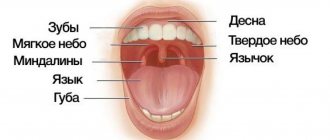
All tissues of the oral cavity, both teeth and gums, are interconnected and naturally have a complex structure. Gums, just like teeth, require careful and thorough care. Periodontology is a separate science in dentistry that deals with the study of gum disease. Inflammation from the teeth can spread to periodontal tissue, and vice versa. Therefore, it is so important to maintain careful hygiene of the entire oral cavity and promptly treat any dental diseases.
Gum structure
The periodontium consists of a complex of tissues that form the entire periodontal space.
- Periodontium is a complex of fibers that hold the dental unit in the socket. The periodontium is located between the cementum and the alveolar wall. Nerve fibers, lymphatic vessels, veins and arteries are also located here, which together are responsible for the proper metabolism of the tooth.
- The gums are the outer part of the entire complex. The gums are the first to bear the brunt of harmful microorganisms that enter the oral cavity.
- The alveolar process is a bone plate that has a spongy structure and serves as a bed for the dental unit.
- Cement is the outer covering and protection of the tooth root.
- Enamel covers the crown of the tooth and is the hardest element of the entire complex.
- The pulp is the main source of metabolism in the tooth. Consists of blood vessels and nerve endings.
- Dentin is a substance located around the pulp and consisting mainly of mineral components.
What it is
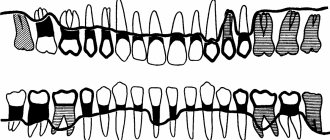
Periodontium is periodontal tissue, the main function of which is to hold the tooth in the alveolus. All periodontal tissues are interconnected, so any changes in the functioning of one or another element inevitably affect the functioning of other elements. The periodontal structure includes periodontium, gums, alveolar processes and cementum. Some dental scientists also include tooth enamel, dentin and pulp in its composition.
The term “periodontium” appeared in dentistry a little over a hundred years ago and has since firmly taken its place in modern dentistry, although in Russia the term “took root” a little later, around the mid-30s of the last century. of periodontology deals with a thorough study of the periodontium, its main functions, structure, and possible diseases .
Periodontal functions
In a healthy state, the periodontium performs a number of functions assigned to it:
- Support. The main function is due to which the tooth is held between bone plates.
- Shock-absorbing function. Correctly distributes pressure over the entire dentition.
- Trophic. A function responsible for nutrition and ensuring metabolism of the tissue complex.
- A protective function that helps create a barrier against the effects of bacteria.
- Reflex – affects the correct distribution of the chewing load.
- The plastic function is responsible for the elasticity of periodontal tissues.
Periodontium
Periodontium
(lat. Periodontium) - a complex of tissues located in the slit-like space between the cementum of the tooth root and the alveolar plate. Its average width is 0.20-0.25 mm. The narrowest section of the periodontium is located in the middle part of the tooth root, and in the apical and marginal sections its width is slightly greater.
The development of periodontal tissue is closely related to embryogenesis and teething. The process begins in parallel with the formation of the tooth root. The growth of periodontal fibers occurs both from the side of the root cement and from the side of the alveolar bone, towards each other. From the very beginning of their development, the fibers have an oblique course and are located at an angle to the tissues of the alveoli and cementum. The final development of the periodontal complex occurs after tooth eruption. At the same time, the periodontal tissues themselves are involved in this process. It should be noted that, despite the mesodermal origin of the constituent components of the periodontium, the ectodermal epithelial root sheath takes part in its normal formation.
The basis of the periodontium is connective tissue. Its main structure is collagen fibers. They form the basis of the periodontal ligament and connect the cement of the tooth with the bone tissue of the alveolus. Despite the lack of elasticity, collagen fibers provide some mobility of the tooth in the socket, mainly due to the slight tortuosity of their course. The sections of fibers that penetrate the cement and bone tissue of the alveoli are called perforating - Sharpey's fibers. The depth of their penetration into the cement is no more than 3-5 μ.t, and into the alveolar bone - up to 20 μ.t. In the periodontal gap, collagen bundles coming from the cement and alveoli form a pronounced intermediate plexus, which ensures the adaptation of the entire tissue complex to changing loads on the tooth. The collagen that is part of the periodontal ligament is typical in its physicobiochemical properties, but its fibrils have a relatively small diameter - no more than 55 μ.t. In addition to the typical collagen fibers in the periodontium, there are immature - elastic - oxytalan fibers. They reach a length of several millimeters and run parallel to the cementum of the tooth root, crossing the collagen bundles at right angles. These fibers are credited with a significant role in the process of regulation and distribution of blood flow during physical stress on the periodontium.
Periodontal diseases
Reasons why gum disease occurs:
- soft and hard plaque on teeth;
- anomalies in the location of dental units;
- poor-quality prosthetics or treatment;
- genetic predisposition;
- reduced immunity;
- diseases of internal organs;
- hormonal imbalances in the body;
- constant stress;
- various bad habits;
- Irregular oral care.
In contrast to the large number of causes influencing the development of periodontal diseases, there are not so many diseases themselves:
- Gingivitis is the initial stage of gum inflammation.
- Periodontitis is an inflammatory process in the gums, gradually spreading to the alveolar processes of the jaw.
