Tonsil hyperplasia is a disease that is considered a childhood disease, in which pus collects in the folds of the mucous membrane of the tonsils, causing pathologies of the heart and/or kidneys.
- Causes of tonsil hyperplasia
- Symptoms
- Tonsil hyperplasia in children
- Diagnostics
- Treatment
- Prevention
- Forecast
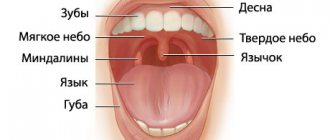
Tonsils are a collection of lymphatic tissue that is designed to protect the body and has several locations. During certain processes in the body, the tonsils cease to perform the function of immunity and help the infection to spread. When lymphatic tissue increases in quantity, the tonsils become larger. Because of this, the child can no longer breathe normally. Hypoxia develops, and with a lack of oxygen in the body, as is known, the brain suffers greatly. In such cases, the child’s development is disrupted and he often falls ill.
Tonsils can grow due to swelling caused by inflammation. Provocateurs may be allergic agents or infection. The third reason is true hyperplasia. From 3 to 6 years, enlargement of the tonsils is a normal physiological process. Tonsil hyperplasia can be caused by pathogens such as mycoplasma and chlamydia. Correct prescription of medications is important for treatment. Anti-inflammatory drugs are relevant to relieve inflammation and minimize swelling. Antibacterial drugs are needed to destroy the pathogen that caused the disease.
If drug treatment is ineffective, the doctor prescribes a surgical operation called adenotomy. After this, you need to take immunostimulants for prevention. For the first degree of hyperplasia, surgery is not required.
Causes of tonsil hyperplasia
For the occurrence of the disease, a damaging factor, for example, a burn, is important. In such situations, not only the tonsils are affected, but also the tissues adjacent to them. Not only too hot water, but also alkaline and acidic substances can damage the tonsils. For treatment of such patients, hospitalization is mandatory.
Among the reasons are the impact of a third-party object. Most likely these are small fish bones that violate the integrity of the lymphatic tissue. When swallowing, a person in such cases feels as if something is stabbing in his throat. The next reason is tumors and abnormal development of the tonsils. An organ can also be damaged if:
- contact with infected mucus (adenoiditis)
- mouth breathing, resulting in prolonged inhalation of cold air
- diseases to which the child was exposed at a young age
- relapses and frequent diseases of the ears, throat and/or nose.
The following children are at risk for tonsil hyperplasia:
- malnourished
- with poor living conditions, without proper care from parents or guardians
- imbalance of hormones in the body
- lymphatic-hypoplastic constitutional anomaly plays a role
- exposure to radiation for a long time
- lack of vitamins
Activation of the production of lymphoid cells plays a role in pathogenesis.
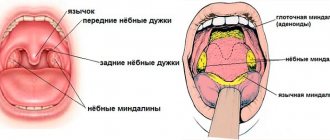
Localization and type of lingual tonsils
The lingual tonsil can be singular or paired
The lingual tonsil is located under the surface of the back of the tongue. It is a formation of lymphoid tissue in which the process of maturation of immune cells and the production of antibodies occurs.
Despite the fact that it is designated as an unpaired organ, most people have two such tonsils. This is explained by the symmetrical division of the organ’s lymphoid tissue into two parts.
The lingual tonsil in the photo is determined by an accumulation of lymphoid tissue consisting of follicles, so its structure appears heterogeneous. To determine how many lingual tonsils a person has, it is enough to carefully examine the groove at the base of the tongue. If it is very clear and noticeable, it means that the lymphoid tissue is divided into two organs and two tonsils. Interestingly, this division is not a pathology.
The anatomy of the lingual tonsil is simple. Having figured out where the lingual or uvular tonsil is located, you should understand the functions that this organ performs. Along with the palatine tonsils, the lingual tonsil is an organ of the immune system, acting as a barrier to germs and viruses that enter the body through the mouth. When there is a threat of penetration of pathogenic microorganisms, immune cells are formed and released in this tonsil, designed to protect against the disease.
Symptoms
For effective treatment, parents must notice the pathology in time and come to the doctor with this problem. Timely diagnosis is a guarantee that there will be no complications. Doctors often record hypertrophic processes in several types of tonsils, including the pharyngeal tonsil. The doctor must palpate the tonsils; the consistency is soft or tightly elastic to the touch. The shade can be either light yellow or rich red.
The child may complain of difficulty inhaling and exhaling, as well as discomfort when swallowing. Breathing becomes noisy, the doctor records dysphagia (swallowing disorder) and dysphonia (voice disorder). Parents may characterize the little patient’s voice as nasal, his speech as unintelligible, and some of the words may not be pronounced entirely correctly by the patient.
