Purulent sputum
Purulent sputum is a mucopurulent substance consisting of white blood cells, dead tissue, cellular debris, serous fluid and liquid mucus.
The color intensity of the purulent secretion can vary from milky with yellow to green, and manifests itself in pneumonia, bronchiectasis, abscess pneumonia, prolonged bronchitis or acute infectious lesions of the respiratory system.
A cough with purulent sputum is a good reason to consult a doctor, because if pus is coughed up, its shade will allow you to determine the pathology and choose the appropriate therapy.
- Yellowish-purulent and yellowish-greenish (mucopurulent) abnormal secretions indicate that antibiotic therapy will help reduce symptoms.
- A green or greenish tint indicates a long-standing respiratory infection, pneumonia, ruptured lung abscess, chronic infectious bronchitis, infected bronchiectasis, or cystic fibrosis.
- Bright yellow and orange mucus is produced by pneumonia (caused by pneumococcal bacteria), pulmonary embolism, bronchioloalveolar cancer, or tuberculosis.
- Discharge of a pale, milky, yellowish or yellowish-gray hue (clearly visible on a white background) indicates the ineffectiveness of antibiotic treatment, since the symptoms of the disease are associated either with a viral infection or with allergies (even asthma), and not with microbiotics that are sensitive to antibiotics .
- A foamy pink color is characteristic of severe pulmonary edema.
- Foamy white indicates pulmonary obstruction or edema.
- Light yellow sputum with blood indicates a possible inflammation of the throat or bronchi, or the presence of bleeding erosions, ulcers or tumors of the lower airways. The abundant presence of blood clots in bronchial secretions indicates tuberculosis, bipolar disorder, pulmonary embolism, and abscess pneumonia.
What is sputum? Which one is normal? Why is it needed?
The sputum takes on a yellow or yellowish-green tint if it contains impurities of pus, which indicates the development of inflammation, which is caused by a bacterial infection. The bright yellow (canary) color of phlegm is due to an increased content of eosinophils and is observed with eosinophilic infiltrative processes in the lungs or bronchial asthma.
The discharge of yellow mucus may also be due to subjective reasons. Tobacco and nicotine tars give the mucous exudate a yellow-rusty hue. Eating large amounts of carrots or citrus fruits can also cause the formation of large amounts of yellow exudate.
It is a thick, viscous, jelly-like substance that is released when you cough up. Secreted in the mucous epithelium of the lower airways by submucosal and unicellular glands.
Its composition includes high molecular weight glycoproteins, immunoglobulins, lipids and other substances. Simply put, phlegm contains:
- Impurities of saliva;
- Slime;
- Red blood cells;
- Fibrin;
- Epithelial cells;
- Bacteria;
- Foreign inclusions (dust particles, food residues, etc.).
The norm of phlegm released per day from the tracheobronchial tree is 10-100 ml. This is the amount of substance that a person ingests during the day without noticing.
Diagnosis of sputum by consistency and smell
In order to evaluate this criterion, it is necessary to expectorate sputum into a transparent glass container, evaluate it immediately, and then remove it, cover it with a lid, and let it sit (in some cases, the sputum may separate, which will help in diagnosis).
- Mucous sputum: it is released mainly during ARVI;
- Liquid colorless is characteristic of chronic processes developing in the trachea and pharynx;
- Foamy white or pinkish sputum is released during pulmonary edema, which can accompany both heart disease and inhalation gas poisoning, pneumonia, and inflammation of the pancreas;
- Sputum of a mucopurulent nature can be released with tracheitis, sore throat, bacterial bronchitis, complicated cystic fibrosis and bronchiectasis;
- Vitreous: characteristic of bronchial asthma and COPD.
An unpleasant odor is characteristic of complicated bronchiectasis or lung abscess. A fetid, putrid odor is characteristic of lung gangrene.
If the sputum separates into two layers when standing, it is probably a lung abscess. If there are three layers (the top one is foamy, then liquid, then flaky), this may be gangrene of the lung.
Folk remedies for coughs
When talking about how to treat a cough, we should not forget about traditional medicine. Some of the most accessible and effective recipes include:
- Infusion of coltsfoot. Preparation boils down to pouring 1 tablespoon of herb into 1 tbsp. boiling water, infuse for 10-15 minutes, strain. Take 1 tsp of this infusion orally. up to 4 times a day.
- An infusion of a mixture of plantain, thyme, elecampane root and wild rosemary herbs. 2 tbsp. dry mixture of herbs is poured with 1 liter of boiling water, infused for 2 hours, filtered. A solution of 1 tbsp is taken. orally up to 4 times a day.
- White cabbage juice. Freshly squeezed juice is mixed with honey in a 2:1 ratio. The finished mixture is taken orally, 1 tsp. 6 times a day.
- Lemon juice. Mix 2 tsp. product in a cup of warm water, add honey to this mixture, and take 3-4 times a day.
In addition, treatment for cough with yellow sputum involves frequent gargling with saline solution.
You need to dissolve 1⁄2 tsp. salt in a glass of warm water and gargle with the resulting solution as often as possible. This process clears trapped mucus.
Traditional treatment:
Diagnostics
If the patient suffers from phlegm in the throat without coughing, the reasons are determined by the doctor. Based on the results of the examination, a diagnosis is made, which is corrected with the help of certain medications, traditional methods and lifestyle changes.
Diagnostic measures include:
- examination (larynx, tonsils, oral cavity, nose);
- listening to breathing with a fanendoscope (determining wheezing or determining its absence);
- bacteriological culture of sputum;
- studying anamnesis, determining chronic diseases;
- blood test and instrumental studies (if necessary).
Other reasons
If sputum accumulates in the throat due to allergies, then you should take antihistamines (Suprastin, Cetirizine, Loratadine, Tavegil). Relief should occur within the first day of using them. If the symptom is caused by reflux and reflux of stomach contents, then treatment is prescribed by a gastroenterologist.
It will be individual for each patient (with the use of enzymes, anti-inflammatory drugs and dopamine receptor blockers).
You will also be interested in:
- How to treat a dry cough in an adult that lasts for a long time without fever
What diseases does it occur with?
Yellow thick sputum when coughing is observed with:
- Bronchitis - a certain color of discharge is characteristic of different types of disease. Yellow sputum during bronchitis is observed in acute or chronic form. The patient first develops a dry, then a wet cough. At the same time, sore throat, fever, and chills are observed.
- Cellulitis, abscesses, pleurisy - due to purulent processes, the discharge becomes yellow in color.
Any disease requires strict medical control.
Bronchial asthma
Signs characteristic of bronchial asthma.
- high-pitched wheezing when exhaling;
- difficulty breathing, chest tightness, cough that worsens at night;
- seasonal deterioration of the respiratory system;
- development of eczema or allergies;
- systematic colds that “descend” into the lower respiratory tract;
- the appearance or exacerbation of symptoms during physical activity, emotional overload, inhalation of polluted air, contact with allergens;
- stabilization of the condition after taking antihistamines and anti-asthmatic drugs.
Discharges in this disease differ in:
Sputum must be taken for analysis. Based on the results of the study, the nature of the disease is determined and a treatment method is selected.
A bright yellow or greenish color indicates the death of eosinophils, a type of white blood cell. When a vessel in the lung tissue ruptures, blood appears. With malignant tumors, a rotten smell is noted.
Pneumonia
Yellow sputum when coughing is characteristic of an acute form of pneumonia. It requires immediate medical intervention.
- elevated temperature;
- fever and chills;
- chest pain;
- sleep disturbance;
- persistent cough;
- feeling of lack of oxygen;
- sweating;
- weakness and loss of strength.
