Periodontal disease is a fairly rare disease of non-inflammatory origin, characterized by systemic damage to the periodontal tissues (periodontium), which is often difficult to diagnose in the early stages. Its appearance, as a rule, is associated with a hereditary predisposition or systemic diseases of certain organs.
There is often an erroneous spelling of this term - periodontal disease. In order to dispel all doubts, let us turn to the etymology, which covers two words in ancient Greek: πᾰρά (para - “near, located near”) and ὀδόντος (odóntos is the genitive case of the word ὀδούς - odus, translated means “tooth”).
Consequently, from the ancient Greek language this term is translated as “near the tooth” or “located next to the tooth.”
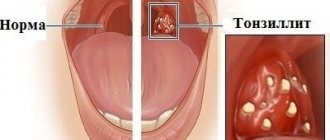
There are cases when even doctors mistakenly call periodontal disease a completely different disease - periodontitis, which is in fact a completely different phenomenon due not only to its inflammatory origin, but also to other features.
Diagnosis of periodontal disease
To identify signs of periodontal disease in adults, the following diagnostic procedures are usually performed:
- inspection;
- probing of the gingival sulcus;
- assessment of tooth mobility;
- X-ray examination (orthopantomography);
- biomicroscopy of the gums to determine the degree of microcirculation impairment.
The patient will also need observation from a general practitioner and endocrinologist to detect and treat general somatic pathology.
After a diagnosis of “dental disease periodontal disease” is made, further examination should be aimed at finding the causes of disturbances in the processes of cellular tissue nutrition, predicting the further development of the disease and the likelihood of inflammatory complications.
Symptoms of dental periodontal disease
The main symptom of the disease is detected during x-ray diagnosis of periodontal disease. The image shows a uniform decrease in the height of the interdental septa with alternating foci of osteosclerosis and osteoporosis in the deep parts of the alveolar process and the body of the jaw, as well as in other bones of the skeleton. Traditionally, changes are accompanied by the presence of diseases of the cardiovascular or endocrine systems and metabolic disorders.
There are other symptoms of severe periodontal disease that are more noticeable to the patient and others:
- gum retraction;
- exposure of the necks and roots of the teeth;
- pale gum color;
- lesions of teeth of non-carious origin (wedge-shaped defects, hyperesthesia).
Stages of periodontal disease
In modern dentistry, there are three degrees of severity of periodontal disease.
Mild degree
How does periodontal disease begin? In the early stages, the disease occurs without pronounced symptoms with gradual atrophy of the gum edge and bone tissue. With periodontal disease of the anterior teeth, a slight exposure of the dental necks occurs; in some cases, patients experience increased sensitivity of teeth to food irritants (hot and cold, sweet and sour). On X-ray images, the onset of periodontal disease is indicated by the first signs of bone tissue atrophy.
Average degree
With an exacerbation of periodontal disease, not only the necks, but also the roots of the teeth are exposed - by 2 - 3 millimeters. X-ray images show destruction of bone tissue along half the length of the root and the presence of foci of sclerosis.
Severe degree
With severe periodontal disease, exposure of the roots of the teeth reaches 4–5 millimeters, bone tissue atrophy on X-ray photographs covers two-thirds of the root.
Periodontal disease – what to do?
At the initial stage of periodontal disease, you should consult a periodontist. No folk remedies will help get rid of the disease. Only a specialist will be able to carry out the necessary diagnostic procedures and prescribe, based on the identified symptoms of periodontal disease, treatment aimed at slowing down degeneration in periodontal tissues and preventing inflammatory complications. It is also necessary to eliminate non-carious dental lesions and undergo a thorough examination by a therapist to diagnose and treat common diseases that provoke the development of periodontal disease.
Complex therapy of periodontal disease involves the following measures:
- Timely removal of dental plaque.
- Normalization of occlusal relationships (grinding teeth, prosthetics, splinting).
- The use of vitamins and agents that improve microcirculation (nicotinic acid, aloe extract, heparin).
