Swelling after surgery is a natural phenomenon after any surgical intervention, including plastic surgery. Injured tissues need time to recover, complex processes take place in them, and therefore you just need to be patient a little...
After all, after a few weeks, looking in the mirror, you will forget about your experiences and inconveniences endured - they will seem insignificant before the miracle of transformation, before your dream come true - about a young, fresh face, high and youthful breasts, graceful contours of the figure...
And although “time heals,” there is a great opportunity to help him. How - we will talk about this further.
About lymphedema
Lymphedema is a swelling condition that can develop in the legs after lymph nodes are removed or injured. Lymph nodes are small, bean-shaped structures that are located throughout the body. They drain fluid away from different areas of your body. The inability to drain fluid leads to tissue swelling.
During surgery, lymph nodes in your pelvis were removed to get rid of any remaining cancer cells. This increases the risk of developing leg lymphedema. The risk will be higher if you have had radiation therapy or had lymph nodes removed in your groin. If you only have lymph nodes in your pelvis removed, you may be less likely to develop leg lymphedema.
Lymphedema may develop immediately after surgery or years later.
to come back to the beginning
Reasons for appearance
Any plastic correction on the face involves tissue injury during the work. The difference lies in the volume of injured tissue - for example, with a circular lift, more incisions are made than with a thread lift. Even safe ultrasonic SMAS lifting destroys and damages tissue in the deep layers.
When tissues are damaged, as a response to traumatic effects, new volumes of interstitial fluid begin to be produced, which promotes healing and restoration of blood vessels, lymphatic channels and other systems at the site of the damaged ones. Visually it looks like swelling. The face is more prone to swelling than other parts of the body, especially in the area around the eyes, since these areas contain the thinnest tissues in which fluid can more easily accumulate.
The area around the eyes is especially prone to puffiness.
Risk factors for developing leg lymphedema
Risk factors for developing leg lymphedema include:
- weight gain or excess weight;
- infection of the affected leg;
- radiotherapy of the pelvic area;
- reappearance of cancer.
There are other factors that are thought to increase this risk. These include:
- Sedentary lifestyle.
- Flying on an airplane.
- Compression of the leg. It occurs when there is a tight ring of pressure in one area of the leg and is often caused by wearing certain clothing.
- Exposure to extreme temperatures.
to come back to the beginning
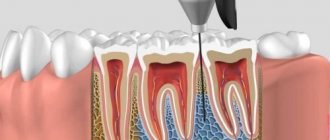
Why does numbness occur after dental implantation?
The first hours after dental implantation, anesthesia continues to be active, especially if it was about installing several implants at once. As a rule, a conduction method is used, which ensures blocking of nerve endings for up to 5-6 hours. But the implantation procedure itself takes no more than 2-3 hours, so after it, numbness can actually persist: in some patients - for a couple of hours, in others - up to 5-6 hours. In both cases, this is the norm, and the duration of anesthesia depends on the condition of the body.
Slight numbness of facial tissues can persist for 2-3 days - it is inextricably linked with swelling. But if sensitivity is not restored, you should consult a doctor. The causes of this condition may be damage to the facial or jaw nerve: the sooner treatment is started, the higher the chance of completely restoring tissue sensitivity.
Read more about what facial neuralgia is as a complication after dental implantation >>>
Swelling and numbness are the body’s natural reaction to the “invasion” of a foreign body, that is, an implant. Take a mini-vacation from work for 3-4 days, try to lead a more measured pace of life, give up business trips and important business meetings - give your body rest, because it needs strength to recover. If you want to reduce the risks of any consequences and complications to zero, try to carefully approach the issue of dental implantation, trust your doctor and follow all his recommendations.
How to reduce your risk of developing lymphedema
It is impossible to predict which patients will develop lymphedema, but there are preventive measures to reduce the risk of its occurrence.
Protect your skin
One of the measures to reduce the risk of developing lymphedema is to protect the skin as much as possible from injury or infection. This is because the affected area begins to receive cells that fight the infection, which in turn causes swelling. Your legs may simply not be able to handle the removal of this extra fluid.
Treat cuts and scrapes
- Wash the area with soap and water.
- Apply first aid ointment to it.
- Place a clean, dry gauze pad or Band-Aid® over the top.
