Dental modeling is a set of manipulations to prepare for the installation of orthopedic structures. Used to visually demonstrate the potential appearance of an artificial smile model and check the comfort of wearing a denture. At this stage, the doctor reproduces with wax the external aesthetic shape of the complete dentition and individual units.
The second name for modeling is the Wax-up technique. It is carried out during dentures and implantation by taking a personal impression of the oral cavity.
The wax sample is used as a base for the production of a permanent orthopedic product. To obtain an ideal impression, carious and destroyed units are reconstructed with liquid wax. The technician begins further manipulations after the composition has completely hardened. The specialist determines the accuracy of the connection between the created model and the tooth and determines the correct distribution of the chewing load.
There should be no pain during fitting. After receiving data on the anatomical structure of the visitor’s dental system, the physician determines the tactics of further treatment and begins restoration.
Features of the procedure
Wax-up for aesthetic restoration is popular among orthopedists. Wax is a malleable compound that can be molded. With its help, an accurate impression of the tooth is created, taking into account the anatomical features.
The accuracy of manipulation affects the comfort of the artificial prosthesis. Following the technology will relieve the patient from pain when talking and eating.
The Wax-up technique is safe and does not cause discomfort. This is due to the absence of violation of the integrity of the oral mucosa. There is a risk of cross-reaction in those who suffer from allergic reactions to bee products. In this case, replace the composition.
Short or overactive upper lip
If a patient with excessive visualization of the maxillary gums has a short upper lip (compared to the norm) (Fig. 4 and 5), then this is most likely the cause of aesthetic imbalances. If the length of the facial contour, gums, lips and central incisors is normal, then in a patient with excessive visualization of gingival tissue, the likely cause of this condition will be an overactive upper lip. In young women, with a calm state of the facial muscles, 3-4 mm of the central incisors of the upper jaw are usually visualized, and with a wide smile, the crown of the teeth 10-11 mm long is completely visible. Accordingly, the upper lip should usually rise 6-8 mm during the transition from a relaxed state of the facial muscles to a wide smile. However, in a patient with a hyperactive upper lip, these parameters may be 1.5-2 times higher. At the moment, there are no methods for dental correction of a short or overactive upper lip, however, plastic surgery is possible. However, it is important to make this diagnosis when planning restorative treatment of anterior teeth. The patient should be informed that treatment may not only fail to correct, but may even worsen excessive gingival visualization.
Purpose of application
The need for Wax-up is due to the following factors:
- Reproduction of dental units from wax is the starting stage of restoration work. It is required for planning future work of dentists. Wax impressions help to track the individual characteristics of the structure of teeth and avoid errors during implantation.
- Calculation of the cost of upcoming dental procedures.
- Temporary prosthetics. The specialist takes samples for the production of intermediate prosthetic restorations made of plastic. The technology is used when additional time is needed to create fixed prostheses.
Change in passive protrusion
The presence of short maxillary central incisors (less than 9 mm) can result from several factors (eg, normal variation, wear of the incisal edge, excess gingival coverage). Although cases of insufficient height of the central incisors do occur, it is quite rare. A more common cause is abrasion of the cutting edge. To determine the degree of tooth wear, it is necessary to measure the distance between the cemento-enamel junction (CEJ) and the cutting edge of the incisor, which is normally 10-11 mm for central incisors. Thus, the degree of abrasion of the incisors is determined relative to the average value of this indicator. Another method is wax modeling of a worn incisor on a diagnostic model using wax, when the ideal contour of the incisors is restored, after which the height of the added wax is measured.
