Gums and teeth
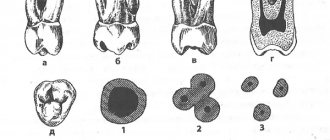
Everyone knows that teeth are the main characters in the process of chewing and grinding food. According to their roles, teeth in a person’s mouth are divided into types:
- Incisors – the front 4 teeth, play the role of biting off the largest pieces.
- Fangs - their role is to break food and separate it into pieces; they are also called “eye teeth”.
- Small and large molars play the role of chewing and grinding food.
People eat food of different origins, both plant and animal. On this basis, it was concluded that people are omnivorous creatures.
This is possible due to the arrangement of the teeth and the structure of the oral cavity, which makes humans fundamentally different from animals.
All teeth have the same structure: a soft core, dentin. The core consists of blood vessels and nerves, and the hard substance (bone) is dentin. The main function of this substance is to protect teeth from microdamage. To do this, it is “painted” with enamel, which feels absolutely nothing. In addition, enamel has no equal in strength in the human body. It consists of an alloy of minerals (phosphorus and calcium salts) saturated with organic substances. The highest concentration of calcium is observed in dentin, where nerve fibers are contained.
Text of the book “Topographic anatomy and operative surgery for dentists”
Mucous membrane
The soft palate is innervated by the lesser palatine nerve (n. palatinini minores).
Submucosal layer
thin.
The muscular basis of the soft palate is:
• uvula muscle (m. uvulae);
• palatoglossus muscle (m. palatoglossus);
• velopharyngeal muscle (m. palatopharyngeus);
• muscle that lifts the velum palatine (m. levator veli palatinae).
The soft palate is supplied with blood by the small palatine artery, which runs from the greater palatine canal posteriorly. Additionally, vessels from the ascending palatine artery (a. palatinae ascendes), which is a branch of the facial artery, approach the soft palate.
The ascending pharyngeal artery (a. pharyngea ascendens), which extends from the external carotid artery, also participates in the blood supply to the soft palate.
Floor of the mouth
Stratigraphy
Layers of the floor of the mouth:
• mucous membrane;
• lingual glands with adjacent vessels, nerves and layers of fiber;
• muscles of the oral diaphragm (Fig. 137).
Rice. 137. Contours of the mucous membrane of the floor of the mouth and tongue (after: Zolotko Yu. L., 1964). 1 – apex linguae; 2 – facies inferior; 3 – v. lingualis; 4 – frenulum linguae; 5 – plica sublingualis; 6 – tunica mucosa oris; 7 – caruncula sublingualis; 8 – gingiva; 9 – vestibulum oris; 10 – frenulum labii inferioris; 11 – dentes incisivi; 12 – dens caninus; 13 – dentes premolares; 14 – cavum oris proprium; 15 – dentes molares; 16 – dens serotinus.
Under the mucous membrane
in the fiber on the mylohyoid muscle (mm. mylohyoideus) there are lingual glands.
The following elements are adjacent to them:
• outside – lower jaw with m. mylohyoideus;
• on the medial side – mm. genioglossus et mylohyoideus;
• posteriorly – submandibular gland;
• the submandibular duct passes along the medial edge of the sublingual gland complex;
• in turn, the lingual artery passes medially and posterior to the duct;
• the lingual nerve approaches the excretory duct, located further in the sublingual tissue before immersing into the thickness of the organ.
The floor of the mouth is formed by the following muscles:
• mylohyoid muscles (mm. mylohyoidea), which make up the diaphragm of the mouth. The mylohyoid muscles, moving from the hyoid bone to the mylohyoid line of the body of the lower jaw and intertwining with each other, form a median suture along the midline. Between the bundles of mylohyoid muscles there are gaps in which anastomoses are located between the mental and lingual arteries. In addition, through these gaps, inflammatory processes can spread from the sublingual tissue into the submandibular region and retention cysts of the sublingual gland (“diving” cysts) can move;
•mm. geniohyoidei (geniohyoid muscles), adjacent to the mylohyoid muscles on the side of the mouth;
•mm. genioglossi, located above mm. geniohyoidei;
•mm. digastrici, approaching the mylohyoid muscles from the side of the neck.
Cellular spaces above the oral diaphragm
1. Two lateral spaces, which are the bed for the lingual glands, are limited:
• above – the oral mucosa between the tongue and gums;
• below – m. mylohyoideus;
• inside – by the muscles of the tongue;
• externally – by the lower jaw.
