September 9, 2022 Colds in children are one of the most exciting topics for parents. Every mother wants her baby to always be healthy and to avoid any illness, and she becomes scared when the thermometer shows a high temperature in the child. However, one way or another, the child’s body has to deal with various infections.
Regular acute respiratory viral infections in children are associated by parents with long absences from kindergarten and school. Moreover, regular viral diseases can lead to the development of various complications.
How often do children get sick?
Children under 5 years old experience up to 8 episodes of ARVI per year1. In kindergartens, the morbidity rate is especially high in the first and second year of attendance - 10-15% higher than at other times.
The number of visits to pediatricians with ARVI increases from September to April, and the peak incidence occurs from February to March. In the summer months, the incidence decreases by approximately 3-5 times.
Children are especially vulnerable to influenza. The reason for this is insufficiently developed immunity. The spread of the virus in children's groups (in schools, kindergartens, boarding schools) is occurring rapidly.
Immunity in children. Why do children get sick more often?
The immune system of children develops throughout childhood.
The immunity of infants is imperfect and this feature is a special mechanism that protects the body from too violent immune reactions to infections.
In the first weeks of life, the baby is protected by the antibodies that he received from his mother and then continues to receive them through breast milk. But such protection is sometimes not enough.
Moreover, while immunity is just developing, periods of maximum risk of developing infectious diseases arise; they are called critical periods:
First critical period
This is a period of vulnerability for newborns, which occurs in the first 28 days of life. During this period of time, the child’s body is protected only thanks to antibodies received from the mother through the placenta and breast milk. The risk of contracting bacterial and viral infections during this period is very high. Premature newborns are a special risk group.
Second critical period
Lasts from 4 to 6 months of life and is accompanied by a decrease in the amount of maternal antibodies.
Due to some mechanisms, which are also still poorly developed, the child’s own antibodies are produced, but they are not yet sufficient to protect the baby. Therefore, the body’s susceptibility to airborne and intestinal infections during this period is also high. Thus, in children under one year of age, all the basic mechanisms of the body’s defense against bacteria and viruses are weakened.
Third critical period
Occurs in the 2nd year of life. It is from this age that the child begins to have more and more contact with the outside world and various infections. The child's sensitivity to respiratory and intestinal infections is still high. The baby's immune defense mechanisms are not yet fully developed.
Fourth critical period
Appears at 6-7 years of age. Children of this age are also prone to infectious diseases, as some indicators of the immune system change.
Fifth critical period
Adolescence from 12-15 years, and the age may vary slightly for boys and girls. This is due to an increase in the secretion of sex hormones, which slightly weakens the immune system. Children of this age are characterized by high sensitivity to viral infections.2
Types of immunity
Immunity includes humoral and cellular immunity. Let's look at each of them in more detail. Humoral is ensured by the presence of antibodies (substances that bind to antigens) in the blood. Cellular is provided by cells of the immune system. Immunity can be congenital or acquired. In turn, the acquired one can be active or passive. Active develops after illness, for example, ARVI. It also forms after vaccination. Passive is formed when ready-made antibodies are transfused into the body in the form of serum. It also develops when antibodies are passed from a mother's milk to her newborn baby. In fact, natural immunity includes congenital immunity, acquired after an illness, as well as passive immunity during the transfer of antibodies from mother to baby. Artificial immunity is called immunity after the introduction of a vaccine or serum with antibodies.
ARVI or flu
Despite the fact that influenza is part of the group of acute respiratory viral infections (acute respiratory viral diseases) and their symptoms are very similar, the manifestations of influenza are more pronounced.
If the symptoms of a cold are accompanied by a runny nose, nasal congestion, sore throat, headache, low-grade fever, cough and general malaise, then with the flu there is a sudden onset of illness, high temperature, and fever.
With influenza, the risk of developing bacterial complications, such as bronchitis, pneumonia and otitis media, is many times higher than with regular acute respiratory viral infections.