To diagnose the disease, an X-ray of the lungs is performed. To identify the pathogen, sputum culture, blood and urine tests are prescribed. Based on the results of the study, broad-spectrum antibiotics, anti-inflammatory and expectorant medications are prescribed.
Parasitic lesions of the lungs
- dirty hands and household items;
- unwashed food.
Larvae hatch in the gastrointestinal tract. They penetrate the veins and travel through the blood vessels to the capillary system of the lungs. The further path lies through the alveoli into the lumen of the bronchi, trachea and pharynx. A person swallows them along with secretions of the bronchial glands and saliva. The larvae return to the digestive system.
A cough that produces mucus may be caused by:
- concentration of parasites in the lungs;
- entry of larvae into the tissues of blood vessels of the respiratory organs;
- the presence of helminths that impede the access of oxygen in the bronchi;
- movement of larvae through the respiratory system.
Parasitic infection of the lungs provokes the development of diseases:
- pneumonia;
- exudative pleurisy;
- eosinophilic pneumonia.
The presence of heartworms is difficult to diagnose because symptoms often do not appear for several years. Some of the signs are characteristic of colds:
- temperature increase;
- paroxysmal cough in the morning;
- sputum discharge;
- loss of appetite;
- muscle pain;
- nausea.
To diagnose helminthic infestation at an early stage, a general blood test is performed. For bronchopulmonary syndrome, radiography is prescribed. The photographs show where the larvae penetrate into the tissue.
In the chronic stage, feces are examined for the presence of helminth eggs. This method is relevant no earlier than 3 months after infection. If only males, immature females or old individuals entered the body, then traces of their presence will not be found.Cough is a symptom that is familiar to everyone
It accompanies both the common cold and serious diseases, including diseases of the lungs, heart and even stomach.
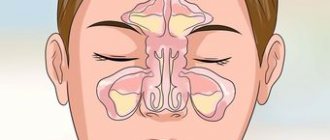
Most people prefer to treat their cough on their own. But not everyone knows that it is not the cough itself that needs to be treated, but the disease that led to its occurrence. A little anatomy A person takes about 20,000 breaths a day. At the same time, approximately 8000 liters of air enter the respiratory tract. The respiratory tract is divided into upper and lower: upper respiratory tract
- this is the nasal cavity
- pharynx (nasal, oral and laryngeal parts)
- larynx
lower respiratory tract
- these are the trachea and bronchi
Normally, about 2 liters of mucus are formed in the respiratory tract per day, which contributes to the natural cleansing of the respiratory tract. The mucous membrane of the bronchi is designed in such a way that the mucus, with the help of special cilia, rises up into the pharynx and is then swallowed. And from the upper respiratory tract (nose and nasopharynx), mucus freely flows down and is also swallowed.
If there is a violation of the mucous membrane (for example, smokers have no cilia in the bronchial mucosa) or any factors cause thickening of the mucus, then it cannot be excreted freely and stagnates. All this leads to irritation of the so-called. cough receptors (special cells that are involved in the cough reflex). It turns out that cough receptors are present not only in the respiratory tract, but even in the heart and stomach. Those. diseases not only of the respiratory tract will be accompanied by a cough.
Thus, a cough that occurs as a result of severe arrhythmia helps the patient not to lose consciousness and even helps restore the normal rhythm of heart contractions. What is a cough like? The cough can be constant and short, barking and silent... Coughs are also divided into wet (doctors call it “productive”) and dry (“unproductive”).
A wet cough produces sputum. It can be liquid or thick, mucous (transparent) or purulent (yellow, green). If the sputum is red or brown, contains streaks or blood clots, then this symptom is called hemoptysis. The amount and nature of sputum gives the doctor information about the cause of the cough. For example, thick green sputum indicates severe inflammation that should be treated with antibiotics.
And depending on whether sputum comes out at all, it will depend on what medications need to be prescribed. For example, if you have hemoptysis, you should not take expectorants, because they may increase the amount of blood in the sputum. And with a dry cough, the use of expectorants can intensify the cough, even to the point of suffocation. A cough that takes up to 3 weeks to cure is an “acute” cough; it most often accompanies ARVI. If the cough persists for more than 3 weeks, it is called “chronic.” Chronic cough is a sign of a serious illness.
Different diseases - different coughs.
Diseases of the upper respiratory tract The most common cause of cough is the familiar acute respiratory disease (ARI). The cough is usually dry, accompanied by pain and sore throat. A runny nose during acute respiratory infections can also cause coughing due to mucus draining down the back wall of the throat.
Bronchial asthma In approximately 10% of cases, the only manifestation of bronchial asthma is a cough.
With an exacerbation of bronchial asthma, a narrowing of the lumen of the bronchi occurs, which complicates the passage of air mainly during exhalation and leads to coughing, wheezing or attacks of suffocation. A typical cough is that it occurs at night and in the early morning hours.
Inflammatory diseases of the bronchi and lungs: bronchitis and pneumonia Inflammation and the presence of mucus in the respiratory tract leads to irritation of cough receptors during bronchitis and pneumonia. With these diseases, the cough is very rarely dry and is always accompanied by an increase in body temperature.
Smoker's cough Smokers are characterized by a cough in the morning with the discharge of thick sputum and frequent coughing throughout the day. If smoking has not led to the development of a chronic disease, then it is enough to give up the bad habit for the cough to disappear on its own.
Gastroesophageal reflux disease This disease causes the valve that separates the esophagus from the stomach to relax. Reflux is the reflux of food from the stomach back into the esophagus. Heavy eating, bending the body, and even singing can provoke the contents of the stomach to enter the esophagus. The acid contained in the gastric juice irritates the esophagus and can lead not only to heartburn, but also to cough. Sometimes a cough is the only sign that something is wrong with your stomach.
Cardiac cough Most heart diseases result in the heart not being able to pump the required amount of blood. Blood “stagnates” in organs, incl. and in the lungs. This leads to irritation of the cough receptors. A dry cough occurs, worsening in a horizontal position. The cough may be accompanied by palpitations, a feeling of shortness of breath, and shortness of breath. There is no treatment for such a cough; it will disappear on its own if the signs of heart failure are eliminated.
Cough due to medications Taking a number of medications can lead to side effects such as coughing. The reasons for this effect of drugs have not yet been sufficiently studied. It helps to recognize that medication has led to the development of a cough if there was no cough before the medication was prescribed. The cough bothers you mainly in the daytime, it is dry, and more often it is a small but debilitating cough. 3-7 days after discontinuation of the drug, the cough disappears. Cough with tumors Some lung tumors for a long time can manifest themselves only as a cough: dry or with the release of a small amount of light sputum. No changes are detected on radiographs of the lungs. Only visiting a doctor and carrying out special research methods helps make a diagnosis at an early stage.
Cough with whooping cough Whooping cough is an infectious disease that occurs with a prolonged paroxysmal spasmodic cough. In the first 2 weeks, the cough is similar to the cough of a common cold and may be accompanied by a runny nose and a slight increase in body temperature. Starting from the third week, a period of debilitating cough begins. The cough comes in attacks that are repeated from 2 to 15 times in a row. Such a cough must be treated, because... it leads to serious complications. Complications that a cough can lead to. Frequent persistent cough, especially in the form of prolonged attacks, leads to an increase in intrathoracic pressure and can contribute to the development of: - pulmonary emphysema - cardiac complications (arrhythmias, increased ischemia, development of cor pulmonale) - hemorrhage in the sclera of the eyes - dizziness - fainting - deterioration of cerebral blood circulation (especially if there have been previous strokes) - lung rupture
In addition, cough can lead to headache, vomiting, sleep disturbances, and urinary and fecal incontinence in an elderly, debilitated patient. Chronic cough can lead to the formation or enlargement of existing hernias (diaphragmatic, inguinal, scrotal, etc.). Chronic cough can cause depression, which complicates the patient's relationships with others, which ultimately significantly worsens the quality of life. What research needs to be done.