2. Paired intermuscular gaps are located between m. genioglossus and m. geniohyoideus.
3. The unpaired space is located between the genioglossus muscles.
With phlegmon of the floor of the mouth, the spread of the purulent process is most likely in the following directions:
1) in the peripharyngeal space - mediastinum;
2) into the retromaxillary space;
3) in the sheath of the neurovascular bundle of the medial triangle of the neck - the mediastinum.
Language
The tongue has two sections, delimited by a V-shaped shaft:
1. Anterior (apex and body), located in the oral cavity.
2. Posterior (root), located in the pharynx area.
Relief
The mucous membrane of the upper surface of the tongue at the root, moving to the epiglottis, forms three folds:
• middle lingual-laryngeal (median);
• two lateral lingual-laryngeal (borderline).
Between these folds a depression is formed in which foreign bodies are usually retained.
The mucous membrane of the lower surface of the tongue is clearly visible when the mouth is open and the tip of the tongue is raised. Fringed folds of the mucous membrane (plica fimbriata) diverge at an acute angle from the midline.
Along the folds, the ducts of the anterior glands of the tongue open. With the tongue raised and retracted posteriorly along the midline, the sublingual fold (frenulum) - frenulum lingua, stretched between the tongue and the lower jaw, is also clearly visible.
• The frenulum must be cut to restore full tongue movement.
From the sides of the midline, along the lower surface of the tongue, a neurovascular bundle stretches (v. lingualis, n, lingualis, a. profunda lingue, and behind also n. hipoglossus) (Fig. 138).
Rice. 138. Muscles, vessels and nerves of the tongue, floor of the mouth and lower lip (after: Zolotko Yu.L., 1964). 1 – v. lingualis; 2 – fiber located between the genioglossus muscles, – 3 – m. longitudinalis inferior, 4 – m. genioglossus, 5 – n. lingualis,6 – v. lingualis,7 – ductus submandibularis,8 – ductus sublinguales minores,9 – glandula sublingualis,10 – n. mentalis(rami labiales inferiores),11 – a. labialis inferior,12 – glandulae labiales,13 – m. orbicularis oris,14 – m. mentalis,15 – m. buccinator, 16 – v. facialis.
Stratigraphy
The tongue has two layers:
• mucous membrane;
• muscles.
The intrinsic muscles of the tongue, located in layers within the organ in the direction from top to bottom, include:
• the superior longitudinal muscle (m. longitudinalis superior) shortens the tongue;
• the lower longitudinal muscle (m. longitudinalis inferior) shortens the tongue;
• transverse muscle (m. transversus linguae) reduces the diameter of the tongue;
• the vertical muscle of the tongue (m. verticalis linguae) flattens the tongue.
Additional muscles of the tongue include:
• hyoglossus muscle (m. hyoglossus), which has an attachment point outside the tongue on the greater horn and body of the hyoid bone. When this muscle contracts, the tongue lengthens, as well as it moves backwards and downwards;
• the genioglossus muscle (m. genioglossus) outside the tongue fans out from the chin. When the muscle contracts, the tongue flattens and moves anteriorly;
• styloglossus muscle (m. styloglossus) is directed to the tongue from the styloid process (retracts the tongue posteriorly and upward).
Damage to the tongue is accompanied by severe bleeding and deformation of the organ.
Suturing a tongue wound
Conditions for suturing a tongue wound:
1. Gentle treatment of the wound edges.
• Incised wounds of the tongue can be sutured without excision of their edges.
2. No bleeding (if it is impossible to stop bleeding in the wound, ligation of the lingual or external carotid artery should be performed without delay).
3. Separate suturing of the tongue wound and the defect of the mucous membrane of the floor of the mouth to prevent the development of a single rough scar.
4. Use of absorbable suture material.
5. Use of round needles.
Requirements for sutures on a tongue wound:
1. Ensuring longitudinal orientation of the wound. Applying sutures to a wound of the tongue oriented in the transverse direction will lead to the development of permanent deformation and disruption of the function of this organ.
2. Strict adaptation of the entire thickness of the wound edges.
3. Reliable hemostasis.
4. A small “step” of the seam (up to 1–1.5 cm) (Fig. 139).
Rice. 139. Suturing a tongue wound: 1 – correct orientation of the tongue wound during suturing; 2 – incorrect orientation of the tongue wound during suturing (according to: Semenov G.M., Petrishin V.L., Kovshova M.V., 2001).
