Implantation with immediate loading is an innovative method of dental restoration that allows you to install any number of teeth in the shortest possible time in the most gentle way. The minimal invasiveness of the procedure reduces not only the duration of the rehabilitation period, but also the number of contraindications to surgery.
Immediate Load implantation is also called one-stage or express implantation. Considering the peculiarities of implant installation, it is also called basal implantation.
For the first time in Russia, basal implantation was used in a metropolitan clinic, where to this day it is a popular method of dental restoration.
Only the ROOTT center has an exclusive franchise for the use of the ROOTT immediate load implantation method in Russia.
Contents of the basal dental implantation section:
- Benefits of the basal method
- Installation video
- Engraftment of implants
- Advantages
- Photos before and after treatment
- Features of the method
- Stages of implant healing
- The history of the implantation method
New teeth in 3 days - all inclusive! And you can chew!
Implantation with immediate loading of a prosthesis - 44,000 rubles. for a unit.
Installation of a complete metal-ceramic bridge prosthesis on one-stage implants of the ROOTT system (1 jaw) - RUB 210,000. 250,000 rub.
Only our center has an exclusive franchise for the use of the ROOTT immediate load implantation method in Russia.
How much does implantation cost in 1 day?
The cost of implantation using the immediate loading method is lower than the cost of two-stage treatment. This was made possible by reducing visits to the doctor and eliminating the need for bone grafting. Promotions and discounts that are regularly held at the Ilatan clinic allow you to insert teeth in one day “turnkey” on favorable terms. The cost is fixed in the contract and does not change during treatment. The turnkey price includes all necessary procedures and manipulations, from implant installation to follow-up examinations. You can ask your doctor any questions you have during a consultation or online by filling out the form on the website.
Advantages of the basal implantation method
The unique feature of the method is determined by the method of implanting implants into the deep basal layers. These tissues are practically not subject to atrophic processes, unlike the alveolar spongy layer. As a result, it is possible to install implants using the basal method even in complex clinical cases, when alveolar tissues are atrophied, in patients with periodontal disease and other serious diseases.
Installation is carried out using the compression method through a puncture. This is a much less traumatic method compared to the need to saw through the bone for a plate implant or remove a flap of gum for a two-phase implantation.
Basal implantation is performed using monoblock systems, that is, the rod and abutment form a single whole. This made instant loading possible: immediately after implantation, a light bridge-like prosthesis is fixed on the top of the implant and included in the chewing process.
Being correct load conductors, such implants transfer normal pressure when chewing food to the bone layers of the jaw. This stimulates metabolic processes in them and activates osseointegration.
Due to the fact that the implant and abutment are a one-piece structure, FIXED dentures can be installed immediately. A person can forget about missing teeth or removable dentures, returning to a normal lifestyle within 3-4 days. Implants, being conductors, evenly and correctly distribute pressure on the bone and among themselves, while stabilizing each other. The implant healing process is based on stimulating the natural processes of bone tissue restoration during the process of chewing food.
Prosthetics using the All-on-4 method
The prosthesis installed on the day of surgery has a service life of 1 year. Then it can be replaced with metal-ceramic or zirconium without affecting the implants. The zirconium prosthesis has no limitations on service life, does not cause allergic reactions and is manufactured using the precise CAD/CAM method (modeling and manufacturing of the prosthesis occurs using computer technology and high-precision milling).
Screw fixation is very popular, when the prosthesis is screwed without the use of cement. This ensures that nothing extra remains under the prosthesis (there will be no excess cement, since there is no cement at all), and the prosthesis can be easily unscrewed by the dentist without damaging the implants and the prosthesis itself.
A properly manufactured screw-retained prosthesis should not be screwed directly to the implants, but to multi-unit abutments, which, in turn, are screwed to the implants. This is the most critical place for the long-term functioning of the implant and prosthetic structure. If the prosthesis is made from the level of implants without abutments, then we are not talking about factory accuracy. In this case, complications arise such as loosening or fracture of screws, inaccurate fit of the prosthesis to the implants, which leads to infection of the junction of the implant and the prosthesis, inflammation and loss of bone tissue, up to the loss of the implant.
Expert opinion
Igor Yurievich Malinovsky
Maxillofacial surgeon, implantologist
Experience: more than 11 years
Implantation with immediate loading combines a number of modern protocols, the essence of which is the almost instantaneous restoration of aesthetic and chewing functions of the dentition, mainly with multiple restorations. When implanting implants, not only cancellous bone tissue is used, but also deeper layers, both of the jawbone and of the skull. Due to this approach, basal dental implantation is carried out without additional osteoplastic interventions.
Secrets of technology success
Rapid implantation is gradually replacing classical implantation. The success of the technology is explained by a number of advantages presented by:
- versatility. Implantation is applicable in almost all clinical cases; low morbidity. The operation is performed without incisions in the gums and does not require bone tissue augmentation;
- speed. In just 3-5 days you will be able to enjoy your renewed smile without worrying that the artificial teeth will fall out at any moment;
- complete restoration of chewing functions. Immediately after installing the prosthesis, you will be able to enjoy your favorite food, but you still need to increase the load gradually;
- accompanying lift. Without expensive, dangerous plastic surgery, you can get rid of wrinkles and tighten your facial contours;
- durability. A reliable implant installed by an experienced dentist serves its owner for a lifetime;
- efficiency. Installing a separate implant to replace each extracted tooth is an expensive and time-consuming procedure. Modern methods offer comprehensive restoration of the dentition in a minimum of steps without the need for bone augmentation, which allows you to get rid of unnecessary expenses.
