- Changing mode
There are many reasons why the cheek becomes numb. Numbness is not always associated with any disease. More often, the phenomenon occurs for a short time, due to an uncomfortable position of the head, prolonged sitting in an uncomfortable position, during an attack of fear or panic. Less commonly, the cheek becomes numb due to damage to the nervous tissue or vascular pathology. If a symptom occurs frequently, you should consult a doctor to determine the cause and prescribe treatment.
Most often, cheek numbness does not require treatment, but there may be exceptions.
general information
The trigeminal nerve consists of sensory and motor fibers. It originates in the structures of the brain and is divided into three branches:
- ophthalmic: responsible for the eye, forehead and upper eyelid;
- maxillary: innervates the area from the lower eyelid to the upper lip;
- mandibular: involves the chin, lower jaw, lips and gums.
With neuralgia, one or more branches of the trigeminal nerve are affected, which determines the main symptoms of the pathology. People over 45 years of age are most susceptible to the disease, and women get sick more often than men.
Make an appointment
Causes of jaw clenching during trismus
- inflammation of the masticatory muscles;
- inflammation of the gums;
- caries;
- abscess;
- inflammation of the periosteum of the lower jaw;
- jaw injuries (cracks, fractures, dislocations);
- dousing with cold water;
- animal or insect bites.
Trismus can also be a consequence of the following diseases:
- osteomyelitis of the jaw;
- periostitis;
- neurosis;
- epilepsy;
- meningitis;
- hysteria;
- arthrosis of the jaw joint;
- cancerous tumors;
- convulsions;
- rabies;
- tetany;
- paralysis;
- tetanus;
- pulpitis in the acute stage, etc.
Causes
The causes of trigeminal neuralgia can be of different nature:
- compression of the entire trigeminal nerve or its branches against the background of: enlargement of the arteries or veins of the brain (aneurysms, atherosclerosis, strokes, increased intracranial pressure due to osteochondrosis, congenital developmental features);
- tumors of the brain or facial tissues in close proximity to nerve fibers;
- congenital anomalies of bone structure, narrowed openings through which nerve branches pass;
- injuries of the skull, facial area: bone fractures, post-traumatic scars of soft tissues;
- proliferation of scar tissue after injury, surgery, inflammation;
The risk of developing trigeminal neuralgia increases significantly:
- over the age of 50;
- against the background of mental disorders;
- with regular hypothermia;
- with insufficient intake of nutrients and vitamins into the body (anorexia, bulimia, malabsorption, etc.);
- with regular overwork, stress;
- for helminthic infestations and other helminthiases;
- for acute infections: malaria, syphilis, botulism, etc.;
- for chronic inflammation in the oral cavity (caries, gingivitis, abscesses, etc.);
- against the background of autoimmune lesions;
- with excessive exposure to allergies;
- for metabolic disorders.
What is arthrosis of the TMJ
Arthrosis of the TMJ is a disease that destroys the components that form the joint (Greek arthron joint, suffix oz - destruction). First, the articular cartilage is destroyed, then the following occurs in the articular elements:
- proliferation (tissue growth);
- calcification (calcium redistribution) and ossification of cartilage;
- hyperplastic (proliferation) and destructive (destruction) processes in the epiphyseal parts of bones (these are the rounded ends of the bones - the head and fossa);
- reactive-inflammatory (from the word “response”) changes in the synovial membrane;
- fibrosis (overgrowth of connective tissue) with hardening of the joint capsule, which affects nearby muscles, tendons and ligaments.
With the destruction of cartilage, its shock-absorbing functions are reduced, and impacts are transmitted directly to the bone. Patients involuntarily increase the destruction by reacting emotionally to events - they clench their teeth, not daring to say too much, with a “stony” face and tense muscles, compressed blood vessels and stress hormones, they face the blows of fate. The amount of nutrients decreases, the TMJ would be happy to recover - but there is no building material. Instead, the epiphyseal sections of the bone are flattened under pressure, and bone growths appear on them.
Then the joint enlarges, compressing the nerve endings located nearby. The pain radiates to the ear, back of the head, and teeth. When the jaw moves, a specific clicking sound appears (occlusion-articulation syndrome).