In order to avoid serious complications and make a timely diagnosis, you must consult a doctor.
Depending on the characteristics of the cough, its duration, and based on the results of the examination, the doctor will prescribe an examination. As a rule, this is a clinical blood test, fluorography and a study of external respiratory function. If the results of these studies do not help determine the diagnosis or even during the examination one can suspect that they will not be enough, the doctor prescribes more complex studies (for example, bronchoscopy, computed tomography, lung scintigraphy) and consultations with specialists. You can hardly find a person who has never coughed. And, of course, there is no need to consult a doctor every time at the first sign of a slight sore throat or slight cough. These disorders are transient. However, it should be remembered that only a doctor can reliably recognize the cause of cough and prescribe the necessary treatment.
Symptoms that should alert you and prompt immediate medical attention: - hemoptysis (sputum is uniformly red or with red/brown streaks) - increased body temperature for more than 3 days - choking or shortness of breath - cough for more than 3 weeks - chest pain - nausea and vomit"
Analysis of yellow sputum: diagnosis. How is it researched?
Samples of secretions taken from the throat for analysis make it possible to determine the cause of changes in the shade and consistency of tracheobronchial secretions.
The material is collected in a sterile glass container in the morning on an empty stomach, after thoroughly treating the mouth and throat with saline solution. If it is not possible to collect pathological clots during coughing, bronchoscopy is prescribed to obtain the necessary material.
Sample examination is carried out using several methods:
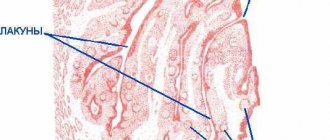
Microscopic analysis makes it possible to determine the content of leukocytes, erythrocytes, alveolar macrophages, epithelial cells in phlegm, detect Kurshman spirals, drusen of actinomycetes, fungi, Charcot-Leyden crystals, eosinophils, neutrophils. Macroscopic analysis determines the daily volume of secreted exudate, its smell, density and color
Special attention is paid to the delamination of the material when left in glass containers for a long time. Bacteriological analysis (Bakposev) allows you to determine the types of bacteria present and their sensitivity to drugs
Causes of mucus discharge when coughing
Blood in sputum almost always becomes a sign of dangerous diseases of the respiratory system. An exception can be considered a rupture of a small bronchial vessel, which occurs during severe physical overload or a sharp, hysterical, barking cough. Usually the sputum in this condition is brown. Treatment is simple - anticoagulants are used.
Relatively safe sources of a frightening symptom include complications after improperly performed medical procedures. Blood in a cough can be a consequence of bronchoscopy, arterial catheterization, or pulmonary puncture. Such hemoptysis begins unexpectedly, usually the next morning after diagnostic or surgical operations. The pathological symptom goes away without drug treatment.
Lung diseases that cause blood in the sputum when coughing
Almost always, the doctor begins the diagnosis with a test for tuberculosis. In addition to blood in the cough, this disease is accompanied by increased sweating, increased body temperature, and sudden weight loss.
If such a disease is not confirmed, the doctor will prescribe additional tests to rule out:
- traumatic injury to the lung (a dangerous condition accompanied by a decrease in blood pressure, pain, and breathing problems);
- infectious, parasitic, fungal infection (in addition to blood clots in the sputum, the patient complains of general weakness, bronchial obstruction, allergic manifestations);
- adenomas in the bronchi (hemoptysis is accompanied by discharge of pus in the mucus when coughing, hiccups, and a constant feeling of fatigue);
- heart attack, lung abscess (streaks of blood in the sputum have an unpleasant odor, tachycardia, cyanosis, severe shortness of breath, fever occur);
- pneumonia (blood in the mucus appears when infected with staphylococcus, legionella, pseudomonas);
- cancer (prolonged cough with blood discharge may indicate lung cancer).
Blood in the sputum after bronchitis often occurs after improper treatment of the disease. A symptom is considered the body’s first “bell” about the transition of the disease to the chronic stage or an exacerbation of the acute form.
Rare respiratory diseases
After collecting anamnesis, the doctor recommends undergoing a comprehensive examination for unpopular lung diseases. Blood in sputum may be a sign of bullous emphysema, silicosis, foreign body aspiration, or aploidosis. Such diseases are usually accompanied by additional symptoms. During the medical history, the doctor asks questions about shortness of breath, heaviness in the chest, dizziness, loss of coordination, and tinnitus. A visual examination is carried out to determine widened intercostal spaces and changes in the shape of the chest.
Cough with blood in diseases of the heart and blood vessels
The cause of the appearance of uncharacteristic secretions in the mucus may be a change in the condition of the heart and blood vessels
It is important to promptly identify and begin treatment of pathologies such as mitral stenosis, aortic rupture, cardiac outflow of the lung, and blockage of arteries during a heart attack. In addition to the appearance of blood in the sputum, the described diseases are characterized by significant shortness of breath, pain
Most often, the cough worsens after physical activity.
Coughing up white mucus without coughing
Enveloping the larynx with white mucus without a reflexive attempt to remove it is a common reason for patients to see a doctor. Most often, this is pure physiology, not dangerous to health: unfavorable ecology, food irritating the mucous membranes, alcoholic drinks.
If, in addition to sputum, cold symptoms appear: runny nose, headache and fever, this is a reason to consult a doctor.
Most likely, acute respiratory infections provoked an exacerbation of a latent process, which is localized in the upper respiratory tract and does not manifest itself in anything other than hypersecretion of mucus. The pathology does not descend into the bronchi, so there is no cough. But such “innocence” may hide tumors of the nasopharynx, so consultation with a specialist is necessary.
For prevention purposes, any expectoration of white mucus without coughing for a couple of days is a reason to visit a therapist.
An examination with special equipment and a series of tests will allow you to determine the true cause of hypersecretion and prescribe therapy or send you to a specialized specialist.
If you cough up green sputum: treatment
How to treat a disease depends on the causes of its occurrence.
At the same time, patients are often recommended not only classical drug therapy, but also a number of special procedures that can be easily performed at home.
For bacterial infections, antibiotics are prescribed (Augmentin, Flemoxin, Lincomycin, Unidox, Sumamed, Azithromycin, Cefix, Cefuroxime, Hemomycin, Ampiox, Doxycycline, Clarithromycin, etc.), which will help get rid of pathogenic microflora, as well as:
- mucolytics: ACC, Fluimucil, Mucaltin, Carbocysteine, Fluditec, Pectolvan, Prospan, Acetin, licorice root syrup, Libexin Muco;
- expectorants: Ambroxol, Lazolvan, Ambrohexal, Ambrobene, Gedelix, Bromhexine, Flavamed, Doctor Mom, dry medicine, Pertussin, Herbion primrose syrup;
- antihistamines: Zodak, Erius, L-cet, Suprastin, Edem, Loratadine, Claritin, Tavegil, Aleron, Alergodil, Fenistil, Cetirizine;
- immuno-strengthening: Umkalor, Aflubin, Isoprinosin, Lavomax, Oscilococcinum, Amiksin, Anaferon, Immunal, Proteflazid, Immunorix, Derinat, tinctures of echinacea, ginseng, lemongrass, etc.
