Periodontal disease is a set of pathological processes that spread to the tissues surrounding the teeth and holding them in the alveoli. According to statistics, pathologies belonging to this group are diagnosed in 90% of the adult population. Moreover, most often diseases of this type are detected in men and women aged 37-45 years.
In the absence of timely and competent treatment, periodontal diseases can cause loosening and premature tooth loss, the appearance of foci of chronic infection in the oral cavity, deterioration of the body’s immune status and the development of other complications. That is why modern dentists pay increased attention to the development of methods and means for treating pathologies belonging to this group.
Structure and functions of periodontium
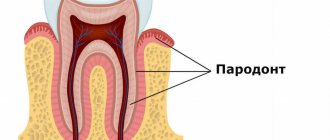
Periodontium is usually called a complex of tissues that includes:
- alveolar processes (areas of the jaw that bear the dentition);
- gums (mucous membranes covering the alveolar processes);
- periodontium (tissues consisting of protein fibers and located in the space between the alveolar plate and the cement of the tooth root);
- cement (special bone tissue covering the roots and necks of teeth).
In the human body, the periodontium performs the following functions:
- shock-absorbing (evenly distributes the load on the jaws);
- supporting-retaining (provides strong fixation of the tooth in the alveolar socket);
- trophic (contains an extensive network of lymphatic and blood vessels, a huge number of nerve receptors);
- barrier (protective) and others.
Preserving periodontal tissue in a healthy state is the key to long-term and proper functioning of the masticatory apparatus.
What are the differences between periodontitis and periodontal disease?
Patients often confuse these diseases. However, many doctors also do not consider periodontal disease as a separate dental problem, especially since it is excluded in the latest classification of diseases. But clinically the disease still exists and in its “pure” form occurs in no more than 3-5% of patients.
Periodontitis is a consequence of gingivitis, a slight inflammation of the gums. It most often occurs as a result of poor oral hygiene, that is, the accumulation of large amounts of plaque and tartar on the teeth/under the gums.
But the causes of periodontal disease have not been fully determined. On the one hand, it is caused by a general weakening of the body and disruption of metabolic processes, on the other hand, the disease develops as a consequence of long-term and complex treatment of periodontitis using conservative methods without the use of drugs aimed at tissue regeneration: constant curettage and trauma disrupt the nutrition of the gums and they are reduced in volume. Unlike periodontitis, with periodontal disease there are no voluminous periodontal pockets, but there may well be deposits on the necks and roots of the teeth, the gums do not bleed - on the contrary, they are pale and whitish. In the same way, exposure of tooth roots occurs, that is, a reduction in the volume of the mucous membrane - gum recession. And as a result, increased sensitivity occurs, increased susceptibility to thermal irritants and pressure due to the exposure of tooth roots, on which the enamel layer is practically absent. The more the disease progresses, the more pronounced the mobility of the teeth.
Causes of periodontal disease development
Factors that increase the likelihood of developing periodontal disease are:
- heredity;
- hypovitaminosis;
- failure to comply with hygiene requirements;
- presence of dental plaque;
- dental anomalies (bite disorders and others);
- somatic diseases (malfunctions of the nervous system, gastrointestinal diseases, diabetes mellitus, cardiac and endocrine disorders);
- smoking;
- weakened immune system;
- non-compliance with drinking regime;
- habit of breathing through the mouth;
- the presence in the oral cavity of low-quality fillings, orthodontic or orthopedic structures incorrectly installed in dentistry.
In addition, the risk of disease directly depends on the place of residence, lifestyle, characteristics of professional activity and dietary habits of patients.
What it is
Periodontium is periodontal tissue, the main function of which is to hold the tooth in the alveolus. All periodontal tissues are interconnected, so any changes in the functioning of one or another element inevitably affect the functioning of other elements. The periodontal structure includes periodontium, gums, alveolar processes and cementum. Some dental scientists also include tooth enamel, dentin and pulp in its composition.
The term “periodontium” appeared in dentistry a little over a hundred years ago and has since firmly taken its place in modern dentistry, although in Russia the term “took root” a little later, around the mid-30s of the last century. of periodontology deals with a thorough study of the periodontium, its main functions, structure, and possible diseases .
Symptoms of periodontal disease
The first symptoms indicating the occurrence of periodontal disease are:
- tingling, itching, numbness in the gums;
- bleeding of gum tissue;
- swelling of the interdental papillae;
- thickening of the gingival margin;
- detachment of gums from dental crowns.
In the future, the clinical picture may be supplemented by:
- gradual exposure of the necks of the teeth;
- redness, hyperemia of the gums;
- formation of pathological gum pockets;
- increase in interdental spaces;
- gradual loosening of teeth.
Symptoms of tissue diseases also include increased sensitivity of dental tissues to irritants, as well as aching pain in the affected area.
Classification and symptoms
Pathological damage to the tissues surrounding the dentition, in most cases, occurs as a result of an imbalance between bacterial symbiosis and oral tissues. There are 5 main categories:
- Gingivitis is an inflammation of the marginal part of the gum mucosa adjacent to the teeth, occurring without disturbing the position and mobility of the teeth. Accompanied by swelling, redness, pain and bleeding. The main cause is periodontal pathogens: Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and other gram-negative anaerobic coccobacilli. Under the influence of their toxins, a change in the structure of the tissues of the dental epithelial junction occurs, which serves as a barrier that prevents the penetration of infectious agents towards the tooth root. There are several forms: catarrhal (occurs in 97% of cases), hypertrophic, ulcerative-necrotic. The outcome of gingivitis can be complete restoration of periodontal tissue. Without adequate treatment, it turns into periodontitis and threatens adentia.
