Periodontitis is an inflammatory disease that affects periodontal tissue. In dentistry, there is another disease with a similar name - periodontal disease. It is characterized by the same changes, but they develop without an accompanying inflammatory process.
Periodontal tissues include gums, blood vessels, ligaments and bones. All these structures securely fix the teeth and ensure their normal nutrition. With the development of the inflammatory process, these functions are disrupted, which leads to the appearance of specific symptoms. The main danger of periodontitis, like periodontal disease, is the development of tooth mobility with subsequent loss. Therefore, both diseases require early diagnosis and effective treatment.
Generalized periodontitis: symptoms and treatment
Periodontitis is a very common pathology of periodontal tissues (soft tissue structures around the dental unit). If the pathological process is started and left without treatment, then you can lose all the dental units.
Periodontal pockets are the best location for the emergence and development of an infectious process, which does not have the best effect on the healthy state of the body. A beautiful and healthy smile gives you self-confidence and makes you feel natural. When periodontal tissue is damaged, the gums become red and swollen. The disease affects the overall health of the body and the well-being of a person. If something bothers you in the oral cavity, you should immediately consult a specialist. Dentist therapists at the branches of the West Dental family clinic in Yanino-1 and Vsevolozhsk will help with identifying the origins of anxiety and their treatment.
It has been scientifically determined that the occurrence of periodontitis is influenced by: soft plaque and hard deposits; filling material or orthopedic structure fixed in violation of treatment protocols.
The main differences between acute and chronic periodontitis
Having considered the main characteristics of chronic and acute periodontitis, we can identify several main differences between these stages. Firstly, they differ in severity. Chronic periodontitis occurs slowly and often unnoticed by humans, while acute periodontitis is characterized by the suddenness and rapidity of damage to periodontal tissue.
Secondly, the factors that cause the disease vary significantly. Chronic periodontitis is caused mainly by general disturbances in the functioning of the body and bad habits, while the acute stage is provoked by mechanical damage to the teeth and gums due to injuries, certain types of dental diseases and improper installation of dentures.
Thirdly, the stages have different symptoms. If chronic periodontitis does not have a serious effect on the human body as a whole, then its acute form leads to intoxication, weakness, disrupting the usual course of life.
Fourthly, the localization of inflammation is somewhat different. In the chronic form, as a rule, the entire periodontium is affected to one degree or another, which is also typical for the acute non-purulent form. The acute purulent form is localized in a certain area of the oral cavity and leads to deepening of the periodontal pockets and significant swelling of the gums at the site of inflammation.
Fifthly, chronic and acute periodontitis require radically opposite measures of dental intervention. In the first case, regular preventative teeth cleaning at the dentist, treatment of the oral cavity with antiseptics to reduce the number of bacteria and relieve inflammation, physiotherapeutic procedures or treatment of periodontitis using the Vector apparatus are often sufficient. In the acute stage, it is often necessary not only to relieve inflammation, but also to remove a loose tooth, perform cavity surgery on the gums, or open the resulting fistulas and boils to remove pus. Patients often require consultation with an orthopedic dentist, who evaluates the possibility of installing dentures instead of extracted teeth.
Classification
According to the number of units affected by pathology:
- Catarrhal (localized) – 1-3 units in the affected area;
- Generalized – the entire dentition is affected.
According to the severity of generalized periodontitis (ICD code K05):
- Generalized mild periodontitis (ICD 10 code K05.3). This clinical diagnosis is made when the depth of the pockets in the gingival tissue is less than 3.5 mm, and less than 1/3 of the root is resorbed.
- Average. The subgingival depressions are 3.5-5 mm, and the bone is sclerosed at 50% of the root length.
- Severe degree. This stage is indicated by the depth of periodontal changes greater than 5 mm and resorption of more than 1/2 of the root.