Despite the growing popularity of rapid implantation, many patients are worried that it is impossible to carry out high-quality dental restoration in three days. Doctors claim that such rumors are nothing more than a myth, but admit that the procedure has its drawbacks.
FEATURES OF IMPLANTS FOR IMMEDIATE LOADING
HOW IMPLANTS WORK WITH BONE TISSUE
- The cortical plate is a narrow protective shell layer, 95% consists of mineral salts, and accordingly is hard and practically does not dissolve;
- The alveolar region (spongy) is a softer layer of bone, 70% consists of bone septa and crossbars, between which capillaries pass. This section is most susceptible to inflammatory processes and bone resorption in the absence of chewing load;
- The basal section is a deep layer of bone, which is denser and stronger than the previous two and is least susceptible to atrophy. It is this department that is used by specially created implants for cases of severe bone tissue deficiency. Thanks to a special thread, according to indications, the rods are attached, including in the cortical plate, which gives them greater stabilization and uniform load distribution based on the principle of support at 5 points.
Before performing basal implantation, the doctor individually models the structure so that the distribution of pressure during chewing is uniform. In combination with basal implants, compression ones are used, which work with the alveolar region and can be installed at different angles to give the entire structure stability sufficient to withstand immediate chewing load. When such implants are implanted, the alveolar region is subject to compaction (condensation), forming a dense (cortical) layer around the implant. This layer does not dissolve for a long time and serves as the foundation of the product until the new bone absorbs it. The final stabilizer of the structure is the fixation of the prostheses 3-4 days after installation of the implants. This technology allows you to restore the roots of teeth even in complex cases of bone tissue atrophy.
Do not forget that the bone structure of each patient is individual; there are cases of atrophy when the implantation of any implants is not indicated without additional manipulations to build it up (the bone can be atrophied even up to 1-2 millimeters in height or width). Such cases are extremely rare, however, even after bone grafting, the overall period of dental restoration can be significantly reduced, since prosthetics on basal implants is performed after implantation, and not after several months, as with the classic protocol with delayed loading.
What is delayed implantology?
Lazy loading is a two-step method. At the first stage, a titanium implant is inserted and a cap is placed on it. Then the gum is sutured, and at the second stage a post is installed on which the crown is attached. The period between phases, also called the osseointegration period, is 3-4 months for the jaw and 5-6 months for the maxilla. Even in the case of delayed implantology, the patient may have a temporary bridge, but it will be a temporary mobile or fixed bridge that is supported by natural teeth rather than implants.
BY CHEWING YOUR FOOD YOU HELP THE IMPLANTS TAKE PLACE
Instant chewing load is one of the key points of the technology, since implants act as conductors of chewing load, capillaries in bone tissue are activated, cells begin to receive proper nutrition and self-heal. Thus, in addition to restoring aesthetics and returning to normal food intake, patients also help the process of osseointegration (engraftment of implants in the body). In patients with severe facial asymmetry due to missing teeth, the bite is gradually restored, the facial muscles begin to work as before, and premature signs of aging disappear. Diction is restored, digestion and the general condition of the body as a whole are improved. The fact is that due to the absence of teeth, patients begin to avoid hard foods; as a result, less nutrients enter the body and metabolism is disrupted.
Limitations for one-stage implantation
Absolute contraindications, in the presence of which one-stage dental implantation in Moscow becomes impossible, include:
- Weakening of the immune system;
- Diseases associated with changes in bone structure (porosity and loosening of bone tissue);
- The presence of inflammatory processes in the mucous and gingival tissues;
- The presence of cysts and granulomas in the jaw area;
- Disruption of the circulatory system;
- Psychical deviations;
- If it is impossible to tightly fix the implant, in the presence of a massive hole formed after tooth extraction;
- Oncological processes in the body;
- Diseases of periodontal tissues;
- Hypersensitivity to anesthetics;
- Endocrine diseases caused by increased blood sugar;
- Presence of sexually transmitted diseases;
- Tuberculosis in an advanced stage;
- Decrease in bone tissue;
- Excessive tension in the masticatory muscles;
- Diseases of autoimmune etiology.
Among the restrictions that are relative in nature, the following points are highlighted:
- The presence of rotten or caries-affected teeth in the oral cavity;
- Failure to comply with hygienic care rules;
- The period of bearing a child;
- Inflammatory processes in the area of gingival tissue;
- Excessive alcohol dependence, drug use and tobacco product abuse;
- Inflammation of tooth roots;
- Joint diseases;
- Vertical anomaly of occlusion.
Also, one-stage dental implantation in Moscow is not recommended if the following general factors are present:
- Use of medications that have a negative effect on blood clotting;
- Use of sedatives and antidepressants;
- Prolonged depression and stress in the patient;
- Exhaustion of the body;
- General somatic diseases in the acute stage;
- Presence of restrictions for fixation of local implantation systems;
- Alcohol abuse;
- Neglect of oral care rules.
Temporary reasons for this technique include:
- Presence of acute diseases;
- Pregnancy period;
- Drug use;
- Rehabilitation after radiation exposure;
- The period of recovery after any illness.