The reason for the decrease in the clinical height of the crown may also be its excessive gum coverage. Since the most common etiology of this condition is gingival hyperplasia, the gum itself and its contours rarely look normal. When the gums appear healthy and the reduction in crown length of the central incisors cannot be explained by wear of the incisor edge alone, it is most likely due to alteration of passive protrusion.[4] During the normal process of teething, the central incisors of the upper jaw pass through the gum and continue to actively grow until they come into contact with the opposing teeth. At the eruption stage, a significant part of the anatomical crown remains covered by the gum. With age, the anatomical crown becomes increasingly visible due to apical migration of the gums. This process, called passive protrusion, continues during adolescence until the gingival margin is located 1-2 mm from the CEJ. For reasons still unknown, in some patients the process of normal passive protrusion stops. This results in the formation of a short clinical crown due to excess gingival coverage. This condition is called “alteration of passive protrusion” or “delay of passive protrusion” (Fig. 6 to 9).[13] Although, according to Volchansky and Cleaton-Jones, the level of the gingival margin of the maxillary central incisors is relatively stabilized by 12 years of age,14 it would be premature to make a diagnosis of alteration of passive protrusion until the patient has completed growth. To diagnose alteration of passive protrusion, the tip of the instrument is inserted under the gingival margin to determine the CEJ. If it is possible to determine the level of the CEJ, then a decrease in crown height can be considered a variant of the norm, erasure of the incisor edge, or a combination of both. If the CEJ cannot be determined, it is most likely hidden by adjacent tissues and then the diagnosis of alteration of protrusion is obvious.
Rice. from 6 to 9 Since the treatment of alteration of passive protrusion includes surgical lengthening of the coronal part of the tooth,[1,4,15] it is necessary to conduct additional diagnostic studies to carry out adequate intervention. Under local anesthesia, the position of the alveolar ridge is determined. A periodontal probe is placed in the sulcus and advanced until it contacts the alveolar ridge. The distance from the gingival margin to the bone crest is approximately 3 mm,[16,17] and is called the “biological width” (BW) (Fig. 10).[18]
Figure 10. Biological width. Note the position of the adjacent connective tissue, epithelium, and gingival margin in relation to the alveolar bone margin.
After determining the position of the edge of the alveolar ridge, the area of the attached gum is measured. The periodontal probe is pressed against the mucosa in the projection of the corresponding tooth perpendicular to the longitudinal axis of the teeth. The probe is moved towards the crown until a fold appears in the area of the mucogingival junction (GJ). Thus, the distance from the SDS to the gum edge is determined. To determine the zone of attached gingiva, the value of the zone of free gingiva, measured from the gingival margin to the base of the pocket, is subtracted from the total value of keratinized gingiva.
After assessing the attached gingival zone and biological width, the preferred method of surgical treatment can be selected. A healthy gum requires a biological width of at least 3 mm. Thus, if a patient has a SB of 4 mm, then 1 mm can be removed with gingivectomy. Before any surgical procedure begins, the dentist must ensure that there is an adequate amount of gum remaining (3 mm) after the operation. For example, if there is 1 mm of excess gingival excision and the presence of normal bone and gingival parameters, the soft tissue gradually regenerates until a distance of 3 mm is restored between the gingival margin and the edge of the alveolar bone crest.
SB with alteration of passive protrusion is often 3 mm. The gum removed during gingivoplasty or gingivectomy gradually regenerates in its original place until it reaches normal biological length. In such cases, more attention must be paid to the underlying bone. The mucoperiosteal flap is folded back to visualize the bony ridge, which is usually adjacent to or even fused with the CEJ. Since there is no biological indication for removing interproximal bone, the flap does not involve the interdental papillae. Using high-speed tips and chisels, bone tissue is removed until a distance of 2-2.5 mm is reached from the CEJ to the edge of the alveolar ridge (Fig. 11).
Rice. 11 The distal size of the flap depends on the amount of gingiva visualized with a wide smile. The size of the flap usually extends to the mesial border of the first molars. After completion of the ostectomy, the flap is adapted (slightly coronal to the CEJ) and sutured. Using a periodontal probe inserted under the flap, measure the distance from the gum edge to the edge of the alveolar ridge, which should be approximately 3 mm. After suturing, minor reconstruction of the gingival contour can be performed using electrosurgical instruments to achieve complete symmetry. When a good relationship between bone and adjacent gingiva can be achieved, healing occurs with minimal coronal or apical gingival displacement (Figures 12 to 14). However, it is often necessary to perform additional minor soft tissue reconstruction 6 weeks after surgery.