Treat burns
- Wrap an ice pack in a towel and apply to the burn for 15 minutes. You can also wash the burn with cold water.
- Wash the area with soap and water.
- Apply first aid ointment to it.
- Place a clean, dry gauze pad or bandage on top.
Watch for symptoms of infection, which include:
- redness;
- edema;
- heating of surrounding tissues;
- sensitivity.
Call your doctor or nurse if you have these symptoms.
Don't wear tight clothes
Avoid wearing tight clothing that leaves deep marks on your legs, such as socks or sweatpants with elastic cuffs. Wear loose-fitting clothing that does not leave marks on your legs.
Compression garments, which prevent severe swelling from occurring, work differently. It ensures uniform pressure on the leg and proper fluid flow through it. You can learn more about compression stockings in the Compression Stockings section of this resource.
Avoid exposure to extreme temperatures
Extreme heat and cold can cause fluid to accumulate in the leg and cause swelling. Avoid or reduce time in hot baths or saunas.
Be careful when flying by plane
If you are at risk for lymphedema, air travel is associated with certain negative factors, including:
- Cabin pressure. The pressure in the cabin of an airplane is usually slightly less than the pressure on the ground. This causes the skin to stretch and fluid to accumulate in the legs.
- Sitting motionless for long periods of time. If you don't move for a long period of time, fluid can accumulate in your legs.
- Lifting and carrying luggage can cause muscle strain.
- Dehydration (when your body does not get the amount of water it needs).
Here are some tips to help reduce your risk of developing lymphedema:
- Buy a seat with sufficient legroom, such as a seat at the front of the cabin.
- Ask for help to carry, lift or remove luggage that is too heavy for you.
- Stand up and walk up and down the airplane aisle if possible.
- While sitting, do simple exercises with your feet and ankles. Exercise throughout the flight will help restore circulation and movement of lymphatic fluid. You can try the following exercises: Point your toes towards the ceiling and then lower them towards the floor.
- Make circular movements with your feet in one direction and then in the other.
Other ways to reduce risk
- Do not give injections (shots) or acupuncture into your affected leg(s).
- Do not use sharp pedicure tools. Use cuticle remover cream and file your nails instead of trimming them.
- Moisturize your skin frequently to avoid flaking and cracking.
- Keep the area between your toes clean and dry to prevent infections.
- Don't go barefoot.
- Make sure your shoes fit your feet to avoid blisters.
- Make sure your toe rings or ankle bracelets fit loosely.
- Try to sit cross-legged as little as possible.
- Choose a sunscreen with an SPF of at least 30 to protect your skin from sunburn.
- Try not to gain weight, as excess weight is one of the risk factors for developing lymphedema. If you are overweight, try to lose weight.
- Limit your salt intake. Its use can lead to swelling, which will put excess strain on the lymphatic system.
to come back to the beginning
Is it possible to speed up recovery?
In order for the healing process to be quick and painless, the patient must follow some rules, prohibitions and recommendations. At least during recovery, you should give up bad habits - alcohol and cigarettes, as these products reduce the speed of healing. You will also have to give up sports and physical activity, visiting the bathhouse, sauna, solarium, beach, and taking hot baths. In the first week after correction, you should not wash your hair.
To get rid of swelling faster, it is advisable to remove salt from your diet. Contrary to some myths, you should not take diuretics. But there is no need to reduce water consumption - on the contrary, it is recommended to drink more than a liter of clean drinking water daily. In the first days, it is better to eat light foods that do not burden digestion. Only full compliance with all doctor’s prescriptions will help make recovery short and simple.
How to recognize the first signs of lymphedema
After surgery, swelling occurs at the incision site (surgical suture) in all patients. This is normal and will subside a few weeks after surgery.
Swelling caused by lymphedema usually occurs in the lower leg(s). If left untreated, it can spread throughout the leg and all the way to the torso. At first, this swelling may appear and disappear. It may decrease as you lift your leg higher than your chest.
Other early symptoms may include a feeling of heaviness in your leg(s) or a feeling that clothes, socks or shoes are pressing in on you.
to come back to the beginning
What to do at home
After surgery to replace the hip joint, in the absence of complications, the patient is discharged on days 8–10. If swelling persists by this time, it is necessary to carry out complex treatment at home, including drug therapy, folk remedies, exercise therapy, massage and diet.