ICD codes M.19. 0 (1, 2, 8 – last digit changes)
Symptoms
The main characteristic symptom of trigeminal neuralgia is paroxysmal pain. It comes suddenly and in its intensity and speed of spread resembles an electric shock. Typically, intense pain forces the patient to freeze in place, waiting for relief. The attack can last from a few seconds to 2-3 minutes, after which there is a period of calm. The next wave of pain may come within hours, days, weeks or months.
Over time, the duration of each attack of neuralgia increases, and periods of calm are reduced until a continuous aching pain develops.
The provoking factor is irritation of trigger points:
- lips;
- wings of the nose;
- eyebrow area;
- middle part of the chin;
- cheeks;
- area of the external auditory canal;
- oral cavity;
- temporomandibular joint.
A person often provokes an attack when performing hygiene procedures (combing hair, caring for the oral cavity), chewing, laughing, talking, yawning, etc.
Depending on the location of the lesion, the pain takes over:
- the upper half of the head, temple, orbit or nose if the ophthalmic branch of the nerve is affected;
- cheeks, lips, upper jaw – if the maxillary branch is affected;
- chin, lower jaw, as well as the area in front of the ear - with neuralgia of the mandibular branch.
If the lesion affects all three branches or the nerve itself before it is divided, the pain spreads to the entire corresponding half of the face.
Painful sensations are accompanied by other sensory disturbances: numbness, tingling or crawling sensations. Hyperacusis (increased hearing sensitivity) may be observed on the affected side.
Since the trigeminal nerve contains not only sensory, but also motor pathways for the transmission of impulses, with neuralgia the corresponding symptoms are observed:
- twitching of facial muscles;
- spasms of the muscles of the eyelids, masticatory muscles;
The third group of manifestations of neuralgia are trophic disorders. They are associated with a sharp deterioration in blood circulation and lymph outflow. The skin becomes dry, begins to peel, and wrinkles appear. Local graying and even hair loss in the affected area is observed. Not only the scalp suffers, but also the eyebrows and eyelashes. Impaired blood supply to the gums leads to the development of periodontal disease. At the time of the attack, the patient notes lacrimation and drooling, swelling of the facial tissues.
Constant spasms of muscle fibers on the diseased side lead to facial asymmetry: narrowing of the palpebral fissure, drooping of the upper eyelid and eyebrow, upward movement of the corner of the mouth on the healthy side or drooping on the diseased side.
The patient himself gradually becomes nervous and irritable, and often limits himself to food, since chewing can cause another attack.
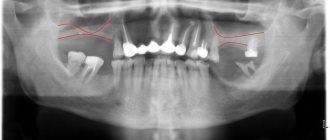
Characteristics of sinus lifting and bone grafting
Bone grafting in dentistry is designed to increase the volume of bone tissue to create suitable conditions for placing a dental implant. An increase in the volume of hard tissues can be carried out both through the use of one’s own bone material and with the use of synthetic substitutes. Bone grafting is performed on both the lower jaw and the upper jaw.
Sinus lifting is an operation performed exclusively on the upper jaw and, in essence, is a type of bone grafting. Its task is to raise the bottom of the maxillary sinus in order to increase the volume of bone mass. Additional bone material can be either your own or artificial. There are two ways to perform a sinus lift: open and closed. They differ in the complexity of execution and the ability to add different amounts of bone tissue.
Dental implant placement should not be confused with bone grafting or sinus lifting. These are two different operations, although they can be performed simultaneously. If there is initially a small amount of bone tissue, it may not be possible to place a dental implant immediately. Then, first, bone tissue is built up, and only a few months later, an artificial tooth is implanted.
Diagnostics
A neurologist diagnoses trigeminal neuralgia. During the first visit, he carefully interviews the patient to find out:
- complaints: nature of pain, its intensity and localization, conditions and frequency of attacks, their duration;
- medical history: when pain attacks first appeared, how they changed over time, etc.;
- life history: the presence of chronic diseases, previous injuries and operations is clarified, special attention is paid to dental diseases and interventions.
A basic examination includes assessing the condition of the skin and muscles, identifying asymmetry and other characteristic signs, checking the quality of reflexes and skin sensitivity.