Rice. from 12 to 14
Indications and contraindications
The orthodontist prescribes dental diagnostics after a clinical examination if there are indications:
- Abrasion of units due to malocclusion and other pathologies.
- Destruction of the supragingival area due to advanced forms of caries.
- Distinctive color.
- All that remains of the units is the root base.
- Edentia.
- Multiple pathologies.
Contraindications:
- dental pathologies in acute form;
- recovery after radiation therapy;
- drug addiction;
- diseases of the jaw tissue;
- inflammation of various etiologies.
Modeling methods
Dentists use two methods of diagnostic modeling.
- Indirect
This technique is based on modeling a plaster model. Does not require prolonged presence of the visitor in the clinic. The orthodontist takes an impression of the oral cavity and passes it on to the technician to form the structure in the laboratory.
Precise finishing of the sample edges is carried out for user comfort. This method is chosen by the dentist to work with teeth located in hard-to-reach places.
- Straight
It is a combination of two technologies - Wax-up and Mock-up. Modeling is carried out directly in the patient’s mouth. Suitable for working on single structures.
The specialist fills the tooth cavity with liquid wax or a plastic mass. Reproduction and pinning are then performed, after which the resulting model is retrieved. Based on the resulting layout, a composite sample is created.
A person walks with the installed temporary system for a short time to evaluate its convenience and correct manufacture. The method is suitable for people who want to improve their bite or suffer from increased enamel wear.
Material characteristics
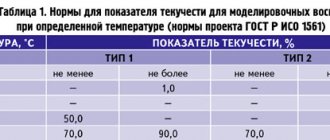
When carrying out the procedure, two types of beeswax are used:
- 1 type Found application in direct modeling.
- Type 2 Used with indirect technology. The wax is of lower quality, but the result of the work is at a decent level.
Recommendations must be followed when selecting, storing and using the material:
- the use of colored waxes allows you to achieve clear contrast;
- the frozen forming composition is rigid and does not crumble;
- absence of crumbs and impurities in the heated mass;
- absence of chips and cracks when scraping;
- compliance with storage periods;
- competent selection of the type of material depending on the technique;
- selection of soft types of material.
Preparatory stage
Before starting to reproduce the dentition, the following recommendations are followed:
- inspection is carried out;
- CT and X-ray diagnostics of the jaw are performed;
- treatment of dental diseases;
- compliance with hygiene rules, sanitation of the oral cavity.
The manipulation is carried out after a full examination and dental therapy.
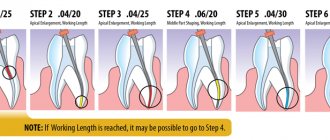
Step-by-step algorithm
Stages of the procedure:
- taking a plaster (silicone) impression of the patient’s jaw at the site of future placement and on the opposite side;
- preventing jaw closure using silicone bite pads;
- determining the relationship between the upper jaw and the skull using a facebow;
- transferring samples onto a gypsum base;
- fixing the model on the articulator;
- modeling a wax cast on plaster models;
- Demonstration of the layout to the client.
The Mock-up technique involves transferring the mock-up to the mouth. Algorithm of the doctor’s actions:
- obtaining silicone keys;
- gentle removal of deposits;
- fixing the layout with special glue;
- placing composite or polyurethane into impressions, fixation;
- impression taking, grinding and polishing;
- assessment of work quality.
The duration of making a model depends on the specific structure and development of the jaw and location.
Pros and cons
Making wax models is a painstaking and technologically complex process. The popularity of the procedure among dental technicians and orthodontists is due to its advantages:
- adjustment of nuances;
- no need to get used to wearing permanent orthopedic structures;
- absence of discomfort, pain;
- gentle preparation process;
- patient participation in the process of adjusting the model using the indirect method.
The disadvantages include reduced accuracy with the indirect method. The volume of the material changes as it hardens.