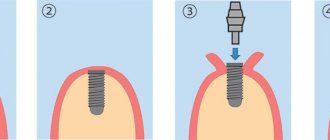
IMPLANTATION STAGES WITH IMMEDIATE LOADING
- preparing the patient and oral cavity for surgery;
- modeling of an individual design of implants to suit the specifics of the patient’s case.
- If there are movable teeth that cannot be restored, they are removed and implants are immediately installed in their place.
- If teeth are already missing, then the bed is formed using a puncture method, and then the implants are implanted into the bone using the compression method;
- The orthopedic doctor makes an impression, models and manufactures the prosthesis;
- the tops of the implants (abutments) are fixed at the required angle for subsequent installation of the prosthesis;
- on the third day after implantation, a permanent metal-plastic prosthesis is installed on the structure, which is adjusted to the patient’s bite;
- the patient can begin to use the new teeth.
VIDEO REVIEWS OF PATIENTS - WATCH HOW THE OPERATIONS GO
Tips on how to choose a clinic and doctor for treatment?
- Make sure that the clinic actually carries out the procedures that it claims, if there are any necessary licenses, certificates, or permits.
- Carefully familiarize yourself with what implantation systems the clinic operates. It is necessary to install implants and superstructures of the same brand. The doctor opens the package only in front of the patient.
- The doctor must have sufficient experience in performing such operations; if the implantologist has performed 2-3 interventions, it is better not to take risks.
- Find out whether the clinic provides a guarantee for the doctor’s work and other services. Warranty obligations must be stated in the contract.
- Analyze customer reviews, list of services, view equipment, examples of work. Compare the cost of services.
DIFFERENCES AND ADVANTAGES OF DENTAL IMPLANTATION WITH IMMEDIATE LOAD
| DIFFERENCES | ADVANTAGES |
|
|
New teeth in 3 days - all inclusive! And you can chew!
Implantation with immediate loading of a prosthesis - 44,000 rubles. for a unit.
Installation of a complete metal-ceramic bridge prosthesis on one-stage implants of the ROOTT system (1 jaw) - RUB 210,000. 250,000 rub.
Only our center has an exclusive franchise for the use of the ROOTT immediate load implantation method in Russia.
Implants for immediate loading
Installation of an implant on the ROOTT system in Russia is carried out only in ROOTT centers. We are official partners of TRATE AG in Russia, installing only high-quality and time-tested implants developed on the basis of research by the European Open Society of Dentistry, with the participation of domestic colleagues from the Russian Association of Implantologists.
The size, shape and method of installing the rods are selected strictly individually according to medical indications. Basal surgery can take place in a one-step format immediately after tooth extraction in 1 appointment.
Read more in the article why the ROOTT implant system. Read more in the article why the ROOTT implant system .
The path of surgical dentistry to the development and full use of the method of direct implantation with immediate loading was one of the most difficult and lengthy in modern medicine. The study of the clinical and morphological features of the method, along with the development of new bone materials and implants, took decades.
One of the main reasons why the concept of immediate implantation justifies itself is the combination of the period of osseointegration with the healing of the tooth socket, stimulation of osseointegration, minimization of bone resorption and bone atrophy.
Theoretical foundations and
historical background
Branemark's discovery of the process of osseointegration, which occurred while studying the microstructure of the bone marrow, was the impetus for the introduction of dental implants into dentistry. The clinical application of this significant discovery was preceded by ten years of in vivo experimental studies to establish the degree of osseointegration of the implants and confirm the presence of direct bone-implant contact. The results obtained confirmed the absence of negative reactions from soft and hard tissues to the implants, which subsequently made it possible to begin clinical studies of dental implantation in humans.
As a result of the studies, the conditions necessary to ensure high-quality osseointegration of dental implants were determined. These include:
- Use of biocompatible materials.
- Compliance with the Bronemark protocol, which assumes a time period from implantation to loading on average of 3 to 6 months, as well as implantation into bone tissue that is completely healed after tooth extraction.
- Low tool rotation speed 900-1500 rpm when drilling bone.
- Using a buccal incision away from the alveolar ridge.
- Carrying out the procedure in a sterile hospital environment.
- Use only titanium tools and materials.
- No infectious process.
The variety of clinical situations and the need to accelerate the orthopedic rehabilitation of patients required a revision of the generally accepted Bronemark protocol, which was solved through the development of innovative methods of implantation, augmentation, the development of new models of implants, new osteoplastic materials and medical instruments, and the improvement of clinical diagnostics.
Currently, the two-stage Bronemark protocol remains frequently used, but the recommended atraumatic drilling to eliminate overheating of the bone tissue does not exclude osteonecrosis. The combination of mechanical damage and excess heat forms a devitalized zone of bone tissue up to 1 mm in size. It is known that heating the tissue near the drill to 38-41°C is sufficient for its death.
Due to the need for bone drilling, which will certainly lead to necrosis of the peri-implant area, it was advisable to propose minimizing the additional stress factor due to loading. This predetermines the holding period from the moment of installation of the dental implant to the load required for high-quality osseointegration, which does not reduce the relevance of the two-stage protocol today.
The use of modern tools and an individual treatment protocol in each individual case allows us to avoid and reduce the degree of undesirable results in the form of osteonecrosis. Prevention of osteonecrosis and fibrous encapsulation is achieved by modifying factors that lead to the formation of heat in bone tissue and are associated with the volume of preparation, the sharpness of drills, the depth of the osteotomy channel, etc.