Differential diagnosis according to pathogenesis:
- acute - more than one annual exacerbation;
- chronic generalized periodontitis (according to ICD K05) is an ongoing pathological process;
- exacerbation of chronic periodontitis – pain, discomfort, activation of the inflammatory process.
Classification and types of periodontitis
Depending on the characteristics of the course, the extent of the lesion and the severity, several forms of the disease are distinguished.
Acute and chronic periodontitis
The acute course of the disease is characterized by the sudden onset of severe symptoms that cause severe anxiety. Therefore, acute forms of periodontitis are considered relatively favorable, since patients seek medical help more often.
Chronic periodontitis, on the contrary, is prone to a long asymptomatic course. The symptoms are mild and patients may not pay attention to them. During periods of exacerbation, the clinical picture becomes more clear, but not all people make an appointment with a dentist. At the same time, the disease continues to progress, so sooner or later such patients will still need medical care.
Localized and generalized periodontitis
The extent of periodontal tissue damage may vary. If the inflammatory process spreads in one area of the jaw, then they speak of localized periodontitis. As a rule, in such cases one or more teeth that are located nearby are affected. Even with a long course, the localized inflammatory process, as a rule, does not spread to neighboring teeth.
With generalized periodontitis, all periodontal tissues (or most of them) on the upper or lower jaw are affected. This form is quite dangerous, since without proper treatment it can lead to the loss of most of the teeth. However, even if the patient seeks medical help in a timely manner, the problem cannot be solved quickly. Treatment of gum periodontitis in the generalized form is usually long-term and complex.
Degrees of periodontitis
Based on the severity of the disease, periodontitis is divided into 3 degrees or stages.
In mild cases, the general condition of the body remains unchanged. Local manifestations include periodontal pockets up to 3.5 mm deep, inflammation, redness and swelling of the gums. Pathological mobility of teeth is not detected.
Moderate periodontitis is characterized by an increase in the depth of periodontal pockets up to 5 mm, a decrease in the height of interdental septa, and the appearance of pathological mobility of teeth. At this stage, the patient may experience exposure of the neck of the tooth, gaps between the teeth, traumatic occlusion, and tooth displacement. The general state of health also changes. Patients may complain of weakness, fatigue, and poor appetite.
With severe periodontitis, manifestations reach their maximum. The depth of periodontal pockets is 6 mm or more. Due to significant bone resorption, severe tooth mobility and fan-shaped divergence develop. Complications in the form of abscesses also often develop, which affects the general condition.
The severity of periodontitis plays an important role in treatment planning, so it is always determined at the diagnostic stage.
Symptoms
The initial symptoms of the inflammatory process in periodontal tissues are the following:
- swelling of the gum tissue;
- severe bleeding during and after cleaning;
- throbbing severe pain.
As the pathology spreads, symptoms intensify:
- enlarged and painful lymph nodes;
- unpleasant odor from the mouth;
- mobility of dental units;
- increased sensitivity of tooth enamel;
- pain when biting and chewing food;
- deterioration of the general condition of the body;
- purulent discharge from periodontal pockets.
Chronic generalized periodontitis (beyond exacerbation) is characterized by:
- reddish color of gum tissue;
- exposure of tooth roots;
- Bone resorption is visually determined on the Rg image.
Publications in the media
Periodontitis is an inflammation of the entire complex of periodontal tissues, characterized by progressive destruction of the periodontium and alveolar bone tissue, and accompanied by the formation of pathological periodontal pockets.