As already noted, tonsil hyperplasia leads to hypoxia - the body does not receive enough oxygen. As a result, coughing and snoring may occur during sleep. If the pathological process involves the child’s ears, then the doctor notes otitis media.
Complications can be constant colds, because a child with hyperplasia cannot breathe normally and keeps his mouth open. Otitis media (the above-mentioned complication) causes persistent hearing loss.
Hyperplasia of the palatine tonsils
There is no inflammation, but lymph tissue growth is observed mainly in young children. Hyperplasia of the palatine tonsils in such cases acts as a compensation mechanism when the body is attacked by infections. When the tonsils become so large that they become an obstacle to the inhalation of air and its passage through the respiratory tract, surgery is performed to remove some of the tissue.
Pathogenesis involves an immunoreactive process. Breathing through the mouth is also important if the child has a problem such as adenoids. They contribute to the production of large amounts of infected mucus, which negatively affects the tonsils. Pathologies of the adrenal glands or thyroid gland play a role in pathogenesis. Apnea is likely to occur at night.
Hyperplasia of the lingual tonsil
This tonsil is located at the root of the tongue. From the age of fourteen, it develops back and therefore splits in two. When this process is disrupted, lymphatic tissue grows. With hyperplasia of the lingual tonsil, a teenager complains of a foreign body in the throat. This process can accompany the patient until he turns 40 years old. The cause is most often congenital. The patient's swallowing worsens, the timbre of his voice changes, and relatives may notice periods of time when the patient does not breathe at night, which is called apnea.
When a child is diagnosed with hyperplasia of the palatine tonsil, during physical exercise, breathing becomes bubbling and noisy. A symptom such as cough is likely to cause laryngospasm. Taking pills will not work; the cough will continue for years. In some cases, the cough can be prolonged and severe, leading to bleeding.
Hyperplasia of the nasopharyngeal tonsil
Researchers put forward the point of view that the nasopharyngeal tonsils play a role in immunity until the baby is 3 years old. Due to frequent childhood illnesses, pathological growth of lymph tissue may begin. The disease is typical for children living in cold or excessively damp rooms. Inflammation appears in the respiratory organs.
Tonsils can be of three degrees of growth. The first degree is characterized by the adenoids covering the top of the plate that forms the nasal septum. If this plate is closed by 65%, the doctor records degree II; closure by 90% or more indicates stage II of the pathology in question.
Symptoms: nasal congestion, significant “snot”, which is why nasal passage is very poor. Due to these factors, blood circulation in the nasal cavity is impaired, which aggravates inflammation in the nasopharynx. If the adenoids are of the second or third degree, then the voice is impaired and is characterized as deaf. The auditory tubes may be closed, in such cases, which is logical, hearing decreases to a greater or lesser extent. The child’s mouth may be slightly open, sometimes the lower jaw may sag, the nasolabial folds may smooth out, which changes facial features.
Hyperplasia of the pharyngeal tonsil
This amygdala develops before the age of 14, with a particularly rapid rate of development in infants. Hyperplasia of the pharyngeal tonsil is one of the manifestations of lymphatic diathesis. Hereditary factors, regular hypothermia of the body, lack of nutrients or calories in the diet, and attack by viral pathogens may also play a role.
In some cases, chronic inflammatory processes in the tonsils cause excessive growth of their tissue. It is difficult for the patient to breathe through his nose, so he opens his mouth to inhale and exhale air. The upper lip is higher than the normal level, swelling of the face and some elongation are observed. Therefore, the doctor may mistakenly suspect mental retardation.
The brain does not have enough air. In the morning the child looks as if he did not get enough sleep. During the day he can be unreasonably capricious. Dryness of the oral mucosa is typical, the voice is hoarse when the child tries to breathe through the mouth. Long-term rhinitis with sinusitis is also recorded; tubotympanitis and otitis are likely. The temperature may be slightly increased, appetite worsens, memory and attention also become worse.
Adenoids treated or removed
The most common pathology in children is enlargement of the nasopharyngeal tonsil (adenoid vegetations, adenoids). According to various authors, the presence of adenoids is noted in children under 14 years of age from 5 to 45% of cases .
adenoids
Adenoids are located in the vault of the nasopharynx, where the nasal cavity ends, serving as a natural filter that prevents viral and bacterial agents from entering the lower parts of the respiratory system - the trachea and bronchi. In children, during the inflammatory process in the adenoids (local fight against viral or microbial agents in the tissue of the nasopharyngeal tonsil), difficulty in nasal breathing may be observed due to the fact that the tissue closes the lumen of the nasal cavity at the back, thereby interfering with the normal passage of air, the presence of mucous discharge in the anterior parts of the nasal cavity, snoring. Children experience a “choking” type cough due to secretions getting from the nasopharynx onto the vocal cords.