Zev
The pharynx is limited by the following elements:
• palatine arches – palatoglossus and velopharyngeal (arcus palatoglossus et palatopharyngeus);
• soft palate;
• root of the tongue.
The basis of the palatoglossus and velopharyngeal arches, which determines the shape and degree of severity, are muscles. In the palatoglossal arch there passes m. palatoglossus, in the velopharyngeal arch – m. palatopharyngeus. Between the arches, tonsil dimples are formed containing the palatine tonsils.
The bottom of this niche (m. constrictor pharyngeus superior, covered with pharyngeal fascia) is also the lateral wall of the pharynx.
The inner surface of the tonsils faces the pharynx and is accessible for inspection, and the outer surface is fixed by connective tissue bridges to the bottom of the niche.
During all manipulations near the tonsils, it should be remembered that their lower pole is 1–1.7 cm from the internal carotid artery (Fig. 140).
Rice. 140. Pharynx: 1 – palatoglossal arch; 2 – velopharyngeal arch; 3 – palatine tonsil (according to: Frauchi V. X. 1967).
Outer wall of the mouth
The mucous membrane of the vestibule of the oral cavity is adjacent to the buccal muscle. On the mucous membrane opposite the 1–2 upper molars there is a small elevation corresponding to the mouth of the parotid gland duct.
The concept of radical uranoplasty according to Limberg
Purpose of the operation:
1. Elimination of the cleft of the hard palate to separate the oral cavity from the nasal cavity.
2. Narrowing of the middle section of the pharyngeal ring for the normal functioning of the soft palate (speech development).
The operation consists of three main stages:
1. Retrotransposition (posterior displacement of mucoperiosteal flaps of the hard palate).
Sequencing:
• along the edges of the defect, a strip of the mucous membrane of the hard palate 3–4 mm wide is excised to the anterior edge of the defect;
• from the level of the distal edge of the first or second molar on the right and left sides, incisions are made in the mucous membrane and periosteum along the inner surface of the alveolar process of the upper jaw, at a distance of 2–3 mm from the gingival margin. The incisions end at the level of the canine socket or lateral incisor;
• in front, a medial incision is connected, refreshing the edges of the cleft, and lateral incisions along the gingival margin with oblique incisions located along the edges of the incisive foramen;
• using a Farabeuf rasp (straight and curved), tongue-shaped mucoperiosteal flaps are carefully peeled off from front to back to the level of the posterior edge of the hard palate and the anterior edges of the greater palatine foramina;
• install the blade of a narrow chisel or osteotome on the medial side of the neurovascular bundles emerging from the greater palatine canals, and perform resection of the posteromedial edge of the greater palatine foramina. The transformation of the large palatine foramina into half rings promotes the displacement of mucoperiosteal flaps of the hard palate posteriorly and medially due to the mobilization of neurovascular bundles, lowering the soft palate and narrowing the entrance to the pharynx.
2. Mesopharyngoconstriction (narrowing of the middle part of the pharyngeal ring).
To narrow the oropharynx, perform the following steps:
• lateral incisions of the mucous membrane and periosteum of the hard palate continue posteriorly to the last tooth;
• the tissue of the peripharyngeal space is pushed apart in a blunt manner until the anterior internal edge of the medial pterygoid muscle is visualized;
• shift the lateral walls medially on both sides.
To reduce the tension of the muscles of the soft palate, starting from the inner plate of the pterygoid process (mm. tensor veli palatini, constrictor pharyngeu superior), an interlaminar osteotomy is performed:
1. A chisel or osteotome is inserted into the oral cavity in the transverse direction. The blade of a narrow straight chisel or osteotome is placed directly outside the greater palatine foramen, and its handle is placed above the small molars of the opposite side.
2. Using weak hammer blows, a notch is made in the cortical plate of the inner surface of the alveolar process.
3. Pressing the chisel blade directly into the bone, move its handle in the medial direction, placing it above the central incisors. Having felt the hook of the pterygoid process (hamulus pterygoideus) through the soft tissue, direct the chisel blade outward from it through the pterygoid notch in the direction of the pterygoid fossa. Inserting a wide straight rasp into the resulting gap instead of a chisel, using lever-like movements, successively break the inner plate of the pterygoid process on one side and the other. By moving the attachment points mm. tensor veli palatini et constrictor pharyngeu superior in the medial direction the entrance to the pharynx narrows.