It has now been proven that the phenomena of bone tissue necrosis can be minimized using the technique of preparing the osteotomy canal with a drill rotation speed of up to 1500 rpm and a drill cooling system. As a result of numerous improvements, the necessary primary stability of the implant was achieved within the limits of permissible micromotion, which led to the emergence and development of an innovative method of one-stage implantation.
Direct implantation with immediate loading has become possible in optimal clinical conditions, as well as with the appropriate size and design of the implant surface, the presence and sufficient volume of the required bone tissue biotype, the absence of additional stress factors and the infectious process. X-ray research methods are traditionally used to determine the clinical conditions for direct implantation.
First stage of the procedure: visualization of bone tissue
At the first stage of diagnostic imaging, as a rule, panoramic radiography is used, which allows one to obtain an image of the upper and lower jaw, the lower half of the maxillary sinuses. PR is far from the best diagnostic method in the context of obtaining detailed information, but it has a number of advantages.
The advantages of panoramic radiography include the ease of assessing the initial vertical height of the bone and macroanatomy of the jaws with the determination of existing major pathology, as well as the low cost and accessibility of the procedure for the patient. The disadvantages of PR are the lack of a detailed three-dimensional image of bone structures, as well as the inability to assess the quality of bone tissue and the degree of its mineralization.
Zoning using diagnostic templates is also not informative enough. Loss or repair of bone tissue from the vestibulo-oral side of the roots of teeth or an installed implant is not determined radiologically, since only the distal and medial areas are visible on X-ray films.
With the advent of computed tomography (CT), virtually all of the shortcomings associated with two-dimensional imaging of the PR have been eliminated. CT today represents a powerful digital method for obtaining three-dimensional images, allowing highly accurate diagnosis of the condition of tissues of different densities without the introduction of contrast agents. The technique reduces the risk of ongoing complications and relieves patients from psycho-emotional stress.
The use of an electronic version of three-dimensional images makes it possible to process data from one anatomical area on all CT sections with precise measurement of parameters and determination of the relationship between adjacent anatomical areas.
The role of the design, size and material of the dental implant
The possibility of effective direct implantation achieving osseointegration of titanium implants has been proven by histological studies in animals, as well as in humans. It was found that particularly careful consideration of implant size and design is required for the use of MNIN.
In the case of the two-stage Bronemark protocol, the length of the implant cannot solve the problems of reducing the load in the bone-implant zone, since the main load is concentrated in the edges of the alveolar process, namely its cortical layer. During direct implantation, the directed load affects the formation of the histological contact zone, so the length of the implant is important.
The resistance of implants is determined by different researchers relative to the average values of the plane of the roots of the teeth bearing the chewing load. Replacement of a tooth with an implant occurs according to the equivalent plane of intraosseous support. With MNINN and two-stage implantation, the width, length and design of the implant are important for the formation of bone-implant contact, since the main part of the stress from the mechanical load is concentrated at the edge of the bone
The length of the implant is important because it increases primary stability. This should also be facilitated by rational implant design. Remodeling and osseointegration do not occur simultaneously, so with a decrease in primary stability and simultaneous loading, there is a risk of exceeding the acceptable micromotion threshold, which will lead to implant loss.
Maintaining the micromotion threshold depends on bone type, implant surface treatment, and biomechanical load. The micromobility threshold, regardless of the surface coating of the product (for example, titanium implants with plasma spraying or bioactive implants) ranges from 50 to 150 μm.
For the direct implantation method with immediate loading, a screw implant with a maximum functional area is used, which is provided by the geometry, number and depth of the thread. The smaller the distance between the threads, the greater their number and the larger the surface area of the implant.
The thread depth also differs between designs. The greater the depth of the thread and the number of turns, the larger the supporting area of the implant. The use of implants of other shapes is ineffective for MNINN. It has been experimentally proven that there is no bone integration on the day of installation of a cylindrical implant with a tight fit, since there is no bone tissue between the threads.
The functional surface influences the rate of bone remodeling under occlusal loading. The geometry of the thread with a V-shaped and thrust profile determines the rate of early osseointegration of the bone-implant contact zone due to resistance to occlusal load forces, which reduces microstress in the bone tissue.
The condition of the implant surface ensures not only proper contact with bone tissue, but also a direct influence on the rate of osseointegration and the formation of distance or contact osteogenesis. The micro- and macrostructures of implant surfaces with different chemical structures have different effects on the stages of osseointegration.
Implant surface: rational choice
The use of a dental implant with a hydrophilic surface increases the adsorption of biological fluids with the subsequent attachment of blood plasma proteins at the stage of hemostasis, which accelerates osseointegration in the early stages. The presence of roughness or depressions of a certain size on the intraosseous part of the dental implant promotes the adsorption of proteins, mechanical retention of fibrin and collagen fibers, adhesion of osteogenic cells, and the synthesis of specific proteins and growth factors.
The relief allows you to significantly increase the specific area of the implant that interacts with the bone, which improves the quality of integration and reduces the level of mechanical stress of the surrounding bone tissue. The quality of the surface and its roughness is determined by the methods of processing the surfaces of the implants.
Below are the main types of surfaces used in the manufacture of dental implants for the direct implantation procedure with immediate loading.
