etc. This can also cause curvature of the arms and legs, increase the risk of fractures and cause disability.
Patients with severe forms of the disease feel inferior, which negatively affects their mental and emotional state.
The most dangerous complication of osteochondroma is its malignancy, i.e. transformation into a malignant tumor - chondrosarcoma. The highest risk of malignancy is with multiple exostoses. In this case, growths localized in the pelvic bones are more likely to undergo malignancy. Less commonly, exostoses of the ribs, scapula, and spine turn into malignant neoplasms. Single osteochondromas transform into a malignant tumor in no more than 1% of cases.
Atypical growth can be observed in any part of the exostosis: the cartilaginous cap, at the base or in the middle part.
Preventive actions
Monitoring the condition of the teeth and oral cavity will reduce the likelihood of tumors.
- Timely sanitation of the oral cavity. Visiting the dentist for a preventive examination and professional hygiene twice a year will prevent the growth of caries, the appearance of defects in fillings and the formation of tartar, leading to gum injury and the appearance of epulis.
- Prevention of gum injury. If systematic injury to soft tissue occurs as a result of poorly fitted orthopedic or orthodontic structures, consult your doctor about this problem. He will adjust the crowns or dentures.
If these preventive measures are followed, the prognosis is favorable and epulis does not recur.
We hope that our article about epulis will be for informational purposes only. And if you want to soothe your gums, make them strong and strong, try the unique two-component mouth rinse ASEPTA ACTIVE.
This is the only rinse with a combination of chlorhexidine + benzydamine for the treatment of inflammatory periodontal diseases. The product has a combined effect: antimicrobial, anti-inflammatory and analgesic. Instant anesthetic effect allows you to quickly reduce pain.
Diagnostics
Diagnosis of bone exostoses is not difficult. If these symptoms occur, you should consult an orthopedist. Based on the patient’s complaints, medical history and examination results, the doctor can already assume the presence of a neoplasm.
To clarify its size and other features, radiography is prescribed. It is carried out in 2 projections. Osteochondroma on x-rays is visualized as a shadow with smooth, clear contours and a pedicle or wide base connected to the bone. If there is no calcification in the cartilaginous layer, it will not be visible on x-ray.
To obtain additional data, the following may be assigned:
- CT scan, which makes it possible to detect the presence of bone marrow contents in exostosis and trace its connection with the medullary canal of the affected bone;
- MRI, which provides accurate data on the thickness of the cartilage cap and thereby clarifies the nature of the neoplasm (malignant tumors are characterized by a thickness of the cartilage tissue covering them of more than 2 cm).
If there is a suspicion of the development of oncology, patients are advised to undergo a biopsy - taking a fragment of exostosis for histological examination. In this way, benign osteochondroma is differentiated from malignant neoplasms.
If exostoses are detected in childhood and adolescence, it is imperative to conduct a full endocrine examination and determine the content of all significant hormones in the blood.
A growth has appeared on the gum: what is the reason?
A lump or growth is a compaction on the gum caused by damage to periodontal tissue, which may appear without any previous signs. Growths appear in people of any age, but mainly in young children, as they unknowingly introduce infection into their mouths. The first thing you need to do when you detect formations in your mouth is to determine the nature of their origin (only a doctor can do this). It comes in two types:
- Infectious. The appearance of cones is caused by the activity of bacteria.
- Non-infectious. Bumps and growths as a result of injury, mechanical or chemical damage.
If a lump has formed in your mouth, you should consult a doctor to rule out possible complications. The doctor will help diagnose the problem and prescribe appropriate treatment.
Treatment of exostoses
When diagnosing exostosis, treatment is prescribed only when symptoms appear. Otherwise, dynamic monitoring of the tumor is sufficient. If the tumor bothers the patient, depending on its type, the nature of the manifestation of osteochondroma, conservative treatment is selected or surgical intervention is prescribed. But the main method of treating exostosis is surgery.
Conservative, i.e., non-surgical, therapy is indicated mainly for exostosis of the calcaneus and rib, but only in the early stages of development. First of all, the use of special orthopedic insoles, made individually, and the replacement of regular shoes with models with offset edges are prescribed. This helps eliminate mechanical pressure on the tumor, reducing the load on the Achilles tendon and calcaneal tubercle.