4. Fissurorrhaphy (closure of the hard palate defect by suturing the medial edges of the mucoperiosteal flaps).
1) Using thin absorbable material, sutures are placed on the soft palate.
2) The medial edges of the mucoperiosteal flaps of the hard palate are connected along the midline with interrupted or U-shaped sutures using absorbable material.
Until complete healing and epithelization of the central and lateral wounds, the surface of the hard palate is covered with a protective plate (Fig. 141).
Rice. 141. The main stages of radical uranoplasty: 1 – refreshing the edges of the wound; 2 – interlaminar osteotomy; 3 – fissurorrhaphy (according to: Frauchi V. X., 1967).
Opening of phlegmon of the floor of the mouth
Drainage of the cellular space between mm. genioglossus and hyoglossus and the lower jaw, reaching above the mucous membrane, and below to m. mylohyoideus, can be performed intraorally:
• dissection of the mucous membrane is carried out within the anterior teeth near the surface of the lower jaw, avoiding damage to the hypoglossal nerve and lingual vessels;
• penetrate under the mucous membrane using a blunt method.
Opening of abscesses and phlegmons of the tongue
Superficial abscesses of the tongue are opened with small longitudinal incisions on the dorsal or lateral surface, depending on the location.
Opening of an abscess of the hard palate
To avoid damage to the greater palatine artery and incisive artery, the mucosal incision is made near the alveolar edge, followed by peeling of the mucous membrane.
Opening the abscess of the maxillo-lingual groove
The incision is made in the area of the second and third molars between the lateral surface of the tongue root and the inner surface of the body of the lower jaw, avoiding damage to the lingual nerve and blood vessels. By dissecting the mucous membrane and submucosal layer between the midline of the groove close to the inner surface of the body of the lower jaw, then they penetrate into the depths of the purulent focus using a blunt method.
12.2.5. Chin area
Borders:
The chin area is limited:
• from above: chin-labial groove;
• below: the lower edge of the body of the lower jaw;
• on the sides: nasolabial folds.
Relief:
The relief of the area is determined by the peculiarities of the shape of the chin, which in some cases requires surgical correction (Fig. 142).
Rice. 142. Different shapes of the chin: 1 – heavy (massive) chin; 2 – finely outlined (smoothed) (according to: Kirpatovsky I.D., Bocharov V.Ya., 1974).
Microgenia
Microgenia is a congenital or acquired (unilateral or bilateral) underdevelopment of the lower jaw. In a bilateral process, as a result of the posterior displacement of the chin, the so-called “bird face” is formed. To correct microgenia, it is necessary not only to surgically lengthen the lower jaw, but also to correct secondary deformation of the upper jaw (retraction of the alveolar process and dentition with fan-shaped protrusion of the anterior teeth).
For treatment, two groups of surgical interventions are used:
1. Surgical interventions on soft tissues to change the external contours of the face.
2. Surgical interventions on the lower jaw to lengthen it.
The first group of operations is designed only to achieve a cosmetic effect through contouring of the soft tissues of the face:
• autocartilage;
• allocartilage;
• plastic (fluoroplastic, silicone).
Methods for surgical lengthening of the lower jaw are divided into the following groups:
1. Plastic (horizontal, step-like, oblique, arcuate) osteotomy.
2. Vertical osteotomy.
Progenia
Progenia is an enlargement of the lower jaw with protrusion of the chin and malocclusion. With this deformation, along with a violation of the shape of the face, the chewing function (biting) is significantly reduced.
There are true and false progeny.
With true progeny, all dimensions of the lower jaw are increased.
With false progeny, the relationship of the dentition is changed only in the frontal region (the lower teeth overlap the upper ones) with a neutral relationship of the first large molars.
• False frontal progeny can be caused by underdevelopment of the anterior part of the upper jaw.
• False forced progeny may be caused by the habitual forward displacement of the lower jaw when the nasopharynx is narrowed.
To eliminate progenia, several surgical options are used:
1. Horizontal osteotomy of the mandibular ramus.
2. Vertical osteotomy of the mandibular ramus.
3. Bilateral resection of the body of the lower jaw with preservation of the neurovascular bundle.
Prognathia
Prognathia is characterized by protrusion of the frontal part of the upper jaw in relation to the normally developed lower jaw.