SLA (andblasted with large grits and acid etched) is a surface that, as the abbreviation implies, is formed by coarse sandblasting followed by acid etching. Due to this type of processing, microdepressions measuring 2-4 microns in size appear on the surface of the product in the form of inclusions in the rough sandblasted surface.
Cell culture experiments, histological studies of bone, and animal experiments with implant removal indicate that SLA is a good choice for implant contact surfaces. In vivo studies have confirmed the superiority of SLA surfaces in implant integration and anchorage compared to other surfaces such as titanium plasma sprayed, machined or hydroxyapatite coated surfaces, especially during the initial healing phase after implant placement.
The most important property of the SLA surface, which plays a significant role in the development and practical use of implants, is the provision of a high load on it, which was confirmed experimentally in torsion experiments.
RBM (Resorbable Blast Media) is an implant surface created by sandblasting with beta-tricalcium phosphate particles of a certain density, mass and size. After mechanical processing, this surface is etched with a low-concentration organic acid, which makes the surface clean (without Ca3O8P2 residues), without modifying the structure of the titanium micropattern.
This method makes it possible to create micropores of greater depth on the surface of the implant than when treated with the traditional SLA method (aluminum oxide Al2O3). In this case, the surface area of the implant further increases due to an increase in the depth of the pores (craters), and its osteoconductivity increases accordingly.
Increasing the efficiency of osseointegration of implants with a bioactive coating also depends on the implantation technique and the patient’s bone tissue biotype.
Osseointegration of implants coated with hydroxyapatite occurs according to the principle of both contact and distant osteogenesis in certain peri-implant areas. With contact osteogenesis, new bone formation occurs directly on the surface of the implant itself.
The implementation of this mechanism occurs by analogy with osteoconduction. Hydroxyapatite on the surface of the implant acts as a passive matrix for osteogenesis. In this case, migration of progenitor cells occurs on the surface of the implant, which begin to differentiate into mature osteoblasts and secrete bone matrix on the surface of the implant under conditions of delayed loading.
Hydroxyapatite significantly reduces the rate of bone tissue remodeling under conditions of occlusal load, which has a positive effect on implantation results when applying immediate load in bone tissue biotype D4. In such situations, hydroxyapatite coating reduces the risk of overloading.
A comparative clinical and morphological assessment of implants with and without a bioactive coating one month after installation does not reveal any difference in the processes of osteogenesis.
Bone density as a factor in the success of dental implantation
Bone density is the most important factor for the success of dental implantation. According to the generally accepted international classification of bone tissue, there are four quality categories:
- D1 consists of homogeneous compact bone tissue.
- D2 bone consists of a thick cortex surrounding dense trabecular bone tissue.
- D3 bone consists of a thin cortex surrounding dense trabecular bone tissue.
- D4 consists of a thin cortex surrounding low-density trabecular bone tissue.
The likelihood of an implant not having micromobility and meeting the minimum required micromobility threshold directly depends on the bone tissue biotype. The lower the bone density, the lower the elasticity. The rate of remodeling of cortical bone tissue is much slower than trabecular bone tissue. In addition, differences in the preservation of lamellar structure are observed.
For one-stage implantation and MNINN, the ideal option is the presence of bone tissue of D1 biotype. A thick layer of homogeneous compact bone tissue is more often found in the anterior regions with a completely edentulous mandible. As the height of the alveolar ridge changes with a decrease in the volume of bone tissue, D1 is more often observed in the corresponding posterior parts of the mandible.
There is practically no implant mismatch for this biotype. The compressive strength of bone D1 is up to 22.5 MPa. In the practice of direct implantation with immediate loading, bone tissue with the full biotype D1 is not found, which is due to the environment of compacted, but trabecular bone tissue.
The preferred option for immediate loading is bone with biotype D2, let's say biotype D3 with a compressive strength of 7.5 MPa. Implant mismatch in biotype D2, namely the presence of cortical bone tissue of different densities and coarse trabecular tissue, is not predicted.
Clinical discrepancy is expected in bone biotype D4, in which there is thin cortical bone surrounding low-density trabecular tissue, and in some variants of biotype D3, in which thin cortical bone surrounds acceptable-density trabecular bone and has insufficient volume.
Taking into account the classification of bone tissue biotype and the corresponding localization by jaw sections when using INNNN can lead to a significant reduction in the risks of a negative result from a labor-intensive and expensive procedure.
Optimizing the load on dental implants
Currently, several approaches are proposed to reduce the occlusal stress factor of the load for direct implantation with immediate loading. In case of multiple missing teeth, a slightly larger number of implants are installed.
Some are loaded with a transitional prosthesis, others remain embedded in the jaws without loading during the normal bone healing period. After the period required for osseointegration, the preserved implants, loaded during the specified period, are also included in the orthopedic design.
Another protocol involves immersion of all installed implants from the very beginning, with the possible placement of additional structures in the bone-implant contact areas to reduce stress. Immediate loading with partial absence of teeth, including the loss of single teeth, was carried out taking into account the possibilities of their unloading, which was achieved by removing the orthopedic structure from occlusal contact.
The necessary conditions for successful dental implantation, related to a sufficient amount of surrounding bone tissue and the shape of the implant, are listed below:
- All alveolar walls must be preserved and have a thickness of at least 2 mm.
- Below the bottom of the socket of the extracted tooth there must be at least 3-4 mm of bone tissue to ensure reliable primary fixation of the implant.
- The implant must match the length and diameter of the socket as accurately as possible.