Etiology. The most important local etiological factors include oral microflora (Porphyromonas gingivalis, Peptostreptococcus, Fusobacterium nucleatum, Veillonella parvula, etc.), dental plaque, anomalies in the position of teeth, bite, and others. Common disorders include diseases of the gastrointestinal tract, endocrine and nervous systems, metabolic disorders, and vitamin imbalance. Bad habits can contribute to periodontal damage. Pathogenesis. Periodontitis is always preceded by inflammation of the gingival margin (gingivitis). During the development of the pathological process, a violation of the epithelial attachment of the gum to the tooth occurs, destruction of the ligamentous apparatus, and resorption of the bone tissue of the alveolar process. A periodontal pocket is formed, which constantly deepens, reaching the root apex. Progressive resorption of alveolar bone leads to pathological tooth mobility. Destruction of the ligamentous apparatus of the tooth is accompanied by overload of individual teeth or groups, and traumatic occlusion occurs. With generalized periodontitis, gradual destruction of the entire complex of periodontal tissues occurs, which ultimately ends in tooth loss. Classification. According to the course, acute, chronic, aggravated periodontitis (including abscess formation), and remission are distinguished. Based on the severity of the process, they distinguish between mild, moderate, and severe periodontitis; according to its prevalence, localized and generalized.
Clinical manifestations. They are mainly determined by the severity and prevalence of the disease. • Localized periodontitis. It is characterized by aching pain, bleeding and severe swelling of the gums. Limited destructive inflammatory process in the area of one or several teeth (up to 5 teeth). Examination with a periodontal probe on all four sides of the affected teeth reveals a violation of the periodontal attachment and periodontal pockets of varying depths with purulent discharge or granulations. Tooth mobility of varying degrees appears. With exacerbations of the process, there is a sharp pain in the gums and alveolar part of the mucous membrane, painful percussion of the tooth, difficulty in eating and brushing teeth. If the outflow of purulent contents through the periodontal pocket is difficult, a periodontal abscess can form. • Generalized periodontitis. The initial stage is characterized by bleeding, swelling of the gums, pain in the gum area, bad breath and shallow periodontal pockets, mainly in the interdental spaces. In the developed stage of periodontitis, multiple pathological periodontal pockets of varying depths appear - with serous-purulent contents in chronic cases or abundant purulent contents in aggravated course of the disease. Based on the depth of these periodontal pockets, degrees of the disease are distinguished: I, II, III. Mobility of teeth develops, and subsequently traumatic occlusion is formed. Characterized by an abundance of soft dental plaque, supra- and subgingival dental plaque. Exposure of the necks and roots of the teeth may be accompanied by hyperesthesia. Sometimes retrograde pulpitis occurs. A chronic progressive course can lead to exacerbations accompanied by pain of a spontaneous nature. Abscesses and fistulas form one after another at intervals of several days. At the same time, changes in the general condition of the body occur—a rise in body temperature, weakness, and malaise. Enlargement and tenderness of regional lymph nodes are observed. The state of remission is characterized by dense gums of a pale pink color, possibly exposing the roots of the teeth. There is no dental plaque or discharge from pockets.
Diagnostics. In addition to clinical data, radiography (panoramic or orthopantomography) is of great importance. With localized periodontitis, destruction and foci of directed resorption along the tooth root are detected. In the initial stage of the generalized process, a compact plate is determined at the apexes of the interdental septa and an expansion of the periodontal fissure in the cervical region. The developed stage is characterized by resorption of interdental septa with a decrease in the height of the alveolar process and the formation of bone pockets; lesions of osteoporosis are detected. In the remission stage, the radiograph shows no signs of active destruction of the interdental septa; the bone tissue is dense. Differential diagnosis • Chronic gingivitis • Periodontal disease • Periostitis and osteomyelitis of the jaw.
TREATMENT Local treatment • It must begin with careful removal of dental plaque, especially subgingival plaque using a scaler (Pieson-master-400). It includes the whole range of local effects: medication, orthopedic and physiotherapeutic. Eliminate local causes that led to the development of inflammation. For longer contact of drugs with periodontal tissues, gingival dressings or forms with a prolonged action are used. • Of particular importance are surgical methods (curettage, gingivitomy, flap operations, etc.) performed on the gums and bone tissue, which are aimed at removing granulations, eliminating periodontal pockets, restoring defects in the bone tissue of the alveolar process, etc. Surgical intervention is recommended to be combined with drugs , promoting the regeneration of periodontal tissue (keratoplasty). Teeth that have mobility are splinted. It is mandatory to remove teeth that have no functional value. To avoid overloading the existing/remaining teeth, direct prosthetics are recommended. • Physical therapy can be varied, including ultrasound and low-level laser radiation. Hydrotherapy in the form of irrigation of the oral cavity with water saturated with carbon dioxide has not only a therapeutic effect, but also improves oral hygiene.