It would not be superfluous to carry out inhalations using a nebulizer or improvised means, for example, a pan of boiled potatoes.
What medications should be used for inhalation therapy in a nebulizer are prescribed to the patient by the doctor; as part of self-medication, only saline solution is allowed.
If there is no fever, it is useful for patients to walk in the fresh air. Required:
- ventilate the room;
- drink plenty of warm drinks;
- use household humidifiers.
More serious pathologies, such as tuberculosis, are treated in hospitals according to specially developed schemes.
Cough with green sputum in adults
Treatment of colds in adults requires bed rest, as otherwise undesirable consequences may develop.
This will allow you to cure the disease in the shortest possible time with minimal risk to the body.
It is much more difficult to carry out therapy for expectant mothers. Nevertheless, it is they who need it in the first place, since frequent coughing attacks can increase the tone of the uterus and in certain women provoke the threat of miscarriage.
Therefore, during pregnancy, self-medicating and not paying attention to the problem is strictly prohibited.
In such cases, you should definitely contact a therapist, who will select medications that are acceptable for this period.
Child coughs up green mucus
As a rule, pediatricians recommend supplementing drug treatment for a child with a special massage:
The baby is placed on his stomach on the adult's lap, while he must rest his hands on the floor and raise his legs as high as possible. An adult initially rubs the baby's back with light movements until a feeling of warmth and barely noticeable redness appears. Using light tapping movements with the fingers of a relaxed hand, the adult begins to actively hit the child’s back for several minutes.
It is very important to control the force of the impact: they should be noticeable, but not painful.
The effectiveness of this massage has long been proven. Most children begin to cough more easily within a few minutes of completing the procedure. Here's a video:
https://youtube.com/watch?v=7RFEP4cbKLc
You should not force feed your child if he refuses to eat. During illness, the body spends all its energy fighting microbes, and eating food leads to a redistribution of energy costs and a decrease in the quality of the fight against infection.
Breathing with turbulence and friction
Chief, I can hear you
Bronchial breathing is a sound phenomenon that occurs when air turbulence passes through the larynx, and is also the site of the division of the trachea into two main bronchi (tracheal bifurcation). Since zones of turbulence occur both during inhalation and exhalation, bronchial breathing is clearly audible both in the first phase of breathing and in the second.
You've probably noticed that the doctor doesn't listen to the lungs at one point, but strives to poke the stethoscope all over the back, and in young beautiful girls he listens especially intently to the lungs in front. In general, he is not doing this out of a good life, believe me. Our lungs are rather large, and the doctor needs to determine whether the noise is heard over their entire surface or whether it is localized. Is one type of breathing heard everywhere, or is there an alternative somewhere?
A striking example of such an alternative is bronchial breathing. As we have already said, normally vesicular breathing should be heard over the entire surface of the lungs. Let me clarify: almost all of it. Above the larynx, in the projection of the trachea and especially in the projection of its bifurcation - the level of the IV-V thoracic vertebrae (in young beautiful girls - this is right at the very top of the cleavage;)) bronchial breathing is normally heard. Sometimes, to distinguish it from pathological bronchial breathing, it is called laryngo-tracheal breathing. That is, the laryngo-tracheal is somehow the norm, but the bronchial is no longer the norm.
Let me emphasize once again that normally bronchial breathing should not be heard over other parts of the lungs. If it appears somewhere else, it means there is a problem in the lungs. Most often, associated with compaction of the lung tissue (under such conditions, sounds are conducted much better than through air lungs).
Depending on the severity of the process, bronchial breathing may overlap with vesicular breathing, or may completely displace it. What can cause hardening of lung tissue? Pneumonia, first of all. Especially massive, lobar, for example.
In addition to pneumonia, compaction of lung tissue can cause tuberculosis, pulmonary infarction, compression atelectasis of the lung (collapse of lung tissue and compression of the lung to its root), pneumosclerosis (when lung tissue is replaced by connective tissue).
To be fair, it should be noted that bronchial breathing can rarely be heard over the entire surface of the lungs. Most often, it is perfectly audible above the source of compaction, and if you move to the side, its volume drops exponentially. This fact helps the doctor to say with a certain degree of probability where exactly the problem is located.
Amphoric breathing is also a variant of pathological bronchial breathing. It can be heard if a cavity in the lung (5-6 cm in diameter, usually smooth-walled) connects to a bronchus. A cavity can appear, for example, with a lung abscess.
Essentially, we get the Pan Flute element. The air passes over the opening of the cavity - and we hear a fairly loud and somewhat musical sound.
The old professors mentioned more than once suggested taking an empty champagne bottle and blowing over its neck. The sound is almost the same as with amphoric breathing.
It's cold!
Fortunately, quite rarely, there are disturbances in the innervation of the respiratory muscles. With such a pathology, they do not all work at the same time, but one by one, step by step. As a result, we get a stepped inhalation. Our exhalation is passive, muscles are not particularly needed there, so the second phase of breathing is usually not changed.
This type of breathing is called saccoded.
But in the overwhelming majority of cases, saccoded breathing is explained by completely normal and not at all pathological reasons. First of all, the cold. It’s good for the doctor, under his coat he may have not only a fiery heart, but also, for example, a woolen vest. But the patient has no choice, he has to be naked to the waist (from above), even if it is not hot in the office or ward, to put it mildly. The muscles begin to engage in tremulous thermogenesis, resulting in saccoded breathing upon auscultation.
Therefore, it is recommended to examine patients in a more or less warm room. And warm the head of the phonendoscope in your hands before applying it to the patient’s skin. For experienced therapists, this is already at the level of automation: you interview a person, and the stethoscope warms up in your hand.
Another option is people who, when they see a doctor, begin to get terribly worried. And again we hear saccoded breathing. Again, if the patient sobs before the doctor arrives, then for some time he will again experience saccoded breathing. And again, the reason is not illness at all, it’s just the consequences of crying.
Well, to figure out whether it is a violation of the innervation of the respiratory muscles or recent crying - this is precisely the art of the diagnostician.
Noise maker mouse
And now we move on to the most notable noisemaker in the lung area. As you know, our lungs are covered with a kind of elastic film - pleura. And the chest cavity is lined from the inside with the same pleura. Between these two layers there is a small cavity, which is called the pleural cavity. Both leaves are coated with a small amount of lubricant to facilitate breathing movements.
If the pathological process is localized not in the depths of the lungs, but on the surface, the pleura covering the lungs can also become inflamed. In this case, the lubrication can either disappear (as with the rapid loss of a noticeable amount of fluid by the body - cholera, blood loss, indomitable
vomiting and other delights), or fibrin may be deposited on the surface of the pleura, adhesions and scars may occur (tuberculosis, cancer, etc.).
As a result, the sliding of the pleura becomes no longer so easy and carefree. And not so silent.
Pleural friction noise is one of the loudest sound phenomena. Already annoying, the old professors compared it to the crunch of snow on a frosty day. Amazingly accurate definition.
Distinctive features - does not disappear when coughing, is clearly audible both on inhalation and exhalation, if you press with the head of the phonendoscope, the pleural friction noise will intensify. Thus, it can be distinguished from fine moist rales and crepitus. There is another sadistic technique: cover the patient’s mouth and nose and ask him to imitate breathing movements with his stomach, perhaps accompanied by music. The pleural friction noise will remain, but there will be no wheezing or crepitus. The main thing with this technique is to quickly run away after it is completed.