These conditions were partially achieved using additional modern techniques, instruments for traumatic tooth extraction and implant installation, and the use of osteoplastic materials. Atraumatic tooth extraction with one-stage implantation is of great importance for the success of osseointegration.
The discrepancy between the shape of the tooth socket and the shape of the implant, the loss of one or more walls of the socket negatively affects the result of the procedure. It is necessary to have three or four alveolar walls for successful implantation. Achieving primary implant stability in the absence of two or more alveolar walls is unlikely, even despite the seemingly sufficient bone reserve.
The availability of modern instruments and the emergence of new methods of tooth extraction using ultrasound makes it possible to successfully carry out atraumatic removal. In the past, the presence of inflammation in the tissues surrounding the tooth socket and the alveolar bone adjacent to the implant bed was considered an absolute contraindication to the procedure. Thanks to the experience of successful osseointegration of implants when installed in an infected tooth socket under the cover of antibacterial anti-inflammatory therapy, this contraindication has become relative, that is, according to modern concepts, it is not necessary to maintain absolute sterility of the surgical wound.
In cases where the shape of the socket coincides with the shape of the implant, the design features of modern implants with their gum formers make it possible to form the contour of the mucous membrane of the cervical area and prevent its growth into the implantation zone.
Use of dental membranes
In the vast majority of situations, there is a need to use osteoplastic materials and special methods for treating soft tissues. The lack of immune protection in the area of osteoplastic material before the onset of active angiogenesis with the final formation of the microvasculature requires measures to prevent peri-implantitis.
If microorganisms enter the peri-implant area, the bone material becomes an excellent substrate for bacterial growth, which quickly leads to disruption of osseointegration processes and loss of the implant. To prevent infection of the surgical field, insulating membranes made from modified biocomposite osteoplastic materials are used and have antimicrobial properties and antibacterial drugs in the postoperative period.
High-quality osseointegration of the implant occurs with complete overlap and subsequent preservation of the mucous-oxide flap or simply the presence of mucous membrane over the implant while maintaining all the walls and sufficient thickness of the alveolar process. High-quality osseointegration does not occur in areas with a significant deficiency of bone tissue (more than 1.5 mm), especially in the cervical area, with fenestrations or a significant fracture of the vestibular wall of the alveolus due to unsuccessful extraction.
Prevention of epithelial growth in the implantation zone, as well as isolation of osteoplastic materials from the negative effects of oral microflora, became possible only with the advent of biological membranes. The following types of membranes are distinguished:
- Non-resorbable membranes. Using non-resorbable membranes, bone tissue defects larger than 3 mm are restored. This type of membrane allows you to restore bone tissue within clearly defined boundaries. Having a rigid fixation contour, frame titanium membranes prevent collapse in the intervention site, thereby making it possible to restore bone tissue both vertically and horizontally in large volumes.
- Resorbable membranes include natural ones (collagen and laminated demineralized lyophilized bone), as well as certain synthetic ones (calcium sulfate, polymers). In the case of using the direct implantation technique, the use of resorbable membranes is more justified, since this technique produces the maximum possible atraumatic tooth extraction while maintaining the contour of the hole in the cervical area with a given height.
Special methods of tissue processing using osteoplastic materials are necessary for direct implantation with immediate loading. The spread of directed tissue regeneration made it possible to prevent not only the premature growth of epithelium into the surgical wound, but also the augmentation of the alveolar ridge. Modern advances in mucogingival surgery (techniques using pedicled flaps, island flaps) make it possible to ensure tissue regeneration.
Bone materials for direct implantation with immediate loading
General and local factors leading to progressive resorption of the jaws have necessitated the development of tissue transplantation and biomaterial science. The development of measures aimed at replacing bone defects in the human body, including the maxillofacial area, has led to the introduction of a number of bone grafting methods into dental practice.
These methods include the following:
- Autogenous transplantation, in which the transplantation of organic bone material occurs within the same organism.
- Allogeneic transplantation, in which the transplantation of organic material occurs from a genetically related organism (from person to person).
- Alloplasty, in which the replacement of bone defects is performed using materials of inorganic origin.
- Xenogeneic transplantation, in which organic material is transplanted from a genetically unrelated organism (animal origin, mainly cattle).
The use of osteoplastic materials for direct implantation with immediate loading has some features that will be discussed in more detail below, taking into account their capabilities and limitations.
Autogenous bone
The gold standard is the use of autologous bone, when the donor and recipient are genetically identical. Autogenous bone is the only material that immediately has the necessary osteogenic, osteoinductive and osteoconductive properties.
Osteogenic properties are inherent in grafts containing living cells that grow into the recipient site and stimulate the growth of new bone. Osteoconduction is the ability of a material to play the role of a passive matrix for new bone, that is, to serve as the basis for the maturation of bone tissue present in the defect. The listed characteristics are determined by the surface structure of the materials.
The osteoinductive properties of osteoplastic materials are manifested in the presence of morphogenetic proteins in them, which induce differentiation of mesenchymal cells from osteoblasts in the bed. This whole “triad of success”, osteogenicity, osteoconductivity and osteoinductivity, is characteristic exclusively of autologous bone.
Autogenous material is collected from both intra- and extraoral areas. When taking intraoral material, the ideal site is the mental triangle due to easy access and the presence of a thick layer of cortical bone containing more morphogenetic proteins than cancellous bone.