Cough is not always associated with adenoiditis (inflammation of the adenoids). Often, a cough is associated with one or another problem in the lower parts of the respiratory system (tracheitis, bronchitis, pneumonia, childhood infections). To exclude this pathology, the child must be consulted with a pediatrician, who will perform auscultation (listen to organ sounds), giving a conclusion about the presence or absence of pathology.
Due to the specific location of the adenoids, it is impossible to apply ointment, apply sprays, or use rinses; because of this, adenoids take a relatively long time to be treated.
Tonsil hyperplasia in children
The child's body is often exposed to infections, such as whooping cough or scarlet fever. Hypertrophic processes are launched as compensatory ones. The diagnosis in question is made mainly to children under the age of ten years. Hyperplasia does not manifest itself as an inflammatory process. The tonsils are pale yellow in color, they are not red.
With the 1st degree of proliferation there are no symptoms. If growth is intense, then parents note a nasal voice of the child, breathing complications and other symptoms that were listed above. A large number of follicles, which are more fragile than normal, close the gaps without plugs.
external reference
- Photos at usc.edu (Registration required)
- Anatomical atlases - Microscopic anatomy, plate 09.163
- Histology Image: 09802loa - Boston University Histology Training System
- MedEd at Loyola (labeled "lymphoid tissue")]
- Lingual tonsil
Anatomy of the mouth | |
| Lip |
|
| Cheek |
|
| Sky |
|
| Gums |
|
| Glands |
|
| Teeth |
|
| Language |
|
| Back of the mouth |
|
Organs lymphatic system | |
| Primary organs | |
| Thymus |
|
| Tonsils |
|
| Lymph node |
|
| MALT |
|
- Anatomical portal
Diagnostics
An experienced doctor pays attention to the facial expression of a small patient. It is important to interview parents, and, if possible, the child himself, to identify the main complaints. The history may indicate such points as low immune defense of the body, respiratory diseases (several per year), and a stuffy nose for a long time. Laboratory tests are important to determine the diagnosis. It is necessary to identify the pathogen and check its response to commonly used medications. The patient is prescribed bacterial culture from the throat.
The patient's blood must be taken for analysis, including acid-base balance, and urine must be taken for analysis to detect inflammation. Instrumental diagnostic methods are also relevant when diagnosing tonsil hyperplasia. Ultrasound diagnostics of the pharynx, pharyngoscopy, fibroendoscopy and rigid endoscopy are performed.
Tonsil hyperplasia can be caused (must be taken into account when diagnosing):
- cancer in the tonsils
- tuberculosis
- granulomas of the pharynx of an infectious nature
- leukemia
- lymphogranulomatosis
Structure
Microanatomy
The lingual tonsils are covered on the outside with stratified squamous non-keratinized epithelium, which invaginates inward, forming crypts. Under the epithelium there is a layer of lymphoid nodules containing lymphocytes. The mucous glands located at the root of the tongue drain through several ducts into the crypt of the lingual tonsils.[2][3] The secretions of these mucous glands keep the crypt clean and free of debris.
Blood supply
The lingual tonsils are located on the back surface of the tongue, through which they receive:[1]
- Lingual artery, branch of the external carotid artery
- Tonsillar branch of the facial artery
- Ascending and descending palatine arteries
- Ascending pharyngeal branch of the external carotid artery
Nervous nutrition
The lingual tonsils are innervated by the tonsils from the tonsil plexus, formed by the glossopharyngeal and vagus nerves.[1]
Treatment
Treatment requires a comprehensive approach, including the use of medications, physical therapy and, if necessary, surgery. In grade I (classification described above), special medications and rinses are prescribed. For the latter procedure, cauterizing and astringent agents are suitable, including a tannin solution; Antiseptics are also prescribed.
Hypertrophied areas are lubricated with a 2.5% solution of silver nitrate. The following medications are suitable for treatment:
- tonsilgon
- tonsilotren
- umkalor
- lymphomyosot
Topical physiotherapy techniques include:
- ultrasound
- ozone
- Microwave
- UHF
In some cases, endopharyngeal therapy with laser is needed. Mud ultraphonophoresis, electrophoresis, inhalation with decoctions of medicinal herbs, and vacuum hydrotherapy are often prescribed. In cases of II and III degrees of hyperplasia, surgical operations are resorted to. Most often, part of the overgrown tonsil is removed. This method is relevant for patients under seven years of age, if there is no polio, diphtheria, infectious diseases, or blood diseases.