If severe pain and inflammation occur, drug therapy is prescribed, including:
- NSAIDs in the form of topical agents (Nimid, Dolaren, Ketoprofen, Voltaren);
- drug blockades with the introduction of a mixture of anesthetics and corticosteroids (performed for severe pain that cannot be eliminated by other means).
Courses of physiotherapeutic procedures are also indicated. Shock wave therapy (SWT) is the most effective. It involves the impact of infrasonic acoustic waves on the affected area. The mechanism of action of the method is based on the cavitation effect that occurs at the interface between media. The acoustic resistance of soft tissue is less than that of bone. Therefore, sound waves penetrate through them and affect bones and cartilage. This provokes an improvement in blood supply, restoration of normal cartilage tissue and bones, and a reduction in the size of tumors.
Additionally, we may recommend:
- electrophoresis with the introduction of anesthetics;
- ultrasound therapy;
- laser therapy;
- Ural Federal District;
- magnetotherapy.
How to remove epulis from gums
The only option to completely get rid of an unpleasant tumor is to remove it surgically. In mild cases, this is performed by a dentist under local anesthesia. If bone is involved or there is a risk of malignant cells being detected, this major operation should be performed by an oral and maxillofacial surgeon. In the case of the giant cell form, all tissues that came into contact with the neoplasm are additionally removed.
You should not start epulis, the treatment of which at the very initial stage can be carried out quickly and easily for a person. The dentist will gently remove the small bump using a laser or liquid nitrogen. Such interventions are very gentle and practically do not damage the surrounding mucosa. After them, the gums quickly recover and heal. To speed up the process, apply compresses with Solcoseryl or Levomekol ointment to the wound. The latter contains a small amount of antibiotic, so it protects the sutures from infection.
During the entire rehabilitation period, the patient is recommended to treat the operated areas with hydrogen peroxide, and then rinse his mouth with antiseptics such as Chlorhexidine, Miramistin or Chlorophyllipt. In severe situations with suppuration, a course of antibiotics cannot be avoided:
- Biseptol;
- Amoxicillin;
- Azithromycin.
Unfortunately, epulis on the gums may appear again after some time. As a preventive measure, dentists recommend avoiding any injuries and protecting the mucous membrane from hypothermia and burns. It is imperative to visit a specialist every 6-8 months in order to notice the formation of a lump in time and remove it without consequences.
When a lump appears on the gum, most people mistake it for an abscess. However, such formations are not always infectious in nature. One of the types of gum tumors is the so-called epulis, which is usually painless and identical in color to the gum tissue.
Surgery to remove exostosis
Surgical intervention is indicated for:
- large size of osteochondroma and the presence of persistent pain;
- development of complications (tendinitis, bursitis, vascular, neurological disorders, etc.);
- bone deformations as a result of the growth of exostosis;
- fracture of the base leg;
- malignancy of the tumor.
For children with bone exostosis, surgery is prescribed only in extreme cases. As a rule, it is carried out only if the testimony remains after reaching adulthood.
But if there are contraindications, surgery is not performed. This:
- purulent-inflammatory processes in the area of the upcoming intervention;
- exacerbation of chronic diseases;
- decompensated form of diabetes mellitus;
- acute infectious diseases.
Treatment of exostosis with surgery involves its complete excision with capture of the cartilaginous cap. There are several methods for removing osteochondral growth. A specific one is selected based on the location of the osteochondroma and its size. Usually preference is given to marginal resection of the growth, i.e., its removal within healthy tissue. Only in some cases is it necessary to resort to corrective osteotomy with concomitant resection of osteochondroma, but the cost of removing exostosis in this way is higher, since the operation also corrects bone deformation.
After surgery, complete recovery is observed in 98% of cases. Therefore, almost everyone who has once removed an exostosis forgets about it forever.
Marginal resection is a relatively simple type of surgery. Its essence is to expose the affected bone and remove the entire neoplasm in the front of healthy tissue along with the surrounding capsule using a sharp chisel, drill, oscillating saw or bur. After removal of the pathological formation, curettage of the maternal bone is performed using cutters and bur. In some cases, the extent of resection can be large and create the need for bone grafting using autografts or special implants. It is important to remove the entire cartilaginous cap and neoplasm, otherwise a relapse may develop.