General treatment is mainly carried out for exacerbations of chronic generalized periodontitis and in the presence of severe general somatic pathology (hereditary neutropenia, type 1 diabetes, etc.). It includes: broad-spectrum antibiotics, desensitizing and sedatives, immunotropic drugs (imudon, xymedon). Sometimes hormonal therapy and drugs that affect mineral metabolism (thyrocalcitonin) are prescribed. General treatment is combined with specific therapy for the general disease and vitamin therapy. Prevention • Timely treatment of gingivitis • Careful oral hygiene • It is advisable to use resort factors (balneotherapy and peloid therapy). The physico-chemical properties of mineral waters, therapeutic mud and climatotherapy have a healing effect on the oral cavity and the entire body.
ICD-10 • K05.2 Acute periodontitis • K05.3 Chronic periodontitis.
Chronic generalized periodontitis
Chronic generalized periodontitis (according to ICD 10-K05) affects the soft tissue and bone structures of all or more dental units. The frequency of occurrence is 5 times higher than carious lesions and its possible complications. Also, a generalized process can most likely lead to complete edentia (lack of teeth). The long-term location of the infectious process in periodontal tissues, without proper treatment, negatively affects the body's immune defense and can contribute to the development of rheumatoid arthritis, heart disease, etc. Generalized periodontitis has a different etiology.
Diagnosis of periodontitis
Diagnosis begins with a consultation with a general dentist or periodontist. The doctor examines the oral cavity and prescribes additional examination, which may include the following methods:
- X-rays of the jaws. This basic examination provides general information about the condition of the teeth and bone tissue.
- Rheoparodontography. This method is used to determine the condition of the vessels of periodontal tissues.
- Ultrasonic osteometry. The study shows bone density.
- Schiller-Pisarev test. It involves staining the mucous membrane with a special solution that reveals foci of inflammation.
- Microbiological culture from the oral cavity. Allows you to determine the composition of microorganisms and their sensitivity to antibacterial drugs.
- Determination of periodontal index and bleeding index.
A comprehensive examination allows you to determine the degree of periodontitis, identify concomitant diseases and complications, and based on this information, plan further treatment.
Diagnostics
To determine the disease and its severity, various diagnostic methods are used. For generalized periodontitis, differential diagnosis includes an extensive consultation examination to draw up a medical history (formation plan):
- collection of complaints (mobility of units, discomfort when chewing, periodic sharp pain in the attached gum);
- visual and instrumental examination (gingival pockets, recession of gingival tissue, dental plaque, reddish gums);
- determination of the color, shape and structure of gum tissue;
- finding out what condition the dental units are in: percussion, palpation, degree of mobility;
- determination of hygiene indices;
- RG images.
Sometimes, a specialist may prescribe a blood test to clarify the etiology.
Diagnostic measures should take into account not only all the symptoms of the pathology and the patient’s complaints, but also the mandatory performance of an X-ray. Basically, in case of periodontitis, it is recommended to perform an OPTG (orthopantomogram) - a panoramic image. In such an extensive image, all dental structures and the degree of bone damage in each unit are immediately visible.
Mild degree
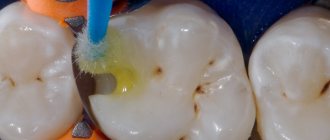
As usual, mild degrees are not given any importance. A subgingival pocket is formed near the dental unit, where microorganisms accumulate. There are signs of periodontal inflammation, and on the Rg image there is destruction of bone tissue by 1/3 of the root, gum pockets up to 3.5 mm. In the cervical area of the teeth, hard deposits are observed, the gums are loose, slightly inflamed and swollen. There is slight bleeding when cleaning, and discomfort when chewing solid food. Mobility and movement of teeth is not observed at this stage.