To confirm the diagnosis, the following is carried out:
- MRI of the brain and spinal cord with or without contrast: allows you to identify tumors, consequences of injuries, vascular disorders; sometimes the study is replaced by computed tomography (CT), but it is not as informative;
- electroneurography: study of the speed of nerve impulse transmission through fibers; allows you to identify the fact of nerve damage, assess the level of the defect and its features;
- electroneuromyography: not only the speed of impulse passage along the nerve bundle is studied, but also the reaction of muscle fibers to it; allows you to assess nerve damage, as well as determine the sensitivity threshold of trigger zones;
- electroencephalography (EEG): assessment of the bioelectrical activity of the brain.
Laboratory diagnostics includes only general studies to exclude other causes of painful attacks, as well as to assess the condition of the body as a whole (usually a general blood and urine test is prescribed, as well as a standard set of biochemical blood tests). If the infectious nature of the disease is suspected, tests are carried out to identify specific pathogens or antibodies to them.
Additionally, consultations with specialized specialists are prescribed: ENT specialist (if there are signs of nasopharynx pathology), a neurosurgeon (if there are signs of a tumor or injury), and a dentist.
When your head hurts and your face goes numb
There may be several reasons for feeling unwell. And it is not always clear which doctor to contact with a particular ailment. Our expert will help you navigate. In order to get a complete answer, in the comments to this article you need to:
- briefly outline the main symptoms;
- make the question as specific as possible;
- write a question in the comments under this article.
You will find answers to your questions in the next issue of the section “What kind of doctor do I need?”
Question: I have a terrible headache, and part of my head and face go numb. The hand goes numb, there is not enough air.
Headache is one of the most common symptoms and includes all types of pain and discomfort in the head area. There are four main types of headaches:
- vascular headache occurs as a result of a mismatch between the resistance of the vascular wall and the increase in pulse volume of blood;
- headache of muscle tension: with prolonged tension or compression of the soft tissues of the head;
- liquorodynamic is associated with tension in the membranes of blood vessels (with an increase and decrease in intracranial pressure);
- neuralgic pain occurs when pressure is applied to trigger zones.
There are also mixed headaches with a combination of the main types and psychalgia, or hypochondriacal headache, which occurs with mental disorders.
All types of headaches differ in location and connection with physical activity.
You should also differentiate between headaches and migraines. Migraine is an intense headache, usually unilateral, pulsating in nature, lasts up to 72 hours, may be accompanied by nausea, vomiting, hypersensitivity to light, sounds, etc., intensifies with physical activity. Some patients may experience an aura in the form of a short-term visual disturbance preceding an attack of headache. Facial numbness may also occur both during the aura and at the peak of the headache.
The patient needs to consult a neurologist to identify the cause of the headache, determine treatment tactics and prevent possible serious consequences of the disease.
_____________________________________________________________________
Question: At night I have a cough, as if something is tickling or bothering me in my throat.
Coughing is a protective reflex. It helps clear the airways of excess mucus or foreign bodies. The moment a person coughs, air abruptly leaves the lungs, forcing out what is obstructing breathing.
Tickling and discomfort in the throat can be the body’s reaction to internal and external irritants. Here are the main reasons for the development of cough and throat discomfort:
- infectious diseases of the upper respiratory tract, both acute and chronic: pharyngitis, laryngitis, tonsillitis, rhinitis, etc.;
- allergic reactions: this can be a seasonal exacerbation; allergens can also be pet hair, house dust, household chemicals, bed mites, low-quality bedding, feather or down pillows and blankets, house plants;
- industrial aerosols (dust and gas contamination of atmospheric air);
- smoking;
- endocrine diseases: dryness of the oral mucosa in diabetes mellitus, formations of the thyroid gland, which can cause pressure on the larynx;
- diseases of the gastrointestinal tract with reflux of gastric contents into the esophagus, worsening in a horizontal position of the body, which is accompanied by heartburn, belching, bitterness in the mouth and a sore throat;
- autonomic disorders and neuroses after prolonged stress.
To determine the cause of a night cough and discomfort in the throat, you need to consult a general practitioner who, when collecting an anamnesis and examining the patient, will be able to determine the examination tactics and refer him to the necessary specialized specialists (otolaryngologist, allergist, endocrinologist, gastroenterologist, etc.).