In the oral cavity, biomaterial is collected within the hill of the upper jaw and lower jaw in the area of the ramus and chin. From extraoral sites, long tubular bones are rarely used for collecting material; relatively often, the ilium is used.
The main disadvantage of using autogenous transplants is the need for additional surgical interventions, leading to injuries and psycho-emotional stress for the patient.
Allogeneic transplants
Allogeneic bone materials are also produced from human bone, but the donor and recipient differ in genetic aspects. This material can exist in mineralized and demineralized forms. Demineralized bone also exhibits osteoinductive properties due to easily diffusible proteins.
Despite all the advances in immunological and genetic diagnostics, cases of transmission of infectious diseases such as Creutzfeldt-Jakob disease, HIV and hepatitis C with bone tissue are still recorded. Low efficiency of using fresh allogeneic bone, the risk of transmission of infections, as well as the prohibition of the church in some regions of the world were forced to abandon such transplantation.
Despite these difficulties, cadaveric bone, after appropriate processing, is now widely used in domestic dentistry.
Alloplastic materials
Alloplastic materials include numerous synthetic products (hydroxyapatite, tricalcium phosphate, bioactive glass) or plant products of organic origin (seaweed, corals).
These materials are biocompatible, antigen-inactive, non-carcinogenic, also do not cause inflammatory reactions, are radiopaque, can be sterilized without loss of properties, and are resistant to high temperatures and humidity. They have only osteoconductive properties.
Xenogeneic bone materials
The appearance of xenogeneic materials after the experiments of Ollier, who transplanted bone fragments between different biological species, occurs in the second half of the 19th century.
Xenogeneic transplants are obtained from animals, so the donor and recipient are foreign in appearance. The main source of xenogeneic materials is cattle bones (Osteomatrix, Bio-Oss, Cerabone). Sometimes pork bones (OsteoBiol-MP3, The Graft) or horse bones (Bioteck) are also used.
There is a pattern: if bone tissue taken from animals belonging to a primitive species is transplanted into animals with a higher level of organization, the results are much better and more predictable than when bones are transplanted from highly organized animals to lowly organized ones.
The resorption time of these materials is also different. Resorption of material with simultaneous physiological replacement by bone tissue is a necessary phenomenon during implantation. But for some materials, complete resorption does not occur. It has been established that they remain included in the newly formed bone matrix.
After the advent of modern methods of production and sterilization, xenogeneic bone materials are widely used in dentistry, including the method of direct implantation with immediate loading. The presence of pronounced osteoconductive properties of xenogeneic materials has determined their advantage over other osteoplastic materials and made them the material of choice after autograft. Sufficient quantity, availability and safety also contribute to their use in surgical practice.
Role of sulfated GAGs
The method of preparation, micropore size, resorption time and properties of the above materials may vary significantly depending on the specific manufacturer and its product. Advanced domestic bone materials, such as Osteomatrix, have osteoinductive properties due to the presence of sGAG, or sulfated glycosaminoglycans.
Sulfated GAGs are an important component of the extracellular matrix. In the periodontium, they are located in the walls of blood vessels and along the entire periodontal membrane. Their content is especially increased in the area of the circular ligament of the tooth.
It has been established that the synthesis of sulfated GAGs always precedes the synthesis of collagen. Thus, when an additional amount of GAG is introduced, the cell immediately has the opportunity to begin the synthesis of collagen, which accelerates the repair process.
Sulfated glycosaminoglycans interact with collagen molecules and affect the formation of collagen fibers, which promote the laying of tropocollagen molecules in fibrils, and fibrils in fibers, while simultaneously limiting their growth in thickness. sGAGs stimulate angiogenesis, accumulate and release growth factors, bind calcium and control the mineralization of the organic bone matrix.
It has also been established that one hundred sGAGs have an anti-inflammatory effect due to the inhibition of enzymes that destroy the intercellular matrix and the biosynthesis of inflammatory mediators. sGAGs additionally support free radical inhibition. Recent studies have confirmed that sGAGs have an anti-edematous effect, which is ensured by the fact that GAG chains, due to their hydrophilicity, adsorb moisture, significantly reducing the swelling of surrounding tissues.
In addition, these bioactive molecules induce osteogenesis, which occurs by creating optimal conditions for the proliferation and differentiation of osteogenic cells and enhancing the action of growth factors.
Advantages of direct implantation with immediate loading
According to observations, during the first year after tooth loss, the width of the alveolar process bone decreases by 25%, and the total height loss is up to 4 mm. Long-term studies of edentulous patients over 25 years using lateral cephalograms demonstrate persistent bone loss. In this case, atrophy of the lower jaw bone can be 4 times greater.
According to Wolff's law, bone requires constant stimulation to maintain its shape and density and undergoes remodeling depending on the forces applied to the tissue. The parameters of the internal architectonics and external configuration potentially change with modification of this impact. The consequence of tooth loss with a corresponding decrease in bone stimulation results in a decrease in bone density and width.
Mechanical support and preservation of bone tissue in contact with the implant occurs subject to the physical presence of the implant. Taking into account the stress effects on the bone during the immersion of implants during direct implantation, the key determining factor in the success of treatment is the type of bone tissue.
Clinical studies on the survival of implants with identical designs and standard surgical protocols have not found the same results for all types of bone density. The density of the alveolar bone, as a consequence of the mechanical deformation that occurs during microstress, is significantly higher at the ridges around the teeth than in the periapical region.