Average degree
With moderate severity, periodontal pockets up to 5 mm are observed. The x-ray shows damage to the bone septa on half the root. In the oral cavity, upon examination, there is a sufficient number of dental deposits, mobility of teeth I-II degrees, inflammation of the gums. A small amount of pus may ooze from under the gums. When the process worsens, slight mobility and displacement of units occurs.
Patients complain of pain in the gums; pain and bleeding when eating; the necks of the teeth are exposed; a reaction to cold and hot food is formed.
Severe degree
Chronic generalized severe periodontitis, as diagnosed, is determined by deep periodontal pockets over 5 mm and 2/3 of the tooth root being exposed. With this degree of pathology, great swelling, bleeding and hyperemia of the gums occurs, and eating is quite painful. In periodontal pockets there is a large accumulation of pus and microorganisms in the form of dental deposits. Patients have complaints of pain, itching, burning and pulsation in the gums. It is impossible to carry out high-quality hygienic cleaning on your own; a persistent unpleasant odor persists for a long time. In the absence of proper therapy, severe suppuration and mobility of grade III-IV units are observed, up to prolapse. Complications may develop in the form of abscess formation of foci of infection and periodontal disease.
Also, this pathology is manifested by a violation of the general condition of the body. A person is worried about weakness, fever, and in connection with this, fatigue. Regional submandibular lymph nodes enlarge and become painful on palpation.
Treatment
When the pathological process has taken the form of chronic generalized periodontitis, it is more difficult to carry out effective treatment. It is important to address the underlying cause of the disease. In this regard, the generalized form of periodontitis requires consultation with dentists in related fields to identify the source of the pathology. The general dentist/periodontist can provide recommendations for consultation with an endocrinologist, hematologist, immunologist, etc. After general interaction and identification of the cause of periodontitis, the attending physician prescribes the necessary therapy.
Treatment of the pathological process consists of the following measures:
- Professional oral cleaning and hygiene training. A specialist removes soft and hard dental deposits, including those under the gums. The tooth enamel is polished with special brushes with paste and coated with a protective gel with fluoride. Oral care products are selected and instructions on their use are provided.
- Treatment of associated dental problems. To cure periodontitis, it is important to treat caries, pulp disease, and pathological processes in the gums and bones.
- Drug therapy. Oral baths with solutions, application ointments, NSAIDs and painkillers, and sometimes antimicrobial drugs are used.
- Removal of subgingival pockets by a dental surgeon. In case of moderate and severe severity, it is possible to perform open and closed curettage of pockets, as well as gum plastic surgery.
- Treatment using orthopedic structures. As part of complex measures, temporary splinting of mobile units is performed with an orthodontic retainer or fiberglass; selective grinding of the chewing surfaces of teeth; prosthetics of large dental defects to redistribute chewing pressure.
- Physiotherapeutic manipulations. Many physiotherapy procedures have a positive effect on recovery: UHF, infrared radiation, magnet and laser therapy, electrophoresis, direct and alternating current, vacuum and acupressure massage, paraffin therapy, mud therapy.
For effective treatment of pathology and the occurrence of remission of the process, it is important to fully comply with the specialist’s instructions.
Treatment of periodontitis
Before treating periodontitis, it is necessary to carry out preparatory measures. These include the removal of supragingival and subgingival deposits, as well as sanitation of the oral cavity. Removing soft plaque and tartar is a mandatory step, since in this case one of the main causes of periodontitis is eliminated. Professional hygiene methods are used to clean teeth - ultrasonic cleaning, Air Flow cleaning, scaling, mechanical cleaning.