Most often, pleural friction noise is heard in places of greatest amplitude of respiratory movements, that is, from below on the sides. Much less often (with tuberculosis) it can be detected in the area of the apexes of the lungs
Smokers
Mostly brown sputum appears in a smoker in the morning. When a person sleeps, mucus accumulates, and when he wakes up, phlegm begins to leave the bronchi naturally. A person who smokes for a long time eventually develops so-called smoker's bronchitis. Moreover, the cough becomes his constant companion. Naturally, smokers do not monitor their health, so they do not pay due attention to the color of the discharge. They are accustomed to a morning cough and do not consider this a cause for concern. However, brown sputum is considered an ideal breeding ground for bacteria.
Thus, by introducing harmful smoke into the body, smokers slowly poison it with heavy elements. Therefore, it is better to give up such a bad habit in order to exclude more serious diseases and complications in the future. People who have continuously consumed harmful cigarette smoke for several years in a row need to cleanse their lungs. To do this, you can use breathing exercises, which are popular today, with which you can improve the health of the entire body. The doctor may also prescribe you expectorant medications or a more gentle healing option using inhalations. Visit the clinic and the doctor will tell you which method is best for you. The doctor will monitor your health throughout the course of therapy, so no complications will arise.
How is endoscopic septoplasty performed?
The essence of the operation is to excise those areas of bones and cartilage that have been deformed. The mucous membrane is not subjected to excision, since it is pre-exfoliated, which allows its integrity to be preserved and the rehabilitation period to be significantly reduced.
Modern medicine allows surgical intervention to be performed in an extremely gentle way, so in most cases only that part of the septum that is deformed and causes discomfort is excised.
The operation is performed using an endoscope. During the intervention, a thorough examination of the deformed area is performed. The necessary areas are removed using low-traumatic microtools. The operation is monitored using an endoscope.
Causes of phlegm in the throat
The most common cause of constant mucus is acute infectious diseases, colds. During the first days, sputum is produced abundantly from the nose, and later from the bronchi and trachea. Such discharge is temporary and stops after recovery. If there is no acute disease, but mucus is formed steadily, we can talk about pathology, an unhealthy lifestyle, or the development of some complex disease.
Lump in throat when swallowing
Patients complain that mucus constantly accumulates in the throat, something foreign is stuck. For this reason, they cannot swallow completely and experience great discomfort from this. The main reasons causing this symptomatology:
- Disorders of the thyroid gland caused by iodine deficiency (diffuse goiter, autoimmune thyroiditis).
- Gastrointestinal pathologies (ulcers, reflux disease, gastritis).
- Neurological reasons. A feeling of “choking the throat” can occur, for example, with osteochondrosis of the cervical spine.
- Chronic tonsillitis, sinusitis, purulent plugs.
- Depression, stress and other psychological problems. Women often feel a lump in their throat during pregnancy.
- Oncological diseases.
Snot in throat
This unpleasant symptom greatly complicates life: it interferes with eating and provokes coughing. When mucus flows down the back of the throat and accumulates in the nasopharynx, we can assume the presence of:
- bronchopulmonary diseases;
- inflammatory processes of the sinuses (pharyngitis, sinusitis);
- diseases of the esophagus (chronic esophagitis);
- allergic reactions;
- various types of irritations (if a person smokes a lot, eats spicy dishes, the body turns on a “defensive reaction” - mucus begins to actively cover all organs).
No cough
If sputum appears, but there is no cough, none of the above causes can be excluded. The disease is provoked by diseases of the respiratory system, gastrointestinal tract, inflammation of the tonsils, colds, lifestyle, and stress. If the mucus in the throat does not clear up, the reason for this may be low air humidity, foreign objects in the nasal cavity, and various muscle diseases.
With an unpleasant odor
According to research, excess mucus and sticky saliva feed the bacteria in the throat, which is the source of the unpleasant odor. Among the main reasons:
- colds, chronic runny nose, sore throat;
- diseases of the gastrointestinal tract;
- bad teeth;
- chronic tonsillitis and other diseases of the nasopharynx;
- pathologies of the nasopharynx, sphenoiditis.
If your throat hurts
The cause of phlegm can be bacterial throat infections and inflammatory processes (tonsillitis, pharyngitis). If a person has a sore throat, a cough, laryngitis is possible. There are other reasons that cause pain and accumulation of mucus - for example, glossopharyngeal neuralgia, tumor processes, thyroid diseases. With these diseases, no increase in temperature is observed.
With blood
Inflammatory diseases of the upper respiratory tract, accompanied by damage to small vessels
To determine the exact cause, you need to pay attention to the color of the sputum. For example, if it is yellow or green mixed with blood, it means that a person has chronic inflammatory diseases
White mucus with blood may be a sign of bleeding in the esophagus or lungs. Viral diseases of the respiratory tract. Severe cough and other reasons leading to rupture of small vessels. Thrombosis, mitral pulmonary artery defects. Lung diseases (bronchitis, tuberculosis).
Laryngopharyngeal reflux in gastroenterological practice
Gastroesophageal reflux disease (GERD) is one of the most common pathologies of the gastrointestinal tract. At the International Congress of Gastroenterology, held in Montreal in 2005, a unified definition of the disease, a description of symptoms and a classification of the disease were developed, which formed the basis of the Montreal Consensus [1]. The Consensus divides the clinical manifestations of GERD into esophageal and extraesophageal syndromes. The presence of reflux-associated symptoms in the absence of damage to the esophageal mucosa is regarded as esophageal syndrome, manifested solely by symptoms, and in the presence of damage to the esophageal mucosa - as esophageal syndromes with damage to the esophagus (complications). Extraesophageal syndromes were divided, in turn, into syndromes whose connection with GERD has been established, and syndromes whose connection with GERD is suspected. Extraesophageal syndromes with an established connection with GERD include reflux cough, reflux laryngitis, reflux asthma and reflux-induced destruction of tooth enamel, and syndromes with a presumptive connection with GERD include pharyngitis, sinusitis, pulmonary idiopathic fibrosis and recurrent otitis media [ 2, 3].
The word “reflux” itself literally means “reverse flow”. GERD is detected in many patients with chronic laryngitis. Otorhinolaryngologists often refer to this condition as laryngopharyngeal reflux (LPR), which represents the retrograde entry of stomach contents - acid and pepsin, as well as bile acids into the laryngopharynx [4, 5]. There are a number of synonyms for LPR, such as extraesophageal reflux, reflux laryngitis and laryngeal reflux. There is currently no gold standard for diagnosing LPR, and therefore data on its epidemiology are limited. In one study of 105 normal healthy volunteers, 86% had laryngopharyngeal reflux during laryngoscopy [6]. In a meta-analysis by AL Merati et al. analyzed data from pH probe readings in 264 patients with LPR; as a result, gastroesophageal reflux was detected in 10–60% of patients [7]. Studies such as these show that LPR is common in the general population, but needs to be diagnosed in some patients before adequate treatment can be given.
Normally, the upper esophageal sphincter and, to some extent, the larynx protect the lower respiratory tract from the entry of contents from the esophagus and stomach. The larynx is very well innervated and any esophageal reflux in a normal person will cause a protective cough. In patients with LPR, this “safety mechanism” may fail. For example, JE Aviv et al. The study showed that sensory deficits may play a role in the formation of LPR. The authors found a decrease in the laryngeal reflex in response to endoscopic air insufflation in patients with documented LPR [8]. Most researchers propose two main pathophysiological mechanisms for LPR, which directly or indirectly cause damage to the larynx by the contents of the esophagus and stomach. The direct mechanism is the result of the action of gastric contents (acid, pepsin and/or bile acids) acting directly on the mucous membrane of the hypopharynx. The indirect mechanism manifests itself as a result of the effect of reflux on the reflex structures of the larynx. This irritation is thought to cause bronchospasm, which in turn stimulates the vagal response, usually resulting in a nonproductive cough. The delicate ciliated epithelium of the posterior wall of the larynx, which normally evacuates mucus from the trachea, is significantly damaged by contact with gastroduodenal chemical agents, which can lead to mucous stasis in the larynx and discomfort [9]. Recently, it has been suggested that the enzyme carbonic anhydrase, which stimulates bicarbonate secretion, protects laryngeal tissues from reflux and that this protective mechanism may be impaired in the larynx of patients with LPR [10].