Loss of bone density occurs not only after tooth loss, but also in the absence of occlusal load. Bone density will be higher if there is a root in the tooth socket, even without occlusal load.
Precise selection of an implant into the socket of an extracted tooth, the perimeter of which has denser bone tissue, improves primary stabilization regardless of the bone tissue biotype. Immediately after tooth extraction, there is a massive movement of cells with high osteogenic potential into the alveolus, coming from the exposed bone marrow spaces of the jaw and periodontal ligament.
If the tooth is in a normal position in the dentition, installation of the implant does not cause any difficulties, since it is placed along the extracted root in the socket, and the reduction in the invasiveness of bone drilling prevents overheating.
In addition to the clinical aspects of dental implantation, there is also a psychological aspect. Traditional fixed prosthetics has a negative impact on patients due to the need to prepare teeth adjacent to the defect.
Treatment according to a two-stage protocol involves the use of temporary orthopedic structures, causing discomfort when eating, talking or other everyday situations. In addition, with this type of implantation, complications are possible in the form of deterioration of osseointegration and reduced aesthetics of the implant-supported orthopedic structure.
An important advantage of direct implantation with immediate loading compared to other methods is the reduction of the psycho-emotional burden on the patient due to a reduction in the number of surgical interventions and the provision of the ability to quickly replace a tooth with an implant. Most patients accept an implant-supported prosthesis as an integral part of their own body.
Thus, using existing methods for installing implants, special tools, materials and auxiliary techniques, it is possible to create all the necessary conditions for high-quality and safe direct implantation with immediate loading, from tooth extraction to the installation of orthopedic structures.
HISTORY OF THE IMMEDIATE LOAD IMPLANTATION METHOD
This implantation method originates at approximately the same time as the classical one, but due to the fact that the commercial wave picked up the classical protocol, it is more common these days. But the more people suffer from bone atrophy, as well as the inability to restore teeth in an acceptable short time, the faster new approaches are developed. In 2011, the European Open Dental Society (ODC) together with the Institute. Tramonte, dr. Tomasz Grotowski (follower of the basal implantation school created by Dr. Garbaccio) and other colleagues, adherents of the Immediate load technique, improved the structure and technology of implantation. Their developments formed the basis for the creation of the ROOTT implantation system by the Swiss company TRATE AG. Being a member of ODC and taking an active part in developments, the center became the first clinical base in Russia to use the new technique on an exclusive basis
Where to go for basal dental implantation in Moscow
By choosing single-phase dental implants, we can count on a beautiful smile after the first visit to the dentist. Immediate loading implantation provides this unique opportunity.
Compared to classic implants, the basal implantation process takes much less time. Monoblock implants are immediately covered by a temporary prosthesis, so you don't have to wait months for a crown, bridge, or full denture to be placed on the implant. During the procedure, there is no need to cut the gum, and the absence of an abutment adapter between the implant and the crown eliminates possible problems arising from loosening of individual structural elements.
You can consult about basal implantation in Moscow at various dentists. Make your choice consciously, giving preference to the most reputable medical institutions. You can navigate the price level by studying the list of dental implant clinics presented below.
| Name | Clinic address | Service cost |
| ROOTT |
| Installation of a one-stage implant (Switzerland, Trate AG) with an adaptation crown - RUB 38,000. |
| Shandora | Moscow, Kolpachny lane, 6, building 4. |
|
| Dentistry Grand Smile | Moscow, st. Miklouho-Maklaya 43 (metro station Belyaevo, Yugo-Zapadnaya, Kaluzhskaya) | Astra Tech implants (Sweden) from 45,000 rubles |
| Dentistry MEDIKASTOM | Moscow, st. Znamenskiye Sadki, 1, K.1 (M. Dmitry Donskoy Boulevard) | Implantations NOBEL BIOCARE (Sweden) from 45,000 rubles |
| Dentistry "Doctor Martin" |
| From 65,000 rubles per tooth using Nobel screw systems |
We remind you that the success of dental restoration, including using basal implantation, largely depends on the patient’s behavior after surgery. Despite the fact that implantation with immediate loading is as gentle as possible, and the recovery period is fast, there are strict recommendations in this regard:
- After implantation surgery, do not eat or drink for 1-2 hours.
- Proper oral hygiene is extremely important, that is, thorough brushing of the teeth, but being as gentle as possible in the wound area.
- Do not use mouthwash unless your doctor tells you otherwise.
- Do not use any stimulants: alcohol and cigarettes.
- On the first day after the procedure, avoid physical activity, sauna, gym, swimming pool and hot baths.
Other jobs
Examples of work “Before” and “After”
Complex one-stage implantation of the lower jaw
Case: there was a loose bridge of 4 front teeth on the lower jaw; after diagnosis, removal of the remaining teeth and complex basal implantation were prescribed.
Dental restoration using basal implantation method
Case: complete absence of teeth in the upper jaw, bone atrophy.
Restoration of all teeth using basal implantation method (March 2012)
Case: partial adentia, exposed roots of natural teeth, periodontitis, increased tooth mobility, severe atrophy of bone tissue in some places beyond the possible norms for classical dental implantation.
Restoration of anterior teeth using basal implantation method (April 2012)
Case: partial absence of front teeth and destruction of supporting teeth under the prosthesis, the relief of the gums and interdental papillae is disturbed.