Sanitation of the oral cavity implies the elimination of all associated dental diseases. As a rule, most patients with periodontitis have caries and its complication – pulpitis. In the presence of incorrectly installed fillings, deformations and breakages of prostheses, correction is also carried out. The main task of the preparatory stage is to create the most favorable conditions for healing. This in turn affects the effectiveness of treatment.
To eliminate signs of periodontitis and restore normal dental anatomy, anti-inflammatory therapy, splinting and surgical treatment are used.
Anti-inflammatory therapy for periodontitis
Anti-inflammatory drugs can be prescribed locally or systemically. Local treatment involves rinsing the mouth and washing periodontal pockets with antiseptic solutions, and applying special gels to the gums. These procedures can be performed either in the dentist's office or at home. General therapy includes the prescription of tablets, injections or droppers. The main groups of prescribed drugs are non-steroidal anti-inflammatory drugs and antibiotics.
Splinting for periodontitis
Splinting is used to eliminate tooth mobility and prevent the progression of periodontitis. In this case, both temporary and permanent methods of fixing teeth can be used.
Temporary splinting
Temporary splinting is used in the presence of severe mobility, which is characteristic of severe forms of periodontitis. The goal of treatment in this case is emergency fixation of teeth and prevention of their loss. Today, modern and aesthetic materials are used as temporary splints - composite and acrylic. They are fixed using adhesive compounds and firmly hold the teeth together for several days. Temporary splinting does not require preparation and can be carried out in the shortest possible time. However, this design has a short service life. Therefore, in the future, temporary tires must be replaced with permanent ones.
Permanent splinting
With the help of permanent splints, you can fix your teeth for a long time. Such structures are installed after preparation, which consists of preparing (grinding) the teeth. Typically, the dentist makes a small depression on the inner surface of the dentition, into which a strong reinforced thread is installed and covered with a composite material. To increase strength, several threads can be used, which are laid in a special way (in several rows or in a figure eight shape). The service life of permanent tires is on average several years.
Semi-permanent splinting
Another method is semi-permanent splinting. As a rule, it is used to fix the front teeth. Structures can be removable or non-removable. Fixed splints are made of composite material and are attached to pre-prepared teeth with adhesive compounds. Removable splints resemble partial dentures with clasps in appearance. They are usually worn at night and used after surgery. Semi-permanent tires last from several months to a year.
Surgical methods for treating periodontitis
Surgical treatment is used to eliminate infected periodontal pockets that persist after conservative treatment. Typically, this situation occurs with deep pockets, intraosseous defects and other complications. Another group of surgical treatment methods allows you to get rid of defects in the gums and bone tissue. To achieve these goals, three main methods are used:
- Closed curettage. With this treatment, granulation tissue can be removed from periodontal pockets and the oral cavity can be cleared of subgingival deposits. Closed curettage involves mechanical curettage without making incisions. Among the disadvantages of this treatment is the lack of visual control. Therefore, closed curettage is not used for deep periodontal pockets due to low efficiency.
- Open curettage. Unlike the previous method, it is performed with gum detachment, which can significantly increase the effectiveness of the intervention. First, incisions are made in the mucous membrane, which allow the gums to be peeled off and granulations and dental deposits in the periodontal pockets are removed under visual control. If there are bone tissue defects, they can be eliminated in one stage, which is a significant advantage. However, open curettage is a more traumatic operation and has more contraindications.
- Flap operations. As the name suggests, their essence is to form a flap from the gums. This allows access to the underlying bone tissue and neck of the tooth. Depending on the characteristics of periodontitis, the dentist can perform bone grafting, remove areas of non-viable mucosa, and perform root grinding.
After surgical treatment, the patient needs postoperative care, which includes antiseptic mouth rinses, anti-inflammatory treatment and, in some cases, antibiotic prophylaxis. To consolidate the results of treatment, it is important to give up bad habits and eat right. For each patient, an individual list of recommendations is compiled that must be followed exactly.