- Periodontal disease is a fairly severe form of the disease, characterized by exposure of the roots of the teeth.
- Periodontoma is the formation of tumors in soft tissues.
Gingivitis
Acute catarrhal gingivitis is an inflammatory process with a predominance of exudation. This disease is characterized by complaints of pain, itching, bleeding gums, and refusal to eat. Upon examination, hyperemia and swelling of the papillae, gingival margin, and sometimes the alveolar gum are determined, which leads to an increase in size and a change in the shape of the gingival papillae (not sharp, but rounded). When the alveolar gum is involved, its granularity (symptom of lemon peel), characteristic of healthy gums, disappears. Bleeding gums are detected when you touch them slightly. This form of gingivitis is observed relatively rarely, mainly during teething, as a result of acute trauma (mechanical, chemical, thermal), in acute childhood infectious diseases, and also as a manifestation of allergies, a symptom of acute herpetic stomatitis.
Chronic catarrhal gingivitis is the most common periodontal pathology in children. There may be no complaints; sometimes children notice bleeding gums when brushing their teeth. Upon examination, congestive hyperemia, pastosity, bleeding of the papillae and gingival margin are determined. The marginal gum is thickened like a roller (stretches like a rubber balloon), the surface becomes shiny. The granularity of the alveolar gum disappears.
With catarrhal gingivitis (both acute and chronic), with significant swelling of the gums, a gingival pocket, that is, a false periodontal pocket, can occur. The radiograph shows no changes in the alveolar bone.
Hypertrophic gingivitis is a chronic inflammatory process characterized by an increase in gingival papillae and marginal gums due to the proliferation of fibrous connective tissue and the basal layer of the epithelium. Most often, hypertrophic gingivitis is observed with close position of the teeth, open bite, small vestibule of the oral cavity, short frenulum of the lips, with improper orthodontic treatment, as well as during puberty (in girls with a late onset of menstruation or a long menstrual cycle, when the effect of estrogens predominates) , when taking antiepileptic drugs and blood diseases.
Hypertrophic gingivitis, caused by local factors (crowding of teeth, dental anomalies), is limited in nature, located mainly in the frontal area. Hypertrophic gingivitis, caused by endogenous causes (endocrine pathology, gastrointestinal diseases, etc.), is generalized, characterized by rapid development, a tendency to relapse and resistance to local treatment.
There are inflammatory (granulating) and fibrous forms of hypertrophic gingivitis. The inflammatory form is characterized by: hyperplasia of the gingival papillae, which are covered with granulations; their hyperemia with pronounced cyanosis and swelling; loose tissue and severe bleeding; pain on palpation; thickening of the gingival margin, its separation from the necks of the teeth, chronic catarrhal inflammation of the alveolar gum. False periodontal pockets are identified due to swelling and hyperplasia of the gums. There is a deposition of plaque and tartar. Hypertrophied marginal gum covers one or another part of the tooth crowns.
In the fibrous form, the gingival papillae are enlarged, dense, pale, do not bleed, and are painless.
According to the intensity of productive inflammation, there are 3 degrees of hypertrophic gingivitis:
— 1st degree — hypertrophy of gingival papillae;
— 2nd degree — hypertrophy of the gingival papillae and marginal gums;
— 3rd degree — hypertrophy of the marginal and alveolar gums.
Desquamative gingivitis is clinically characterized by swelling of the marginal gum, sometimes extending to the attached gum, pronounced hyperemia, severe bleeding and pain. A feature of this form of gingivitis is the constant desquamation of the surface layers of the gum epithelium, not only marginal, but also alveolar, as a result of which almost the entire mucous membrane becomes eroded and easily vulnerable. May occur against the background of hypertrophic gingivitis. Children complain of pain when brushing their teeth and eating, the presence of blood in saliva, the specific smell and taste of blood.
Desquamative gingivitis in children develops rarely, mainly during puberty (in girls, usually during a short menstrual cycle, when the action of progesterone predominates).
Treatment
Treatment of major periodontal diseases is as follows:
- removing all plaque and then polishing the teeth;
- treatment of existing carious formations;
- carrying out high-quality prosthetics, if necessary;
- splinting of the dentition (also carried out if necessary);
- treatment of existing common diseases;
- taking vitamins or medications;
- Regular cleaning of the oral cavity not only at home, but also in the dental office.
In the most difficult situations, in addition to the listed treatment, surgical intervention may be necessary.
Vector device in periodontology
The Vector device allows you to quickly and reliably cure patients of many symptoms. It not only helps to get rid of the disease, but also activates the reserve forces of the periodontium, which allows you to avoid many problems in the future. With the invention of the Vector device, periodontics has reached a qualitatively new level of disease treatment. Literally in one visit to the doctor you can get rid of such unpleasant symptoms as bleeding gums, inflammation and soreness of the gums. Moreover, the treatment is almost painless.
The Vector periodontal device was invented in Germany and is most often used to remove dental plaque, which is the main cause of periodontal disease. Using the device, you can also treat the surface of the teeth with ultrasound before fixing the dentures. However, its main purpose is the treatment of periodontal diseases.
If you have suffered greatly from an inflammatory disease, Vector will help replace curettage, which is why the device is often used for osteoplasty and gingivoplasty.