Carrying out a corrective osteotomy involves cutting the mother's bone using an osteotome and removing the osteochondroma. After this, the bone fragments are fixed in the desired position using special plates, screws or knitting needles.
Where to get treatment in Moscow, clinics, prices?
To remove epulis, you must contact dental clinics that have surgeons on staff. Average cost of the procedure (in rubles) in some Moscow clinics:
- Center for Aesthetic Dentistry – 6000.
- Denta-El – 5000.
- Dantistoff – 7500.
- Inpromed – 5500.
- Capital – 7600.
After surgery, it is very important to follow the doctor’s recommendations regarding wound care, treatment and oral hygiene, and diet. This will prevent the development of complications and relapses.
It is also important not to forget that the primary prevention of the appearance of tumors is timely dental examinations, hygiene, removal of tartar, adjustment of dentures, braces and fillings.
Jump to: navigation, search
EPULIS
(
epulis
; Greek epi- on + ulon gum; synonym
epulid
) - tumor-like connective tissue growths on the alveolar processes of the jaws.
In origin
epulis, local damaging factors are of great importance, in particular injury to the mucous membrane from the sharp edges of destroyed teeth, fillings hanging on the gums, incorrectly made crowns or dentures. In women, the development of epulis is often associated with hormonal disorders that occur during pregnancy. Epulis can also form during teething.
There are fibrous (granulomatous), angiomatous and giant cell epulis. A distinctive feature of fibrous and angiomatous epulis is its connection with the teeth. Giant cell epulis can also develop on edentulous jaws.
Epulis occurs in women 3-4 times more often than in men. Fibrous and angiomatous epulis occurs mainly at young and mature ages (from 20 to 50 years), giant cell - at any age.
Fibrous epulis
macroscopically it is a mushroom-shaped formation of small size, round or oval, sometimes irregular in shape, located in the gum area, often on its vestibular surface, on a wide or narrow base (pedicle). Fibrous epulis has a dense, elastic consistency, is painless on palpation, and does not bleed. Its surface is smooth or lumpy, covered with a pale pink mucous membrane, the color of which, as a rule, does not differ from the color of the surrounding mucous membrane. Microscopically, growths of mature fibrous connective tissue are detected, among the bundles of which islands of bone substance, surrounded by osteoblasts, are sometimes detected (tsvetn. fig. 8a, 86). Granulomatous epulis is usually called ulcerated fibrous epulis with abundant proliferation of granulation tissue in the area of ulceration.
Angiomatous epulis
- a formation of round shape, soft-elastic consistency, localized mainly in the area of the alveolar process at the level of premolars and molars. The surface is fine-grained, covered with a mucous membrane of a bright crimson color, often with a cyanotic tint; upon palpation, bleeding easily occurs, which is sometimes pulsating. Angiomatous epulis grows quite rapidly, especially during pregnancy. Microscopically, its tissue is formed by numerous thin-walled blood vessels with lumens of various sizes and shapes, which resembles the picture of an angioma (tsvetn. fig. 9a, 96).
Giant cell epulis
- a formation of round or oval shape, soft or densely elastic consistency, covered with a dark red or brownish-blue mucous membrane. On microscopic examination, in the connective tissue rich in thin-walled vessels, multinucleated giant cells of the osteoclast type (tsvetn. 10a, 106) and mononuclear cells of the osteoblast type are found. Among these cellular elements, accumulations of erythrocytes and hemosiderin deposits lie freely; There are serous and blood cysts, islands of osteoid and bone tissue. According to the WHO classification, giant cell epulis is divided into peripheral giant cell granuloma (originating from the soft tissue of the gums) and central, or reparative, giant cell granuloma (developing in the bone of the alveolar process).
Giant cell epulis grows slowly, but can have progressive growth and reach significant sizes. In such cases, its surface is often injured by antagonist teeth with the formation of erosions and bedsores. With a significant increase in the size of the epulsa, teeth often become loose.
X-ray examination of fibrous and angiomatous epulis does not always reveal bone changes; Often only a shadow of a soft tissue tumor is visible, sometimes with areas of calcification of various sizes. With prolonged growth of fibrous epulis, an x-ray of the jaw may reveal marginal lesions with clear contours at the site of contact of the epulis with the bone. With angiomatous epulis, in some cases a picture of bone hemangioma is observed (see). Giant cell epulis is characterized by vaguely defined bone destruction (central giant cell granuloma).