Traditional treatment includes taking diuretics (Veroshpiron, Furosemide, Diacarb). It should be taken into account that, in addition to Veroshpiron (potassium-sparing), other drugs in this group remove potassium along with the liquid. Therefore, drugs containing potassium (Potassium orotate, Asparkam) are simultaneously prescribed. Medicines are taken orally according to a special regimen; in case of severe swelling, injections are given.
Ointments and gels that normalize fluid circulation in tissues (Troxevasin, Heparin ointments, Essaven gel) are indicated locally.
Traditional medicine uses decoctions, infusions, compresses, and baths. Folk remedies are only an addition to the main therapy. Before using traditional medicine, you should consult your doctor.
Other Lymphedema Treatments
There are other treatments for lymphedema. Talk to your doctor or lymphedema therapist about which ones are right for you.
Other treatments for lymphedema include:
- Treatment of scars. Scarring from surgery can make it difficult for your body to eliminate fluid. Scar treatments help soften the area around the scar and make it less tight. It will help drain fluid from your legs.
- Improved posture.
- Using kinesiology tape for athletes.
to come back to the beginning
Cosmetology and drug therapy
You can also get rid of swelling and stimulate tissue healing with the help of cosmetic procedures and certain medications. Plasmolifting, ultrasound therapy and phototherapy help well. Also, after plastic surgery on the face, it is important to provide the skin with proper care in order to maintain the result of the correction for a long time. For example, mesotherapy and biorevitalization will help with this.
Among the drugs most often prescribed are those to strengthen the walls of blood vessels, normalize blood circulation and improve venous outflow. Taking vitamin complexes is also recommended. Antibiotics may be prescribed to prevent infection.
Neither cosmetic procedures nor medications can be prescribed independently. Only a doctor can prescribe supplements or recommend cosmetic and physical procedures.
Plasmolifting can be prescribed both after facial plastic surgery and before it - as a preparation.
Make an appointment
To make an appointment with a lymphedema therapist, contact your healthcare provider. They will decide together which lymphedema therapy is right for you. Once your doctor has made a referral, you will be contacted to schedule an appointment. If you have any questions, call Rehabilitation Service at 212-639-7833.
Lymphedema therapy is provided at several Memorial Sloan Kettering locations. For more information, visit www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/rehabilitation/medicine-therapy.
To find a lymphedema therapist in your area, you can visit the following websites:
Klose Training
www.klosetraining.com
Norton School of Lymphatic Therapy
www.nortonschool.com
Academy of Lymphatic Studies
www.acols.com
Lymphatic Association of North America
www.clt-lana.org
to come back to the beginning
What is done in a hospital setting to prevent or reduce swelling
To avoid the occurrence of edema, the following measures are carried out in a hospital setting:
At the stage of preparation for surgery:
- carrying out therapy for chronic diseases until complete remission is achieved;
- clinical examination of the patient, laboratory and instrumental diagnostics to exclude inflammatory processes;
- within 2 hours, broad-spectrum antibiotics are used that act against pathogens of many infections;
- 12 hours before surgery, anticoagulants are prescribed - blood thinners (heparin) to prevent thrombosis;
- thorough disinfection of the operating room.
During the operation, it is performed in a highly professional manner with minimal trauma under sterile conditions. Individual selection of a prosthesis taking into account the age and condition of the patient. The prosthesis must be made from materials that are optimally compatible with body tissues. Prosthetics must be carried out in such a way that the integrity of the implant is not compromised and infection and inflammation do not occur.
In the postoperative period:
- continuation of therapy with antibiotics and anticoagulants for another 5 - 7 days after the intervention;
- the beginning of rehabilitation from the first day to avoid blood stagnation and the development of edema - exercise therapy, physiotherapy, breathing exercises;
- professional wound treatment to prevent infection;
- in case of swelling (usually on the 2nd - 3rd day) - elimination of the cause that led to the problem, the use of diuretics, ointments and gels that reduce swelling, a special set of therapeutic exercises;
- specialists perform lymphatic drainage - alternating light stroking of the skin and deep massage of the lymph nodes;
- training the patient to perform exercise therapy at home, informing about possible complications and preventive measures to prevent them.
Compression cuffs to prevent swelling and thrombosis.