Diagnosis
To make a correct diagnosis, the doctor needs knowledge in the field of facial aesthetics. The main evaluation parameter is the height of the facial oval. When the facial muscles are relaxed, the height of the middle part of the face should be equal to the height of the lower part (Fig. 1).[9] The anatomical landmarks of the midsection are the glabella, the most prominent point of the frontal bone between the brow ridges, and the inferior point of the nasal septum. The lower part is measured from the lowest point of the nasal septum to the lowest point of the soft tissues of the lower jaw, i.e. lower edge of the chin.
Figure 1. The height of the middle third of the face, measured from the bridge of the nose to the lower edge of the nasal septum, should be equal to the height of the lower third of the face, measured from the lower edge of the nasal septum to the lower edge of the chin.
After assessing facial height, it is necessary to determine the length of the upper lip. When measured in a relaxed state of the facial muscles from the lower point of the nasal septum to the lower edge of the lip, the average length of the upper lip in young women and men is 20-22 mm and 22-24 mm, respectively.[10] In a calm state of the facial muscles in young women, 3-4 mm of the central incisors of the upper jaw are usually visualized (Fig. 2), the same figure in men of the same age is 2 mm less.[11] With age, there is a tendency for the upper lip to lengthen. Therefore, the upper incisors are visualized less, and the lower incisors become more “open” in a calm state of the facial muscles. When the patient smiles broadly, the upper lip should move towards the dentogingival junction of the maxillary central and lateral incisors (Fig. 3). When more than 1.5-2 mm of gum is exposed, an unfavorable aesthetic effect occurs.
With a wide smile, the cutting edge of the upper jaw teeth should run parallel to the curve of the lower lip and lightly touch it (but not be covered by it) (Fig. 3). When the cutting edge does not come into contact with the lower lip when smiling, the result is a negative aesthetic effect. Lastly, when conducting a clinical analysis, the length of the crowns of the central incisors of the upper jaw is assessed, which is usually 10-11 mm.[12] Using the data obtained, it is possible to determine the cause of excessive visualization of the gums in each individual patient.
Combination of several etiological factors
Quite often in patients with excessive gingival visualization, this condition occurs as a result of several factors. Although this complicates treatment planning, the presence of multiple etiological factors is not a serious obstacle when using the diagnostic methods described above. For example, alteration of passive protrusion is often observed in patients with a high upper jaw. In this case, a gingivectomy is first performed to create the optimal length of the clinical crown. Diagnosis can then begin using radiography, simulation and dynamic facial assessment. This study should include determining the position of the incisal edge of the upper jaw teeth (in a calm state of the facial muscles and with a wide smile), the appearance of the frontal teeth of the upper jaw (in a calm state of the facial muscles and with a wide smile) and the position of the upper lip line with a wide smile. Once a diagnosis is made, an appropriate treatment plan can be formulated and implemented using orthodontic correction and maxillofacial (orthognathic) surgery.
Dento-alveolar extrusion
Dento-alveolar extrusion is the excessive eruption of one or more teeth in the frontal group of the upper jaw. This condition mainly occurs in cases of lack of adequate opposing occlusion and is most often observed in patients with class 2 occlusion pathology. With the growth of the incisors of the upper jaw, the corresponding section of the alveolar process moves down along with the teeth. In patients with correct aesthetic proportions, an imaginary line connecting the maxillary canine fossae should pass through the periodontal line of the maxillary central incisors. In the case of dento-alveolar extrusion, the incisors lengthen, which leads to displacement of the gums and the underlying bone. In this case, the imaginary line passing along the dentogingival junction becomes broken as it moves downward as a result of the low position of the central incisors (Fig. 15). In addition, the incisal edge of such teeth may be covered by the lower lip in a wide smile due to the low position of the upper incisors. It is the process of excessive teething of the frontal teeth that can determine in this case the excessive visualization of gingival tissue (Fig. 16).
Rice. from 15 to 17
Treatment of dento-alveolar extrusion involves restoring the correct position of the teeth.[19] This can be achieved either through orthodontic treatment or surgically using a segmental osteotomy (Fig. 17). Whatever method is used, mandatory restoration of occlusion is required to achieve stable contact of the frontal teeth, which usually requires the creation of long-term retention.