This deformation of the facial skeleton is accompanied by the following symptoms:
1. Horizontal position of the front teeth of the lower jaw.
2. The upper lip is raised.
3. The lips of the mouth do not close.
4. Mouth half open.
5. The pronunciation of “labial” sounds is impaired.
Stratigraphy
Leather
The chin area is thickened compared to other parts of the face and is fused by connective tissue cords with the underlying fascia and facial muscles. In men, the skin has pronounced hair.
Subcutaneous fat thickness
small. The cellular structure of subcutaneous fatty tissue determines the limitation of hematomas and inflammatory processes in this layer.
Muscles
have a slight thickness and an oblique transverse course of the fibers:
• The muscle that lowers the lower lip (m. depressor labii inferioris) extends from the lower edge of the body of the lower jaw (starting outward from the mental angle) to the lower lip.
• When the muscle contracts, the chin-labial fold deepens, the lower lip lowers, turns out, helping to increase the visible part of the red border of the lips. The course of muscle fibers is longitudinal.
• The combined weak contraction of the muscle that depresses the lower lip and the muscles that depress the corners of the mouth contributes to the manifestation of sadness and grief.
• Significantly expressed contraction of these muscles contributes to the demonstration of contempt, disgust, and disgust.
• The subcutaneous muscle of the neck (m. platysma), passing from the neck to the chin region, is woven with separate fibers into the mental muscle and the muscles that lower the corners of the mouth. Contraction of this muscle enhances the lowering of the lower lip and corners of the mouth.
When the body of the lower jaw is fractured, a violation of the surface sensitivity of the skin of the chin and lower lip, mucous membrane of the gums, teeth develops, a change in pain and temperature sensitivity (parasthesia or anesthesia) due to compression or damage to the lower alveolar nerve (n. alveolaris inferior) - the largest branch of the mandibular nerve . Through the opening of the lower jaw (foramen mandibulae) this nerve enters the mandibular canal (canalis mandibularis). In it, the lower alveolar nerve gives off branches that, connecting with each other, form the lower dental plexus or directly dental and gingival branches that innervate the mucous membrane of the alveolar process and the gums of the lower jaw from the vestibular side. At the level of small molars, a large branch departs from the lower alveolar nerve - the mental nerve (n. mentalis), which exits through the mental foramen and innervates the skin, mucous membrane of the lower lip, and skin of the chin (Fig. 143).
Rice. 143. Position of the needle when introducing an anesthetic solution into the foramen mentale (according to: Bocharov N.N., 1970).
Topographic-anatomical basis of anesthesia of the mental nerve
The mental foramen with the exiting nerve is located under the 2nd small molar in the middle of the height of the body of the lower jaw (the canal is directed posteriorly, upward and outward).
The main stages of manipulation when using the extraoral method:
• fixation of the skin with the finger of the left hand at the site of the projection of the mental foramen;
• inserting a needle into the soft tissue above and posterior to the projection of the hole and then moving it forward, down and posterior to the projection point of the hole;
• bringing the end of the needle to the hole and introducing 0.5–2 ml of novocaine solution into its lumen.
The main stages of manipulation using the intraoral method:
• inserting a needle forward, downward and inward into the transitional fold of the mucous membrane of the oral vestibule slightly above and posterior to the projection point of the hole (corresponding to the first large molar);
• advancement of the needle in depth by 7 – 10 mm;
• performing nerve anesthesia after reaching the mental foramen.
Language structure
The human tongue is a soft pink colored muscle mass on which taste buds are located. At the very top of the tongue, and along its edges, there are papillae, which are responsible for the taste of everything that comes into our mouth. It is no secret that the mouth is the first point where the initial processing of food and the adsorption of microorganisms and harmful substances begins. The tongue takes on the most important role here, accumulating on its surface all the harmful substances that form a coating known to everyone. It is imperative, for preventive purposes, to clean your tongue of plaque, which will get rid of the unpleasant odor and possible infections. At the root of the tongue, there are no papillae, there are tonsils. Which play an important role in protecting the human body, standing in the way of microbes, they do not allow them to penetrate inside.