Indications for use
According to the instructions for use, the drug "Viburkol" is effective in the following conditions:
- fevers of various etiologies,
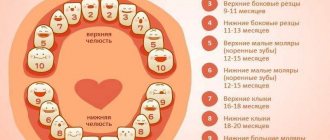
- severe pain during the growth of the first teeth (recommended for children under 3 years of age),
- viral, fungal and bacterial infections,
- diseases of the genitourinary system,
- childhood dyspepsia - disruptions in the digestive tract, stomach pain, cramps and flatulence,
- mild disorders of the nervous system - anxiety syndrome, seizures and other symptoms.
Baby becomes restless when teething
How is the virus transmitted among children?
The influenza virus is transmitted from child to child by sneezing, coughing and talking.
Among children, contact transmission of the virus is common through household items, children's toys, dishes, bedding and various surfaces. The fact is that a virus - for example, the influenza virus - can survive for 2 hours on tables, door handles, pencils, etc. After playing with shared toys or touching the table, the child then touches his face, nose and eyes with his hands.
During epidemic seasons, outbreaks of ARVI and influenza are observed in collective places, most often kindergartens, less often schools.
Symptoms of ARVI in children:
Flu Symptoms
- acute onset with a sharp rise in temperature to 39-40.5C°
- severe aches in the body and joints
- headache, eye pain
- lethargy, weakness, malaise
- decreased or lack of appetite
- nasal congestion, minor rhinitis, dry cough
- may have a sore throat
- sometimes nausea, vomiting, diarrhea.
ARVI symptoms
- acute onset with an increase in body temperature to 37.5-38.0°C.
- aches in the body and joints
- headache
- lethargy, weakness, malaise
- decreased or lack of appetite
- rare to heavy mucous discharge from the nose, nasal congestion
- cough, dry or wet
- sore throat and discomfort
With ARVI, in most sick children the temperature drops on the 2-3rd day of illness. With the flu, the temperature can last up to 5-7 days. If the temperature does not decrease during the course of the illness, this may indicate a bacterial infection.
Symptoms of vitamin deficiency
A lack of certain vitamins can lead to decreased immunity.
Hypovitaminosis, as a rule, has nonspecific symptoms. These include: increased fatigue, decreased body defenses, weakness, lethargy. Vitamin deficiencies have more specific (certain) symptoms. We will not dwell on each vitamin deficiency in more detail, but will only consider vitamins, the lack of which can lead to a decrease in immunity.
These include:
- Vitamin A . Its deficiency is manifested by damage to the eyes, skin, and increased susceptibility to infections.
- Vitamins of group B6 (pyridoxine, pyridoxal). A lack of these substances can lead to dermatitis, lymphopenia (decreased levels of immune cells), anemia, and convulsions.
- Biotin . A deficiency of this substance can lead to seborrhea, hair loss, and deterioration of the immune system.
- Vitamin C . A lack of vitamin C leads to increased fragility of blood vessels, fatigue, pain in the limbs, tooth loss, poor wound healing, and increased susceptibility to infections.
- Vitamin D . A lack of vitamin D leads to the development of rickets in the baby, which is also accompanied by a decrease in immunity and an increase in the overall morbidity of the baby.
Clinical manifestations of ARVI and influenza
- nasopharyngitis - nasal congestion, mucous discharge from the nasal passages, discomfort in the throat in the form of soreness, burning; Mucus may drain down the back of the throat, which can cause a wet cough (nasal congestion, mucus discharge and sore throat can cause the child to become restless, including refusing to eat)
- eustacheitis and otitis media - pain in the ears appears, with some forms of otitis there is a decrease in hearing, with otitis media a high temperature also rises
- Laryngitis is manifested by hoarseness of voice, rough cough, but there is no difficulty breathing
- pharyngitis is characterized by a red throat, namely the back wall of the pharynx and palatine arches; the mucous membrane is loose and edematous; mucus may drain down the back of the throat; with pharyngitis, a dry, obsessive cough is common
- tracheitis is a disease that can cause a strong obsessive cough
- croup syndrome (obstructive laryngotracheitis) is characterized by laryngeal stenosis; this condition is a common occurrence among preschool children with ARVI
What else can you give your baby to expose his condition?