Most patients diagnosed with LPR may not have the classic symptoms of GERD. The main symptoms of LPR are respiratory complaints such as pain or burning in the throat, chronic cough (51%), excessive expectoration of mucus (42%), dysphonia (71%), dysphagia (35%), lump in the throat (47%), vertical (daytime) reflux, laryngospasm [11]. Researchers estimate that up to 50% of patients with laryngeal and voice disorders have reflux [12]. Based on laryngoscopy data, a special scale of “reflux signs” (SRS) was developed in 2001, which included 8 characteristic laryngoscopic symptoms with a general assessment of their severity from 0 to 26 points, which are presented in table. 1 [13]. Conducted by MF Vaezi et al. studies have shown that the presence of more than 7 points on the SRS correlated by 95% with positive data from 24-hour esophageal pH monitoring and suggested the presence of LPR [14]. Many patients with LPR often turn to a phoniatrist because they do not have pathognomonic complaints. If a patient’s dysphonia continues for more than three months, he or she should be screened to detect LPR [15].
Unfortunately, the specificity of laryngoscopic findings and their assessment using the presented SRS is not very high [6]. In 2002, the authors who developed the SRS also proposed the “Reflux Symptoms Index” (RSI) questionnaire, recommended for assessing the effectiveness of LPR treatment with proton pump inhibitors (PPIs), which consists of 9 questions and includes a dynamic assessment of a number of indicators (Table 2). Each IRS symptom is rated over the past month on a scale from 0 (no problems) to 5 (severe problems). A score of more than 13 correlates with a positive result of pH monitoring [13]. It is a self-administered tool that helps clinicians assess the clinical severity of LPR symptoms at diagnosis and then over time after treatment. The IRS is significantly higher in patients with LPR than in healthy controls (21.2 vs. 11.6, p < 0.001). However, this indicator is rarely used by general practitioners and otolaryngologists [16]. In 2004, R. Williams et al. proposed a scale for assessing the severity of chronic laryngitis in otorhinolaryngological manifestations of the extraesophageal form of GERD: degree 0 - no signs of inflammation, degree I (mild) hyperemia and/or swelling in the area of the arytenoid cartilages and interarytenoid space, degree II (moderate) - distribution of hyperemia and/ or edema beyond the area of the arytenoid cartilages and the interarytenoid space to the vocal folds, degree III (severe) - the presence of ulcerations in the area of the arytenoid cartilages and the interarytenoid space or the spread of the inflammatory process to the subvocal part of the larynx [17].
As is known, the most sensitive test for practical diagnosis of pathological acid gastroesophageal reflux is daily intraesophageal pH monitoring, when intraesophageal pH is continuously recorded at a distance of 5 cm above the lower esophageal sphincter. As a standard test for diagnosing LPR, ambulatory 24-hour intraesophageal hypopharyngeal pH monitoring using two pH sensors is proposed, with the second (proximal) pH sensor for fixing supraesophageal reflux as a cause of ENT disorders installed 5 cm above the upper alimentary sphincter (VPS) [18]. Unfortunately, although hypopharyngeal pH monitoring is a more sensitive test for identifying patients with GERD-induced ENT disorders, negative results cannot exclude LPR due to the intermittent nature of the disease and variability. Currently, a more accurate and patient-friendly method for diagnosing LPR has been developed by measuring naso- and oropharyngeal pH using a special Restech's Dx-pH measurement system, which allows recording pH fluctuations in the oral cavity and nasopharynx every 1/2 s for 48 hours [14 , 19].
Treatment of patients with LPR should include diet, lifestyle modifications, physical therapies, and pharmacotherapy. Modification of diet and lifestyle involves the patient following the following recommendations:
- after eating, you should avoid bending forward, you should go to bed with your head elevated;
- do not wear tight clothes and tight belts;
- avoid large meals;
- do not eat at night;
- limit the consumption of foods that cause a decrease in the pressure of the lower alimentary sphincter (LES) and have an irritating effect (fats, alcohol, coffee, chocolate, citrus fruits);
- stop smoking;
- normalize body weight.
Foods and drinks containing caffeine, alcohol, chocolate and mint relax the lower esophageal sphincter and increase stomach acid production, while carbonated drinks with/or without caffeine increase reflux and belching. In addition, the intake of acidic foods (with a pH below 4.6), such as citrus fruits and other sour fruits, tomatoes, dry wines and some others, should be limited. Lifestyle modifications that can reduce symptoms of LPR, as well as other manifestations of extraesophageal reflux, include smoking cessation and weight loss. A study by DL Steward et al. [20] showed that lifestyle changes for 2 months or more, with or without PPI therapy, significantly reduced the symptoms of chronic laryngitis.
Drug therapy usually includes PPIs, H2 receptor agonists, prokinetics, and cryoprotectants for the laryngeal mucosa. Empirical therapy with PPIs is justified because it can help in the diagnosis ex juvantibus (from the Latin ex - based on, juvanus - helping), i.e. treatment carried out in order to clarify the diagnosis. To date, studies of the effectiveness of PPIs in the treatment of LPR patients have produced a wide range of responses [21].
Studies evaluating the effectiveness of PPIs in LPR show results ranging from very good, with response rates reaching 70%, to no difference with placebo [22]. A controlled trial using lansoprazole 30 mg twice daily for three months in 22 patients with idiopathic chronic laryngitis found that 50% of patients in the treatment group had a complete response compared with 10% in the control group [23]. However, another study using lansoprazole at a similar dosage and regimen found no difference in response rates in patients with laryngopharyngitis [24]. A large multicenter study involving 145 patients with suspected LPR showed no benefit of esomeprazole 40 mg twice daily for four months compared with placebo [25]. One recent study of 85 patients with LPR found that PPI twice daily was more effective than once daily and that extending the course of treatment from two to four months resulted in more positive responses [26]. In general, for LPR, the use of a standard dose of PPI twice daily for two to three months is justified. Current recommendations do not suggest the use of H2-blockers in combination with PPIs in patients with suspected LPR [27, 28]. To achieve the best results, PPIs should be taken on an empty stomach 30 minutes before meals, with a course of treatment of 2–6 months until complete histological remission of laryngitis is achieved [29]. Patients whose quality of life and symptoms do not improve after two to three months of therapy most likely do not have GERD as a cause of LPR, but they should be evaluated for the presence of mixed reflux using manometry and pH monitoring [30]. If there is no effect from taking a PPI, a reassessment of symptoms with the participation of specialists from a pulmonologist and an allergist is necessary [31, 32].