Prevention of periodontal disease and periodontitis
Preventive measures include the following:
- periodic professional cleaning of tooth enamel from plaque and tartar;
- ensuring the body receives essential vitamins and minerals, in particular calcium and vitamin D3;
- routine visits to the dentist for oral hygiene;
- eradication of bad habits;
- from early childhood, taking care of enamel and the formation of a correct bite;
- include solid, healthy foods in your diet - raw carrots, apples, which improve blood circulation and strengthen gums;
- learn oral care skills.
The answer to the question of whether it is possible to become infected with periodontal disease is negative. However, there is always a risk of developing periodontitis, gingivitis and stomatitis.
Bibliography
- Barer G.M. – Periodontal diseases. Textbook, M.: GEOTAR-Media, 2008.
- Borovsky E.V. – Therapeutic dentistry. Textbook, MIA 2003.
- Dmitrieva L.A. — Modern aspects of clinical periodontology, M., 2001.
- Loginova N.K., Volozhin A.I. — Pathophysiology of periodontal disease (methodological manual), M., Medicine, 1993.
- Tsepov L.M., Kamanin E.I., Morozov V.G. — Periodontitis: intercellular, intertissue, intersystem interactions and clinical relationships, Smolensk, 1992.
- Gaurav, Solanki and Renu Solanki - Dental Plaque Forming Bacteria's Characterization and Stress Responses - M.: LAP Lambert Academic Publishing, 2012.
- Ijndhe J. - Textbook of Clinical Periodontology. 1995. Copenhagen.
- Kuzmina E.M. – Prevention of dental diseases, M.: 2003.
- Grudyanov A.I. — Antimicrobial and anti-inflammatory therapy in periodontology, M., 2004.
Find a clinic
Treatment methods
Methods and procedures used to treat periodontal disease in dentistry:
- exposure to high pressure oxygen in hyperbaric chambers;
- electrophoresis;
- diadynamic currents;
- amplipulse therapy;
- darsonvalization of gums;
- UHF therapy;
- gum massage;
- local hypo- and hyperthermia;
- ultrasound therapy.
Psychosomatics of periodontal disease
Based on the results of many years of research, American scientists have come to the conclusion that dental diseases such as periodontal disease are directly related to high anxiety, depression and an acute sense of loneliness. This is explained by the fact that increased levels of the stress hormone - cortisol - in the blood negatively affect the condition of the gums and jaw bones. In addition, during periods of nervous tension, people begin to pay less attention to oral hygiene and increase the doses of alcoholic beverages, nicotine and medications, which also contributes to the development of various diseases.
Treatment with antibiotics, dental ointments and gels
Drug therapy is possible after professional teeth cleaning as prescribed by a doctor. Antibiotics should be taken in recommended doses in the absence of inflammatory processes in the oral cavity.
In some cases, during treatment, injections are prescribed simultaneously with the drugs Traumeel and Lincomycin.
To relieve symptoms, the dentist prescribes gels and ointments:
- "Metrogil Denta" is an anti-inflammatory, analgesic agent;
- "Cholisal" - a gel to combat gum inflammation;
- "Kamistad" - for the prevention of gingivitis, relieving swelling, eliminating pain;
- “Gengigel” is a gel that increases blood circulation and promotes the regeneration of soft tissues;
- "Stomatofit" - to relieve severe pain;
- "Asepta" - to stimulate tissue regeneration processes;
- "Solcoseryl" is an antiseptic with a healing effect.
Consequences of periodontal disease - why is it dangerous?
- Firstly, due to the absence of pronounced symptoms, this disease can progress unnoticed over many years and lead to total destruction of the teeth and jawbone - and then teeth fall out with periodontal disease.
- Secondly, the destruction of bone tissue leads to disturbances in the functioning of the gastrointestinal tract with the subsequent occurrence of diseases of the digestive system.
- Thirdly, advanced periodontal disease can provoke periodontitis - acute inflammation of the tissue and tooth loss.
In addition to the above consequences, generalized periodontal disease in an advanced stage causes another dangerous disease - osteomyelitis, that is, purulent bone damage.