Cryosurgery is a method of treating tonsil hyperplasia, in which the organ is affected by low temperatures, which allows you to get rid of pathological growths. In this case, the patient does not feel pain, and there is no blood either. This operation is indicated for patients with heart failure, atherosclerosis and heart defects.
The next method of treating the pathology in question is diathermocoagulation, in other words, cauterization. When agreeing to treatment with this method, consult your doctor about the high likelihood of various complications.
Treatment methods
If you feel discomfort in your throat and do not notice the symptoms of typical tonsillitis, you should consult a doctor as soon as possible. The doctor will be able to examine the patient’s throat in detail and make a diagnosis. Additionally, blood tests and a throat swab may be required.
Based on the examination results, the doctor selects a treatment regimen. For inflammation of the tonsil, conservative therapy is practiced; for hypertrophy, surgical therapy is used.
Drug treatment
The tablet is taken both before and after meals (it is recommended to take it with plenty of water)
Treatment begins with determining the cause of the disease. Both inflammation and hypertrophy are initially treated in the same way. Therapy consists of:
- antiseptic gargles;
- taking antipyretic and painkillers;
- antiviral, antifungal or antibacterial therapy.
A throat swab and blood test can determine the causative agent of the disease. For bacterial infections, broad-spectrum antibiotics are prescribed. They should be taken according to the doctor's recommendations; self-medication is unacceptable.
If the disease is viral in nature, for example, human papillomavirus or herpes, the drugs Acyclovir, Zovirax and their analogues are prescribed. These medications stop the activity of the virus and boost the immune system, helping it fight the disease.
Fungal infection of the lingual tonsil is quite rare, but such a disease can be completely excluded only after tests. If the cause is a fungal infection, the drugs Fluconazole, Itraconazole or Nystatin tablets are prescribed.
Additionally, it is necessary to provide antiseptic protection for the throat, otherwise the infection will quickly spread to neighboring organs. To do this, use rinses:
- Chlorhexidine;
- Miramistin;
- Chlorophylliptom;
- soda or salt;
- iodine solution;
- Lugol's solution;
- chamomile or calendula.
You can also treat the throat with an antiseptic spray; the medicine is also applied to the upper pole of the sublingual tonsil. This can cause a gag reflex, so treatment of the tonsils is carried out carefully.
Recommended sprays:
- Givalex;
- Inhalipt;
- Hexoral;
- Angilex.
Such drugs do not treat hypertrophy or inflammation, but prevent the development of complications and speed up recovery when taking antibiotics or other medications prescribed by a doctor.
To reduce tissue swelling, the doctor may recommend antihistamines, for example, Suprastin. Taking allergy pills will reduce swelling and make breathing easier.
During the inflammatory process, immunostimulants are additionally prescribed, for example, Lavomax or Arbidol.
For chronic inflammation, physical therapy techniques can be used to speed up tissue repair. As with tonsillitis, preference is given to UV irradiation (Solnyshko apparatus) or exposure to infrared rays.
Surgery
Enlargement of the lingual tonsil cannot be ignored
Removal of the lingual tonsil is indicated for severe tissue hypertrophy, suspected cancer, or chronic inflammatory process. Also, bacterial inflammation can develop into an abscess, which requires urgent surgical treatment.
Knowing where the lingual tonsil is located, it becomes clear that it is located in a place where a large number of blood vessels accumulate, so surgery is associated with the risk of bleeding.
The operation is performed under local or general anesthesia. The doctor excises the enlarged tonsil with a scalpel, then stops the bleeding and applies antiseptic and wound-healing agents to the area. Surgery to remove this tonsil carries a risk of wound infection, since the lingual tonsil is located in an area that is easily injured when eating, so antibiotics must be taken before and after the procedure.
After the operation, the patient experiences severe pain for several days, which gradually subsides. Rehabilitation takes an average of 2 weeks. In the first week after the operation, the diet changes radically; the patient will only eat pureed food at room temperature, so as not to injure the wound.
Prevention
It is important to live in favorable conditions, keeping the room clean, maintaining a normal level of air humidity and a temperature comfortable for the human body. Nutrition must be correct for the immune system to be active. In autumn and winter, you need to dress according to the weather, not breathe through your mouth, so that the tonsils are not exposed to icy air.