The necessary comprehensive diagnosis and treatment of LPR was demonstrated by E. F. Kokorina, who assessed, in addition to endoscopic signs of esophagitis, the severity of chronic laryngitis in otorhinolaryngological manifestations of the extraesophageal form of GERD using the Williams scale, the level of dysphonia was assessed using the Consensus Auditory-Perceptual Evaluation of Voice (CAPE) scoring scale. V), proposed by the American Speech-Language Hearing Association, 2003. All patients underwent correction of GERD using PPI drugs; for the treatment of LPR in the main group of patients, the drug Erespal was added according to the standard regimen for 3 weeks. The duration of standard antireflux therapy was 3 months. Dynamic assessment of LPR was carried out several times up to 6 months after treatment; a statistically significant acceleration in the regression of reflux-induced changes in the larynx in patients of the main group was revealed [33]. I. L. Klyaritskaya, A. P. Balabantseva in their study showed that the use of double doses of PPI (pantoprazole) for 12 weeks leads to a significant reduction in symptoms of LPR compared to the control group. The optimal duration of treatment is 6–12 months, and after stopping the medication after 6 weeks it leads to an increase in scores on the Reflux Symptom Index questionnaire [34].
It is necessary to consider the use of prokinetics in the complex treatment of both GERD and LPR, which is a manifestation of GERD. Drugs such as metoclopramide, domperidone, cisapride and tegaserod have been used in patients with GERD in the past, but regular use of these drugs is not recommended by current standards due to limited indications and a high side effect profile [35]. In the treatment of GERD today, according to indications, the prokinetic agents itopride and mosapride are used; unfortunately, the latter is not registered in Russia. Itopride, registered in Russia since 2007, is used in patients with LPR as an adjuvant together with PPIs, as well as for other extraesophageal syndromes, accelerating the rate of reduction of symptoms [36, 37]. E. P. Oleinik et al. recommend the use of itopride, based on their own experience of using it in almost 1000 patients, in the complex treatment of all types of voice disorders due to GERD and LPR [38]. F.V. Semenov et al. A study involving 200 patients with LPR assessed the effectiveness of a two-week course of itopride in the treatment of otolaryngological manifestations of LPR. Its use led to a decrease in subjective complaints of patients and a weakening of the severity of laryngoscopic signs such as hyperemia and swelling of the mucous membrane of the arytenoid cartilages [39].
There are several scientific publications in the literature regarding rehabilitation speech therapy treatment of LPR with special voice exercises that strengthen the muscles of the larynx, and in some centers such therapy is carried out empirically without medical evidence-based support. A report on laryngeal rehabilitation in the treatment of chronic cough associated with GERD was recently published with significant improvement in symptoms [40].
The role of surgical fundoplication in patients refractory to even high (double) doses of PPI remains controversial. In a study by J. Swoger et al. evaluated symptoms in 10 PPI-resistant patients after fundoplication compared with 12 PPI-resistant patients who continued conservative treatment with double doses of PPI, showing that only 1 patient (10%) benefited from fundoplication, which was no different from the group comparison (7%) [41]. However, the role of surgery in PPI-resistant patients who have abnormal non-acid reflux remains important. They can be successfully treated with laparoscopic Nissen fundoplication [42]. Today, the Society of American Gastrointestinal and Endoscopic Surgeons clinical guidelines recommend antireflux surgery for patients who: have failed or are intolerant to medications; have significant extraesophageal manifestations such as aspiration, asthma, or cough; have ulcerative strictures as a complication of GERD [43].
Thus, there are no specific lesions of the larynx with laryngopharyngeal reflux, so the diagnosis of this pathology should be comprehensive and include both ENT and gastroenterological examination methods. Treatment of laryngopharyngeal reflux should also be comprehensive, from lifestyle modification and the use of local remedies to a long course of proton pump inhibitors and prokinetics in adequate dosage, and if they are ineffective, surgical treatment methods should be used.
Literature
- Vakil, N. van Zanden S.V., Kahrilas P. et al. The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensus // Am. J. Gastroenterol. 2006. Vol. 101. P. 1900–1920.
- Katz PO, Gerson LB, Vela MF Diagnosis and Management of Gastroesophageal Reflux Disease // Am J Gastroenterol. 2013. Vol. 108. R. 308–328.
- Lazebnik L. B., Bordin D. S., Masharova A. A. Modern understanding of gastroesophageal reflux disease: from Genval to Montreal // Experimental and clinical gastroenterology. 2007. No. 5. P. 4–10.
- Koufman JA, Aviv JE, Casiano RR, Shaw GY Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of OtolaryngologyHead and Neck Surgery // Otolaryngol Head Neck Surg. 2002. Vol. 127. R. 32–35.
- Ford CN Evaluation and management of laryngopharyngeal reflux // JAMA. 2005. Vol. 294. R. 1534–1540.
- Hicks DM, Ours TM, Abelson TI et al. The prevalence of hypopharynx findings associated with gastroesophageal reflux in normal volunteers // J Voice. 2002. Vol. 16. R. 564–579.
- Merati AL, Lim HJ, Ulualp SO, Toohill RJ Meta-analysis of upper probe measurements in normal subjects and patients with laryngopharyngeal reflux // Ann Otol Rhinol Laryngol. 2005. Vol. 114. R. 177–182.
- Aviv JE, Liu H, Parides M et al. Laryngopharyngeal sensory deficits in patients with laryngopharyngeal reflux and dysphagia // Ann Otol Rhinol Laryngol. 2000. Vol. 109. R. 1000–1006.
- Hanson DG, Jiang JJ Diagnosis and management of chronic laryngitis associated with reflux // Am J Med. 2000. Vol. 108. R. 112S–119S.
- Johnston N., Bulmer D., Gill GA et al. Cell biology of laryngeal epithelial defenses in health and disease: further studies // Ann Otol Rhinol Laryngol. 2003. Vol. 112. R. 481–491.
- Koufman JA The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury // Laryngoscope. 1991. Vol. 101. R. 1–78.
- Koufman JA, Amin MR, Panetti M. Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders // Otolaryngol Head Neck Surg. 2000. Vol. 123. R. 385–388.
- Belafsky PC, Postma GN, Koufman JA The validity and reliability of the reflux finding score (RFS) // Laryngoscope. 2001. Vol. 111. P. 1313–1317.
- Vaezi MF Sensitivity and specificity of reflux-attributed laryngeal lesions: experimental and clinical evidence // Am. J. Med. 2003. Vol. 115, (Suppl. 3 A). P. 97 S-104.
- Karkos PD, Yates PD, Carding PN, Wilson JA Is laryngopharyngeal reflux related to functional dysphonia? // Ann Otol Rhinol Laryngol. 2007. Vol. 116, No. 1. P. 24–29.
- Ahmed TF, Khandwala F, Abelson TI et al. Chronic laryngitis associated with gastroesophageal reflux: prospective assessment of differences in practice patterns between gastroenterologists and ENT physicians // Am J Gastroenterol. 2006. Vol. 101. R. 470–478.
- Williams RB, Szczesniak MM, Maklean HM et al. Predictors of Outcome in an Open Label, Therapeutic Trial of High-Dose Omeprazol in Laryngitis // Am J Gastroenterol. 2004. Vol. 42. R. 776–785.
- Vincent DA Jr., Garrett JD, Radionoff SL et al. The proximal probe in oesophageal pH monitoring: development of a normative database // J. Voice. 2000. Vol. 14. P. 247–254.
- Ayazi S., Lipham J., Hagen G. et al. A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold // J. Gastroenterol. Surg. 2009. Vol. 13 (8). P. 1422–1429.
- Steward DL, Wilson KM, Kelly DH et al. Proton pump inhibitor therapy for chronic laryngopharyngitis: a randomized placebo-control trial // Otolaryngol Head Neck Surg. 2004. Vol. 131. R. 342–350.
- Martinucci I., de Bortoli N., Savarino E. et al. Optimal treatment of laryngopharyngeal reflux disease // Ther Adv Chronic Dis. 2013. Nov. Vol. 4 (6). R. 287–301.