- Periodontitis is an inflammation of periodontal tissues, accompanied by progressive destruction of soft tissues and atrophy of the jaw bone. The causes are usually poor hygiene, mechanical injuries and hypersensitivity to certain medications. Risk factors include hormonal and general metabolic disorders, immunodeficiency states, malocclusions, hypertonicity of the masticatory muscles, etc. The disease develops gradually, and at the initial stage does not cause noticeable discomfort. Early manifestations may include bleeding, soreness and changes in the shape and color of the gums, and the appearance of bad breath. As the process progresses, periodontal pockets deepen, alveolar processes are destroyed, which leads to loosening and tooth loss. In severe cases of the disease, pus may be released from the periodontal pocket and an increase in body temperature may be noted.
- Periodontal disease is a dystrophic lesion of the periodontium, accompanied by gradual resorption of bone tissue. Periodontal disease is less common and, as a rule, is one of the symptoms of hypertension, atherosclerotic changes in blood vessels, neurogenic or endocrine pathologies. The difference between periodontitis and periodontal disease is that with periodontitis there is always an inflammatory process, while with periodontal disease it is absent. With periodontal disease, gum pockets do not form, there is no purulent discharge, and tooth displacement occurs only in severe forms of the disease when the root is more than half exposed. At the initial stage of the disease, there is usually no discomfort. Patients with moderate severity of periodontal disease experience burning, itching, and hyperesthesia. In severe cases of periodontal disease, due to loss of bone tissue, interdental spaces – trema – are formed between the teeth. A fan-shaped divergence of the crowns is observed.
- Idiopathic lesions. These include a number of general somatic diseases, one of the clinical manifestations of which is the progressive lysis of periodontal tissue (Papillon-Lefebvre, Hand-Schueller-Christian syndrome, neutropenia, immunodeficiency states, acatalasia, etc.). The causes of idiopathic periodontal pathologies are not completely clear. The leading role is played by genetic predisposition. Patients develop deep periodontal pockets with the release of exudate, displacement and loosening of dental units. Characterized by rapidly progressing resorption of bone tissue with the formation of oval-shaped cavities.
- Periodontomas are benign tumor and tumor-like pathologies of the periodontium: gingival fibromatosis, epulis, periodontal cyst, etc. They usually develop as a result of chronic irritation of soft tissues by destroyed tooth walls, sharp edges of deep-set crowns, and incorrectly modeled clasps of a removable denture.
Treatment of periodontal diseases
The general treatment program for periodontal diseases includes:
- removal of microbial plaque and mineralized deposits from the surface of teeth;
- caries therapy;
- preventing functional overload of certain areas of the dentition;
- rejection of bad habits;
- carrying out orthodontic treatment (if indicated);
- anti-inflammatory therapy;
- combating systemic diseases;
- the use of drugs that enhance immunity, stimulate osteogenesis and activate the adaptive and protective functions of the body;
- carrying out general hygiene measures (monitoring the regime of work, nutrition, rest, hygiene).
The treatment regimen for periodontal diseases is drawn up taking into account all manifestations of the disease and the results of a comprehensive examination of the patient. Timely seeking of professional help by a patient significantly improves the prognosis of the disease, shortens the duration of treatment and avoids the development of complications.
Therapy of periodontal pathologies
The treatment regimen is individual and depends on the characteristics of the clinical course and the severity of the pathology. As part of complex therapy, therapeutic, surgical, orthodontic and orthopedic treatment is usually carried out. Therapeutic treatment includes professional cleaning, treatment of gum pockets, anti-inflammatory and antimicrobial therapy. Surgical treatment includes various types of curettage, gingivectotomy, curettage of the pathological lesion with the introduction of osteogenic materials. Dental units with a high degree of mobility must be removed. Effective orthopedic methods for gum disease are splinting and selective grinding. Splints tighten movable dental units and fix them in the desired position, which avoids their premature loss. To improve blood supply and tissue regeneration, physiotherapeutic procedures are widely used - vacuum and hydrotherapy, electrophoresis.
One of the modern methods of periodontal treatment is the use of the Vector ultrasonic unit, designed to remove subgingival dental plaque and polish the root surface. The device is an innovative development of German scientists and is currently successfully used in many modern dental clinics. The operating principle is based on the use of ultrasonic waves. The destruction of the attachment of plaque and tartar to the root surface occurs due to the effect of ultrasonic cavitation. Ultrasonic waves are supplied with a special solution containing microparticles of calcium hydroxyapatite. This significantly improves the degree of teeth cleansing and reduces tissue sensitivity. The “Vector” device contactlessly removes dental plaque and at the same time has a positive effect on periodontal tissue: interstitial metabolism is restored, cells are saturated with nutrients, and tissue resistance to infectious and inflammatory processes increases. Treatment of periodontitis with the Vector device is relatively painless. As a rule, anesthesia is not required, but in case of increased sensitivity, patients can be given local anesthesia in the form of a gel that is applied to the gums. The effectiveness of treatment is evidenced by the regeneration of periodontal tissue and the achievement of a long-term state of remission.
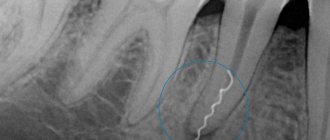
Differential diagnosis of diseases
The doctor makes a diagnosis based on the results of examining the patient's oral cavity using dental instruments, as well as on the results of an x-ray examination. It is also important to ask the patient in detail about the symptoms, their intensity, and nature. It is very important to conduct a detailed clinical examination of the patient to exclude the presence of other diseases.
Differential diagnosis of periodontal diseases is based on the analysis of radiographic data. With gingivitis, there are no changes in the bone base of the periodontium.
When diagnosing periodontal diseases, so-called indices are often used, which make it possible to determine the degree of the inflammatory process and changes in bone tissue, which allows for the most accurate diagnosis.