_____________________________________________________________________
Question: Good afternoon. Fingers often go numb - the little and ring fingers on the right hand, sometimes they even turn blue, sometimes the whole palm turns blue. This also happens on the left hand, but less often. During sleep, the hands also turn blue, but completely, from the elbow to the tips of the fingers.
Blue discoloration of the upper or lower extremities is called peripheral cyanosis. Peripheral cyanosis (acrocyanosis) is associated with insufficient blood supply to small capillaries in areas of the skin distant from the heart. This disorder occurs due to narrowing of small capillaries and slow local blood circulation.
Peripheral cyanosis may be accompanied by cold hands and feet, and a feeling of numbness in the extremities. The causes of peripheral cyanosis may be:
- neurohormonal changes associated with the menstrual cycle;
- Raynaud's syndrome (secondary manifestation of a number of causes);
- diseases of the cardiovascular system;
- diseases of the bronchopulmonary system;
- low blood pressure;
- a number of systemic diseases;
- hypothermia, etc.
The patient needs to see a general practitioner, who, after collecting an anamnesis and examination, will be able to determine the examination tactics and refer him to the necessary specialists. In this case, a visit to a cardiologist, neurologist, rheumatologist, pulmonologist, etc. may be required.
occupational therapist, head of the hospital “Clinics for the whole family 1 + 1”
answered your questions Photo depositphotos.com The author’s opinion may not coincide with the opinion of the editors
Treatment of trigeminal neuralgia
Treatment is aimed at:
- to eliminate the cause of damage;
- to alleviate the patient's condition;
- to stimulate the restoration of nerve structures;
- to reduce the excitability of trigger zones.
Properly selected treatment can reduce the frequency, intensity and duration of pain waves, and ideally achieve stable remission.
Drug treatment
Trigeminal neuralgia requires complex treatment using drugs from several groups:
- anticonvulsants (carbamazepine and analogues): reduce the excitability of nerve fibers;
- muscle relaxants (baclofen, mydocalm): reduce muscle spasms, improve blood circulation, reduce pain;
- B vitamins (neuromultivit, milgamma): stimulate the restoration of nerve fibers, have an antidepressant effect;
- antihistamines (diphenhydramine): enhance the effect of anticonvulsants;
- sedatives and antidepressants (glycine, aminazine): stabilize the patient’s emotional state.
For severe pain, narcotic analgesics may be prescribed. Previously, drug blockades (injecting the problem area with anesthetics) were actively used, but today this method of treatment is almost never used. It contributes to additional damage to nerve fibers.
Treatment of the root cause of the disease is mandatory: elimination of dental problems, taking medications to improve cerebral circulation, etc.
Physiotherapy and other non-drug methods
Non-drug methods complement drug therapy well and help stabilize patients’ condition. Depending on the condition and concomitant diseases, the following may be prescribed:
- ultraviolet irradiation: inhibits the passage of impulses along nerve fibers, providing an analgesic effect;
- laser therapy: reduces pain;
- UHF therapy: improves microcirculation and prevents muscle atrophy;
- electrophoresis with analgesics or antispasmodics to relieve pain and relax muscles;
- diadynamic currents: reduce the conductivity of nerve fibers, significantly increase the intervals between attacks;
- massage of the face, head, cervical-collar area: improves blood circulation and lymph outflow, improving tissue nutrition; must be carried out with caution so as not to touch trigger zones and provoke an attack; the course is carried out only during the period of remission;
- acupuncture: helps relieve pain.
Surgery
The help of surgeons is indispensable when it is necessary to eliminate nerve compression. If indicated, the following is carried out:
- removal of tumors;
- displacement or removal of dilated vessels pressing on the nerve (microvascular decompression);
- expansion of the bone canals in which the branches of the nerve pass.
A number of operations are aimed at reducing nerve fiber conductivity:
- exposure to a gamma knife or cyber knife;
- balloon compression of the trigeminal node: compression of the node using an air-filled balloon installed in close proximity to it, followed by death of the nerve fibers; surgery often leads to partial loss of sensation and decreased muscle movement;
- resection of the trigeminal node: rarely performed due to the complexity and large number of complications.
Make an appointment
Treatment options
If the nerve trunk, plexus or branches of the nerve are damaged or compressed, there are two ways to solve the problem.