Currently, there is simply no complete analogue of the drug “Viburkol” with the same composition. However, there are plenty of products in pharmacies that doctors allow to be used to alleviate the condition of children as their baby teeth grow. Below are the most popular options:
- based on paracetamol: “Cefekon” and “Efferalgan” - help lower the temperature and reduce pain,
- based on ibuprofen: “Nurofen” and “Ibufen” - also help reduce temperature and block pain,
- gels with anesthetic: “Dentinox” and “Kamistad” - for application to the gums to reduce pain.
If the baby's temperature has risen sharply, not rectal suppositories, but antipyretic drugs in the form of syrups will be more effective. As for local pain relievers, due to the immediate action of lidocoin, they give the desired effect faster than others. If the symptoms are too severe and the temperature exceeds the permissible norms, the child should be immediately shown to a doctor. And remember: any medications, even those based on natural ingredients, should be given to the baby only with the permission of a specialist.
- Elizarova, V.M. Trend in changes in the timing of the eruption of primary teeth in the modern generation of children, 2002.
Fever due to ARVI and influenza
Fever is a temporary increase in body temperature due to some illness. Fever is one of the symptoms of ARVI and influenza.
High temperature is the body’s protective reaction to a pathogen that has entered the body. Many viruses and bacteria stop reproducing at temperatures above 37-38°C, and the formation of antibodies is also stimulated.
There are “pink” and “white” fever.
For pink fever:
- heat production and heat transfer mechanisms are adjusted correctly
- baby's skin is pink and hot to the touch
For white fever:
- centralization of blood circulation (blood circulation is aimed at preserving the functioning of the heart, lungs, brain) and disruption of blood microcirculation
- limbs are cold, pale
- bluish leather with marble pattern
- "goose pimples"
- chills
Such a course of fever may be unfavorable.3
Diagnosis of colds in children
The most effective diagnosis of all viral diseases among children is timely contact with a pediatrician. The doctor has information about the epidemiological situation in the region, about outbreaks of the circulating virus in kindergartens and schools. It is very important to collect a detailed medical history of the child and obtain information about possible contacts with patients. All of the above factors will help determine the suspected pathogen.
Among children, virological or bacteriological testing is not recommended, since this does not affect treatment tactics. Most often, children quickly recover on their own, which does not require the use of special laboratory diagnostic methods. Exceptions include a rapid influenza test in children with a high fever and a rapid streptococcal test for suspected acute streptococcal tonsillitis.4
A general blood test, a general urinalysis and other laboratory tests are prescribed strictly by a doctor!
Treatment of colds in children
The main method of treating ARVI and influenza in children is symptomatic therapy, that is, therapy that reduces certain symptoms such as high fever, cough, runny nose, sore throat:5
- taking antipyretics
- vasoconstrictor nasal drops
- rinsing the nose with saline solution
- gargling with antiseptic solutions
- local therapy in the form of sprays and tablets for sore throat (different formulations for different ages)
- physical methods to reduce temperature
In case of high fever, it is necessary to undress the child, remove excess blankets, and clothing should not make breathing difficult. It is also necessary to provide access to fresh air whenever possible. If necessary, wiping with water at room temperature is carried out, since wiping with water improves heat transfer. It is strongly not recommended to wipe a child with alcohol, as alcohol may be absorbed (especially in young children) and poison the child’s body.
Antiviral therapy is applicable only for influenza, but in children antiviral drugs are prescribed strictly by a pediatrician!
Antibacterial therapy is prescribed strictly according to indications. Antibiotics are justified only for severe bacterial complications, including ARVI and influenza. Antibiotics do not work against the virus!
General therapeutic measures:
- The child’s nutrition should be complete and rich in vitamins
- the child should drink enough liquid (water, tea with lemon, decoctions of rose hips, raspberries, black currants, strawberries, cranberries, lingonberries), since drinking plenty of fluids prevents dehydration and reduces intoxication at high temperatures
- bed rest
- ventilation of premises
- wet cleaning of premises
An increase in body temperature within 38-39°C does not require the use of antipyretic drugs. In this case, you can limit yourself to physical cooling methods. But age up to 2 months, severe diseases of the respiratory system, circulatory system, central nervous system, history of febrile convulsions are indications for the use of antipyretics, even if the temperature rises to 38°C.