Misconception or fact
Many people have heard that periodontal disease is contagious. Usually, the person who claims this says that he or someone he knows contracted this disease from other people.
Are these opinions a misconception or a fact? Is periodontal disease contagious or not, is it transmitted by airborne droplets, contact, fecal-oral, vector-borne (through the bites of blood-sucking insects) or other known routes of oral infection transmission? The essence and causes of the origin of this disease will help us answer these questions.
The origin of the disease is not influenced by microorganisms
Oral thrush, one of the most common forms of thrush, is a fungal infection caused by the yeast Candida that affects the mucous membranes of the mouth.
Candida is a genus of yeast. There are about 150 different species of Candida that can cause serious yeast infections. The most common cause of thrush is Candida albicans.
Typically, infectious fungi are a natural component of the skin, oral cavity, and intestinal flora. They do not cause discomfort as long as their reproduction is limited by the balance of other microorganisms and the immune system. Problems only arise when fungi overgrow or break through the natural barriers of the skin and mucous membranes, causing thrush.
Candidiasis is the common term for infections caused by this fungus. Therefore, oral thrush is called oral candidiasis or candidal stomatitis. Fungal infections traditionally occur in the mouth and areas close to the throat. Children are more often susceptible to the disease, but the infection can also occur in adults with weak immune systems.
Forms of candidiasis in the mouth
Typically, mouth fungus develops on the inside of the cheeks or lips. But the throat, tongue or palate may also be affected.
Thrush can change from one form to another, or occur independently.
Types of thrush in the mouth and their signs:
- pseudomembranous candidiasis: white, cheesy, easily removable plaque on the reddened, inflamed mucous membrane
- acute erythematous candidiasis: burning sensation on the tongue, severe redness of the mucous membrane without deposits
- hyperplastic candidiasis: dense gray-white plaque, the oral mucosa is hyperemic
Pseudomembranous candidiasis in the mouth
- classic thrush. In the most common form of oral thrush, pseudomembranous candidiasis, isolated white speckles form in the mouth and are easily removed.
After scraping, the oral mucosa appears shiny, dry and red. As a fungal infection progresses, increasingly large white creamy spots appear, which, when detached, lead to bleeding of the mucous membrane. If left untreated, thrush in the mouth can spread to the throat, esophagus, or gastrointestinal tract.
Other symptoms of oral thrush
In addition to the described plaque and redness of the mucous membrane, late-stage oral thrush causes additional symptoms. These include:
- burning and dry mouth
- increased thirst
- bad breath
- metallic taste in mouth
- swollen lymph nodes
- difficulty swallowing
- pain while eating or drinking
- thrush in the mouth in children is in most cases accompanied by fever
Periodontal disease - contagious or not?
To the questions “Is periodontal disease contagious?” or “Is periodontal disease transmitted by airborne droplets?” Doctors answer unequivocally in the negative. Therefore, you should not believe various dubious articles on the Internet about how periodontal disease is transmitted. The disease is associated with metabolic disorders, and not with the spread of bacteria. Therefore, those who believe that periodontal disease can be contracted or that the disease is transmitted through a kiss are deeply mistaken. However, despite this, we must not forget about the rules of daily oral hygiene in order to prevent the occurrence of other problems with teeth and gums.
What is periodontitis? Causes and symptoms
With contagious periodontitis, the periodontal structures become inflamed, the periodontal junction is destroyed, and periodontal pockets are formed. Pathogenic bacteria accumulate in them.
The reasons for the development of an infectious condition are the accumulation of dental plaque, contagious gingivitis, and improper or insufficient oral hygiene. The contagious disease itself is infectious in nature.
Symptoms of periodontitis:
- redness and bleeding of the gums;
- bad breath;
- exposure of the necks of the teeth;
- loose teeth.
Is the disease contagious? Is periodontitis transmitted through kissing?
Periodontitis is infectious in nature because it is caused by pathogenic microorganisms. May accompany periodontal disease.
When kissing, the pathogen is transmitted, and there is a risk of infection and the development of periodontitis.