Treatment
surgical, consists of excision of the epulis within healthy tissues along with the base (pedicle). After excision of fibrous and angiomatous epulis, in case of bone damage, it is necessary to completely remove its softened area - scrape it out with a sharp spoon or using a bur or cutter. The cessation of bleeding from the wound is a sign of complete removal of the epulis. The operation is completed by electrocoagulation of the wound surface and fixation of a tampon soaked in iodoform on it. Teeth in the epulis area are removed if they are mobile or their roots are excessively exposed, as well as if bone destruction is detected by x-ray. Teeth should also be removed if epulis recurs. When excising giant cell epulis, a partial resection of the alveolar process is performed within healthy tissues along with the teeth. The wound is treated with 96% alcohol, and it heals by secondary intention (under a tampon). In some cases, it is possible to close the wound with a mobilized mucoperiosteal flap.
Forecast
With timely and radical treatment, epulis is favorable.
In the prevention of epulis, the main role is played by the prevention and elimination of gum injuries. It is especially important to monitor the condition of gums in pregnant women.
Bibliography:
Abrikosov A.I. On the pathological anatomy of widespread fibrous osteitis, Rus. Klin., vol. 5, no. 23, p. 343, 1926; Vasiliev G. A. Dental surgery with a course of maxillofacial traumatology, p. 296, M., 1973; Evdokimov A.I. and Vasiliev G.A., Surgical dentistry, p. 242, M., 1964,
T. G. Robustova (author of the article and color drawing).
Category: Source: Great Medical Encyclopedia (BME), edited by Petrovsky B.V., 3rd edition
Recommended Articles
- Article reading time:
1 minute
Seals, or bumps on the gums, form in patients of different age categories. They can lead to various dangerous diseases, and therefore require clarification of the root cause of their occurrence and selection of effective treatment.
Rehabilitation
After removal of the exostosis, the patient remains in the hospital for 3 days, the sutures are removed on days 7-10. Performing marginal resection does not require any serious restrictions even in the early postoperative period. The patient can completely return to his usual lifestyle after the stitches are removed, and forget about exostosis immediately after the operation.
When performing a corrective osteotomy, complete bone fusion occurs after 6 weeks, but full recovery may require up to 3 months. At this time, it is important to strictly follow all the doctor’s recommendations and not to overload the operated part of the body. All patients who have undergone osteotomy are prescribed drug therapy, exercise therapy, and often physical therapy. The duration of rehabilitation in such cases depends on the type of surgical intervention performed and the individual characteristics of the patient.
Thus, osteochondroma is a very common type of tumor. At the same time, statistics on the frequency of its occurrence are not entirely objective, since exostoses often do not appear throughout a person’s life, and therefore are not diagnosed. However, if the formed formation bothers the patient, causes him pain, or reduces the quality of life, you should not hesitate to contact an orthopedist. A specialist will be able to assess the degree of danger of the tumor and, if necessary, remove it using the most gentle method possible.
Diagnosis and treatment of gum formations
A gingival lump can be easily identified during a visual examination and instrumental examination. To clarify the diagnosis, an x-ray or biopsy may be indicated.
Treatment methods are determined by the root cause of the formation on the gums. First of all, you will need to limit the further development of the infection and eliminate pain.
Traditional treatment is as follows:
- fistula
– elimination of pus by rinsing (using Chlorhexidine, Miramistin, decoctions of medicinal herbs, saline solution);
- epulis
– surgical treatment (removal with a scalpel, cryodestruction or diathermocoagulation);
- periodontitis
– unsealing and cleaning of root canals, removal of accumulated pus, mouth baths made of soda solution or herbal decoctions;
- periostitis
– opening the tooth and placing special medications under a temporary filling (if there is no positive result, the diseased tooth must be removed);
- gingivitis
– cleaning of periodontal pockets, antibacterial and antiseptic treatment, removal of pathological formations.
Traditional medicine offers treatment with freshly squeezed juice of Kalanchoe leaves, used in the form of lotions. Another option is to chew the leaves, having previously cleared them of the film. A popular remedy for bumps in the mouth is rinsing with regular vodka.