- Vaezi MF Extraesophageal manifestations of gastroesophageal reflux disease // Clin Cornerstone. 2003. Vol. 5. R. 32–38.
- El-Serag HB, Lee P, Buchner A et al. Lansoprazole treatment of patients with chronic idiopathic laryngitis: a placebo-controlled trial // Am J Gastroenterol. 2006. Vol. 96. R. 979–983.
- Havas T. et al. Posterior pharyngolaryngitis: double blind randomized placebo controlled trial of proton pump inhibitor therapy // Aust J Otolaryngol. 1999. Vol. 3. R. 243–246.
- Vaezi MF, Richter JE, Stasney CR et al. Treatment of chronic posterior laryngitis with esomeprazole // Laryngoscope. 2006. Vol. 116. R. 254–260.
- Park W., Hicks DM, Khandwala F. et al. Laryngopharyngeal reflux: prospective cohort study evaluating optimal dose of proton-pump inhibitor therapy and pretherapy predictors of response // Laryngoscope. 2005. Vol. 115. R. 1230–1238.
- Peghini PL, Katz PO, Castell DO Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects // Gastroenterology. 1998. Vol. 115. R. 1335–1339.
- Fackler WK, Ours TM, Vaezi MF, Richter JE Long-term effect of H2 RA therapy on nocturnal gastric acid breakthrough // Gastroenterology. 2002. Vol. 122. R. 625–632.
- Belafsky PC, Postma GN, Koufman JA Validity and reliability of the reflux symptom index (RSI) // J Voice. 2002. Vol. 16. R. 274–277.
- Yuksel ES, Vaezi MF Extraesophageal manifestations of gastroesophageal reflux disease: cough, asthma, laryngitis, chest pain // Swiss Med Wkly. 2012. Vol. 142. R. l35–44.
- Kahrilas P., Shaheen N., Vaezi M. et al. American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease // Gastroenterology. 2008. Vol. 135(4). R. 1383–1391, e1381–e1385.
- Zerbib F., Stoll D. Management of laryngopharyngeal reflux: an unmet medical need // Neurogastroenterol Moti. 2010. Vol. l22. R. 109–112.
- Kokorina V. E. Use of the drug erespal in schemes for the correction of reflux-induced laryngitis // Bulletin of Otorhinolaryngology. 2010. No. 6. pp. 61–63.
- Klyaritskaya I. L., Balabantseva A. P. Comparative effectiveness of high daily doses of proton pump inhibitors for laryngopharyngeal reflux // Ukrainian Therapeutic Journal. 2012. No. 1. pp. 21–27.
- Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease // American Journal of Gastroenterology. 2005. Vol. 100 (1). R. 190–200.
- Ezzat WF, Fawaz SA, Fathey H., El Demerdash A. Virtue of adding prokinetics to proton pump inhibitors in the treatment of laryngopharyngeal reflux disease: prospective study // Journal of Otolaryngology. 2011. Vol. 40 (4). 350–356.
- Chun BJ, Lee DS The effect of itopride combined with lansoprazole in patients with laryngopharyngeal reflux disease // European Archives of Oto-Rhino-Laryngology. 2013. Vol. 270(4). 1385–1390.
- Oleynik E. P., Kochesokova E. A., Ivanchenko G. F., Demchenko E. V. Treatment of patients with dysphonia with gastroesophageal reflux disease // Treating Physician. 2010. No. 9. pp. 7–10.
- Semenov F.V., Gorbonosov I.V., Vartanyan M.S. Experience with the use of itopride for the treatment of otorhinolaryngological manifestations of laryngopharyngeal reflux // Farmateka. 2011. No. 2. pp. 91–95.
- Pacheco A., Cobeta I., Wagner C. Refractory chronic cough: new perspectives in diagnosis and treatment // Arch Bronconeumo. 2013. Vol. l49. R. 151–157.
- Swoger J., Ponsky J., Hicks DM et al. Surgical fundoplication in laryngopharyngeal reflux unresponsive to aggressive acid suppression: a controlled study // Clin Gastroenterol Hepatol. 2006. Vol. 4. R. 433–441.
- Mainie I., Tutuian R., Agrawal A. et al. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication // Br J Surg. 2006. Vol. 93. R. 1483–1487.
- Zerbib F., Sifrim D., Tutuian R. et al. Modern medical and surgical management of difficult-to-treat GORD // United Eur Gastroenterol J. 2013. Vol. 1. R. 21–31.
E. Yu. Plotnikova*, 1, Doctor of Medical Sciences, Professor M. V. Krasnova**, Candidate of Medical Sciences K. A. Krasnov**, Candidate of Medical Sciences E. N. Baranova*
* State Budgetary Educational Institution of Higher Professional Education Kemerovo State Medical Academy of the Ministry of Health of the Russian Federation, Kemerovo ** Municipal Budgetary Healthcare Institution City Clinical Hospital No. 3 named after. M. A. Podgorbunsky, Kemerovo
1 Contact information
Abstract. Ethiopathogenetic mechanisms, clinical indicators and diagnostic methods of laryngopharyngital reflux. Modern treatment methods are described that presumably diet, changing of the mode of life, physical treatment methods and drug therapy as well as indications for surgery.
Treatment of yellow sputum when coughing
In the absence of elevated body temperature, outpatient treatment following the doctor’s instructions is sufficient. If the temperature rises above 38 degrees, bed rest or hospitalization is recommended, depending on the diagnosis. Complex therapy includes dietary nutrition with the exception of fried, salty, smoked foods, excessive consumption of sweets - junk food provokes the proliferation of pathogenic bacteria.
Preference is given to boiled and steamed foods; it is advisable to consume large amounts of fiber in the form of fruits and vegetables, and dairy products. Maintaining cleanliness in the living space, regularly ventilating the room, and quitting smoking during illness contributes to a speedy recovery.
Based on the individual characteristics of the patient and the complexity of the inflammatory process, it is recommended to take the following medications:
Expectorants - remove phlegm from the upper respiratory tract - Trypsin, Thermopsis, Sodium Benzoate; Bronchodilator medications - promote the release of sputum from the bronchi - Stoptussin, Erespal, Bromhexine, Gedelix; Broad-spectrum antibiotics - for the treatment of yellow sputum, it is important to choose the right antibacterial drugs in addition to symptomatic treatment; Inhalations - have an anti-inflammatory, antiseptic, expectorant effect - Berodual, saline solution; Antihistamines - if the cough is of allergic origin, antiallergic therapy is prescribed
Why choose Elena Malysheva Medical Center?
When choosing a doctor and a clinic for septoplasty, it is necessary to establish a trusting contact between the specialist and the patient. World-class doctors work at Elena Malysheva’s clinic. Dmitry Semenovich Gorin is a certified ENT doctor who has practiced in famous institutions in the USA (Ear, Nose and Throat Institute in New York) and Germany (University of ENT Diseases).
Dmitry Semenovich works with both adult patients and children. Having extensive practical experience behind him, Dr. Gorin performs ENT operations at the highest level. Thanks to the coordinated work of the entire medical center, preliminary diagnosis and basic treatment are carried out with a high degree of efficiency. The modern equipment used allows endoscopic septoplasty to be performed in a gentle manner, reducing the duration and intensity of rehabilitation.
Swelling after surgery persists for a week, and you can start working in 10-14 days.
Endoscopic septoplasty is a gentle surgical method that will solve your breathing problem. Elena Malysheva's clinic will free you from problems and allow you to freely take a deep breath through your nose!
More detailed information and registration by phone: 8.