Sky structure
The part of the oral cavity that is located on top is called the palate. The palate is made up of 2 components, hard and soft. The mucous membrane covers both parts, passing through the hard palate to the soft palate, it gradually turns into gums. The front side of the palate forms rudimentary formations (palatine alveoli), humans do not fully use them, but animals, on the contrary, use them to eat food. The palate has another role besides forming the upper part of the mouth; it is a barrier between the nose and nasopharynx. A kind of barrier wall is a small tongue that blocks access to the nasopharynx during the digestion process.
What diseases does it indicate?
Staining of the vault of the oral cavity indicates the presence of diseases of the gastrointestinal tract, liver and kidneys. The reason for the color change may be a violation of the body's absorption of fats.
Yellowing of the dome of the oral cavity can be a clinical manifestation of a number of pathologies:
- Acute and chronic liver diseases. The yellowness of the mucous membrane is caused by an increase in bilirubin in the blood. The liver is an organ responsible for the exchange of useful components and nutrients. Dysfunction of this organ provokes serious consequences for the body.
- Cholelithiasis. The formation of stones from salt and cholesterol in the gallbladder stops the movement of bile. Stagnation disrupts metabolism and contributes to the development of the inflammatory process.
- Colitis, ulcer or gastritis. The reflux of acidic stomach contents leads to irritation of the oral mucosa and a change in color.
- Kidney failure. Due to disturbances in the urinary system, yellowing of the palate occurs.
- Syphilis. Yellow spots and plaque may indicate an infectious liver lesion in the second stage of the disease.
Damage to internal organs can be caused by infections, diseases or systemic disorders. Yellow sky is a clinical symptom of internal pathologies.
Associated symptoms
The diseases listed above are manifested by an extensive list of clinical symptoms, not limited to yellowing of the oral vault. This list includes:
- swelling, increased or decreased urine output;
- insufficient blood supply to the extremities, weakness, trophic disorders, numbness;
- dysfunction and bloating in the gastrointestinal tract;
- weight loss or weight gain;
- fainting;
- chronic fatigue;
- hypertension, nausea;
- vomiting, dehydration, intense muscle pain.
If alarming symptoms appear, you should seek help from a general practitioner, who, if necessary, will refer you to a gastroenterologist, nephrologist or other specialist doctor.
Treatment and prevention
When the color of the oral cavity changes, it is difficult for the doctor to quickly determine the problem that the patient is facing. Competent diagnosis using instrumental and laboratory tests and highly targeted treatment are required.
If liver, gastrointestinal or kidney diseases are detected, the therapist begins treatment. If necessary, the patient is referred to specialist doctors for further examination. For infectious lesions, complex inpatient therapy is required.
Local infection of the oral cavity is treated in a dental setting. Antibiotic therapy, professional oral hygiene and sanitation are carried out.
A change in the color, texture, or condition of your mouth is a warning sign that requires a visit to your dentist. Do not ignore deterioration in health or changes in appearance. A change in the color of mucous membranes may be the initial manifestation of a serious disease. Competent diagnosis and timely treatment will prevent deterioration of health and the development of complications.
Structure of the mucous membrane
The entire human oral cavity is covered with a mucous membrane, which has a distinctive feature, regenerative ability. The mucous membrane protects the oral cavity from environmental influences. Chemical, mechanical, temperature factors cannot influence it. The structure of the mucous membrane is simple; in the lower part of the mouth - on the cheeks and lips, it forms folds; in the upper part - attached to the bones. The main roles of the mucous membrane:
- The protective role is unpleasant, but it is a fact that many viruses and bacteria accumulate in the human mouth. The mucous membrane retains, prevents reproduction and removes all harmful microorganisms from the oral cavity.
- Sensitive role - Due to the presence on its surface of many receptors responsible for sensations (taste, pain, temperature), it signals all the events that accompany food intake.
- Absorption role – Thanks to this ability, we are able to take medications “under the tongue”. The mucous membrane perfectly absorbs protein and mineral compounds.
Reasons for color change
A yellow tint may appear due to smoking. Tar and tobacco smoke stain the mucous membrane, settling on the surface. A yellow coating appears. Due to vascular contraction and changes in blood composition, blood supply is disrupted. With a lack of oxygen, the mucous membrane turns pale and yellow.
The causes of yellowing of the palate are diseases of the oral cavity and body. This is also caused by age-related changes due to metabolic disorders and blood microcirculation.