To maintain immunity, hardening, spa treatment, and additional courses of minerals and vitamins may be important. Respiratory and any other diseases must be treated on time so that they do not become chronic.
Inflammation of the lingual tonsil
The disease can appear if you are very cold
The cause of inflammation of the lingual tonsil in the vast majority of cases are staphylococci and streptococci. As is known, these same pathogens provoke acute tonsillitis. In the vast majority of cases, the development of inflammation of the lingual tonsil is caused by a decrease in general and local immunity. The fact is that strong immune defense successfully copes with opportunistic bacteria, which are staphylococci.
The inflammatory process is indirectly related to chronic tonsillitis, since this disease provokes a decrease in local immunity, putting the remaining tonsils at risk.
Factors that provoke inflammation:
- decreased immunity;
- hypothermia;
- smoking;
- tonsil hypertrophy;
- glossitis;
- chronic source of infection.
Glossitis is an inflammation of the tongue. As with hypertrophy, the cause of inflammation of the lingual tonsil is often smoking, since nicotine and tobacco smoke reduce local immunity, increasing the risk of developing ENT diseases.
Interesting! Hypertrophy can be both the cause of inflammation of the lingual tonsil, and a consequence of this phenomenon, if the inflammatory process becomes chronic.
Contrary to popular belief, it is mainly adults who experience inflammation of the lingual tonsil; the disease is rarely diagnosed in children.
Symptoms of inflammation
Inflammation of the lingual tonsil is a disease that is difficult to distinguish from a photo, since it can inflame part of the tongue, the larynx and the palatine tonsils. The specific structure and anatomy of the lingual tonsil does not allow one to visually determine this disease independently. Everything is complicated by the symptoms of inflammation, which are characteristic of tonsillitis and pharyngitis. Signs of the disease:
- rawness and sore throat;
- redness of the throat and part of the tongue;
- swelling of the laryngeal tissues;
- pain when swallowing;
- foreign body sensation;
- white coating on the tongue and tonsils;
- enlarged lymph nodes under the jaw;
- increased body temperature;
- symptoms of intoxication.
In the absence of timely treatment, swelling of the epiglottis and swelling of the upper pole of the lingual tonsil appear. This is dangerous for breathing problems, even suffocation.
Quite often, when the lingual tonsil is inflamed, the palatine tonsils hurt, which is explained by the spread of infection throughout all vulnerable organs located in the affected area.
Forecast
Doctors almost always give a favorable prognosis. Thanks to tonsillotomy, a person can breathe through his nose, and his immunity returns to normal. The brain functions without hypoxia, which normalizes the patient’s sleep and general well-being. Nasal voice also disappears after proper treatment. At an early age, moderate hyperplasia of the tonsils can be detected, but after the child reaches ten years of age, it goes away. If after 10 years hyperplasia still exists, you need to consult a doctor.
If symptoms appear, consult a doctor for early diagnosis and treatment.
Tumor of the tonsils: prevention
There are no specific methods of prevention as such. General measures aimed at preventing neoplasia include:
- Adequate oral hygiene.
- Quit smoking and abusing alcoholic beverages, especially low quality ones.
- Regular examination of the oral cavity by a dentist for the presence of papillomas, their treatment if detected.
- Minimizing contact with carcinogens.
- A balanced diet containing physiological norms of food nutrients with the exception of products with food additives and GMOs.
A general high level of suspicion regarding cancer is also important, which contributes to earlier seeking advice from specialists in cases of early adverse symptoms. Don't search for information on how to identify tonsil cancer on your own.
2. Reasons
The connection between hypertrophy of the tonsils and frequent acute respiratory viral infections, tonsillitis, laryngitis and other infectious and inflammatory diseases of the ENT organs has been reliably established. In addition, many sources indicate a higher frequency of such hypertrophies in children with weakened immunity, regardless of the reasons. Finally, a combination of hypertrophied tonsils with adenoids is constantly encountered - a hyperplastic growth of another tonsil, the nasopharyngeal; according to a number of experts, this indicates the commonality of hyperplastic and hypertrophic processes for the entire lymphadenoid ring.
Hence the conclusion is drawn about the compensatory, reactive nature of hypertrophy of the tonsils: in this case, organs that are very often and intensively used and/or cannot cope (with weakened local and general immunity) with their functions increase.
However, the etiopathogenesis of tonsil hypertrophy still remains controversial and is being actively studied by specialists in this field.
Risk factors usually include hypovitaminosis, insufficient and unbalanced nutrition, harmful environmental factors, and endocrine disorders.
Visit our Otolaryngology (ENT) page