The first is to leave everything as is, without performing surgery. Such a solution to the problem is acceptable in case of incomplete loss of sensitivity or a small area of focus, with the exception of cases with displacement of the denture. Compression of the nerve due to regenerative processes will stop progressing after a certain point, “frozen” in one place. Odontogenic sinusitis can be treated with medication using antibiotics.
The second method is to perform surgery. The operation is indicated for injuries during sinus lifting and bone grafting, displacement of dentures or bone mass, extensive or complete loss of sensation. During the operation, the cause of the numbness is eliminated and, if necessary, the damaged nerve is sutured. Restoration of sensitivity takes a long time, sometimes never returning to its original state.
Complications
Without treatment, trigeminal neuralgia gradually progresses. Over time, a pathological pain focus forms in one of the parts of the brain. As a result, the pain covers the entire face, is provoked by any minor irritant and even the memory of an attack, and subsequently becomes permanent. Vegetative-trophic disorders progress:
- irreversible atrophy of the facial muscles is formed;
- teeth become loose and begin to fall out due to advanced periodontal disease;
- baldness is increasing.
Due to constant pain, the patient's sleep is disturbed and severe depression develops. In severe cases, patients may commit suicide.
Prevention
Prevention of trigeminal neuralgia is a set of simple measures that significantly reduce the risk of developing pathology. Doctors recommend:
- undergo regular preventive examinations;
- at the first signs of the disease, seek help (the sooner treatment is started, the greater its effect will be);
- eat right, get the required amount of vitamins, minerals, unsaturated fatty acids;
- regularly engage in light sports and gymnastics;
- get enough sleep and rest;
- minimize stress and physical overload;
- avoid hypothermia and harden yourself;
- to refuse from bad habits.
Treatment at the Energy of Health clinic
If you or your relative are bothered by severe pain in one or another part of the face, the neurologists of the Health Energy clinic will come to the rescue. We will conduct a full diagnosis to identify the causes of the pathology and prescribe comprehensive treatment. At your service:
- modern drug regimens to reduce the frequency and intensity of attacks;
- physiotherapeutic procedures: magnetotherapy, laser therapy, electrophoresis, phonophoresis, etc.;
- delicate therapeutic massage;
- acupuncture;
- help from a psychologist if necessary.
Left or right cheek goes numb: reasons not related to illness
Numbness of the face is not always associated with any pathology. Especially if episodes of sensory impairment are short-term and rare.
Parts of the face may become numb due to incorrect head position, prolonged sitting in an uncomfortable position, general hypothermia, or during periods of severe emotional shock. In these cases, there is no need to worry; numbness does not pose a danger to the human body.
Common causes of numbness that are not associated with illness:
- Incorrect work and rest schedule. Parts of the face may become numb if the head is in one position for a long time. For example, when working at a computer, reading, if breaks are not taken during work.
- Uncomfortable pillow. Uncomfortable head position during sleep can lead to compression of nerves and blood vessels. In the morning this will manifest itself in the form of numbness in different parts of the face.
- Panic attacks. The cheeks may become numb during panic attacks, during periods of severe shock. Numbness goes away along with other symptoms of nervous tension.
Advantages of the Health Energy Clinic
The Health Energy Clinic is a multidisciplinary medical center where every patient has access to:
- screening diagnostic programs aimed at early detection of diseases and pathologies;
- targeted diagnostics using modern equipment and laboratory tests;
- consultations with experienced specialists, including foreign ones;
- modern and effective comprehensive treatment;
- necessary certificates and extracts;
- documents and appointments for spa treatment.
Trigeminal neuralgia is a serious pathology that can seriously disrupt a person’s normal lifestyle. Don't let pain and fear take over your thoughts, get treatment at Health Energy.
Consequences of jaw spasm
Trismus is unpleasant for a person not only due to pain. When opening and closing the mouth is painful, the normal process of eating is disrupted and the gastrointestinal tract suffers. When the jaw spasms, breathing is impaired, which leads to constant oxygen starvation of the brain and headaches. This affects the composition of the blood and the functioning of the cardiovascular system.
Trismus caused by infections or tumors causes serious health problems. In this case, long-term serious treatment is required. In the initial stages, pain is completely relieved. For systemic diseases, when trismus is a secondary symptom, complex therapy is necessary.