In any case, the mother should first assess the child’s reaction to the increase in temperature by analyzing his behavior: is there lethargy, does the child refuse water and drink, what color is his skin and how does it feel to the touch. If the child is active, the skin is pink, and the limbs are warm, then you can limit yourself to physical methods of reducing the temperature. If white fever appears, then antipyretic medications should be given to the child immediately.
Despite a number of effective antipyretic drugs, paracetamol and ibuprofen remain the best drugs for children.
Vitamins and their role in immunity
Vitamins are substances necessary for normal life, the formation of which in the body is absent or very limited. Basically, the source of these substances in children is food and intestinal bacteria, which are also capable of forming them.
They have their own characteristics:
- They are not included in the structure of the baby’s organs and tissues.
- Not used by the body as a source of energy.
Depending on their ability to dissolve in water or fat, vitamins are divided into two large groups:
- Fat soluble . These include vitamins A, D, E, K, as well as vitamin-like substances - ubiquinone (vitamin Q), essential fatty acids (vitamin F).
- Water soluble . These include vitamins B, H, C, vitamin-like substances - choline, lipoic acid, carnitine, orotic acid and others.
Unfortunately, there are reasons that can lead to a decrease in the level of these substances in the body. This problem has a medical name - hypo- and avitaminosis.
Causes of hypo- and avitaminosis:
- Impact of environmental factors.
- Poor nutrition.
- Malabsorption.
- High need (for example, in premature infants and during puberty).
- Liver diseases.
- Increased breakdown of vitamins.
- Damage to intestinal microflora. You can find out more about this problem in our article.
What should not be done in case of acute respiratory viral infections and influenza in a child?
- 1. Since antipyretics are prescribed according to the child’s age, as a rule, the dosage is adjusted according to the child’s weight. Long-term regular use (2-4 times a day) of antipyretics should be avoided due to the danger of side effects and possible difficulty in diagnosing bacterial complications (otitis media, pneumonia, etc.). A repeat dose should be given only when the temperature rises again. If the temperature does not decrease within several hours, you must call an ambulance.
- 2. A child with a fever should not be wrapped. If you dress your child warmly, you can disrupt the process of heat formation and heat transfer, which helps maintain the desired body temperature. Wrapping up can lead to overheating and loss of consciousness.
- 3. You cannot close the windows in the room. A sick child needs fresh air. Frequent ventilation also makes breathing easier.
- 4. You should not take antibiotics without a reason. Antibiotics do not act on viruses and do not prevent bacterial complications.
- 5. You should not use cough medications yourself. Different medications are aimed at treating specific cough problems. Not everyone is prescribed antitussives or mucolytics. Moreover, most often such drugs are not needed in treatment. Everything is individual and the use of such medications should be agreed with the pediatrician.
- 6. You cannot give up walking for several weeks. Short walks will only be beneficial. The child needs fresh air and movement. Of course, walks are justified only after the fever has decreased and the condition has normalized, if the child is active.
- 7. It is not entirely justified to refuse bath procedures during an acute respiratory viral infection for several days or weeks. On the contrary, a child can swim. Exceptions are, of course, high fever and otitis media.
- 8. In relation to the child, any methods of self-medication should be excluded.
All therapeutic measures are carried out only as prescribed and under the supervision of a doctor.
What's included
The product in question contains only natural ingredients, and therefore has virtually no contraindications. Among the active ingredients of the drug:
- belladonna extract,
- pharmaceutical chamomile,
- bittersweet nightshade extract,
- plantain extract,
- calcium carbonate,
- meadow lumbago juice.
“When my son started teething, his temperature jumped, he had a runny nose - in short, the whole set. So, Viburkol helped us a lot. One candle was enough for the baby to fall asleep peacefully for the first time in a long time and not wake up all night! Therefore, I gave him this remedy for some time, and with it that terrible period passed easily and quickly. The temperature, however, was still there, but not as high as before using the suppositories.”
Alena D., Vladivostok, from correspondence on the women's forum
Chamomile, which is part of the drug, helps relieve inflammation.
Chamomile, which is part of the drug, helps relieve inflammation and reduce pain. Bittersweet nightshade fights infections in the body that cause fever. Belladonna also helps relieve inflammatory processes, but meadow lumbago is responsible for normalizing the functioning of the digestive and nervous systems. Plantain extract helps stop bleeding and reduce swelling.