Cleaning the tooth canals is a procedure for removing microparticles of the inflamed pulp from the roots, i.e. affected tissues. This is a particularly labor-intensive process, since the final effect of caries treatment depends on the quality of the work.
Clinical case: a patient has caries that has developed into pulpitis. When opening the tooth, the dentist diagnosed an infection and a severe inflammatory process; it was recommended to remove dead pulp tissue from the roots. If the work is not performed perfectly, an infection gets into the roots, a filling is placed on top, and the pathological process already develops under a thick layer of filling material. The toothache does not subside, the patient goes to the doctor again or endures the pain, quenching it with medications, and eventually loses the tooth. That is why, in case of caries, pulpitis and other problems, it is important to contact trusted doctors who perform high-quality root cleaning. It is advisable for the dentist to work with a microscope - multiple magnification allows you to monitor the process of cleaning the canals from remnants of pulp tissue.
One tooth may have two or more tubules, which are localized in the layers of the periodontium. The main task of the canals is to be a connecting link between the crown pulp and the nerves.
More than 10 years ago, deep caries and advanced pulpitis were the reasons for removing a unit, but now, thanks to effective cleaning and treatment of the canals, it is possible not only to preserve the crown, but also to restore its integrity to an ideal result.
Features of dental canal treatment
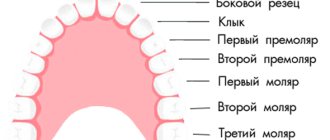
Differences in the structure and functions of the “representatives” of the dentition largely determine the nature of the treatment approach. Treatment of canals for different groups of teeth has its own nuances.
Front tooth canal treatment
The front teeth most often have one canal. They are often curved and difficult to pass through for instruments. In order to preserve aesthetics, the opening of the cavity of these teeth is carried out from the vestibule of the oral cavity. Due to their frontal location, it is important to prevent tooth enamel from darkening, so filling materials containing dyes are not used.
Treatment of wisdom tooth canals
Wisdom teeth can have more than 5 canals; they often have a branched structure, which is not always revealed by x-ray examination. These factors, along with the marginal location of the “eights”, significantly complicate the high-quality treatment of root canals. At the final stage of treatment, various filling pastes are traditionally used.
Root canal treatment of temporary teeth
Endodontic treatment of tooth root canals is usually used only at the stage of root stabilization. When choosing the optimal treatment tactics, it is necessary to take into account the specific structure of temporary teeth. The small thickness of the canal walls, the insignificant degree of dentin mineralization and the relatively large size of the apical foramen are the main reasons for special caution during instrumentation. Zinc oxide eugenol and iodoform pastes, as well as materials based on calcium hydroxide, are usually used as filling agents. They are not toxic to the permanent tooth germ and are able to dissolve along with the temporary root.
Installing a seal
The task of the doctor who has discovered a tooth damaged by caries is:
- drilling out dead tooth tissue and darkened parts of enamel;
- expansion of the carious cavity;
- checking the condition of the pulp;
- preparing the tooth for filling.
The filling process consists of:
- in disinfecting the drilled cavity and drying it;
- installing a medicinal inlay into the tooth canals;
- installation of a temporary filling;
- A permanent filling is installed when a tooth is cured and the lost parts need to be restored.
Stages of tooth canal treatment
Endodontic treatment usually lasts several hours and includes a number of stages.
- Removal of the pulp (pulpectomy).
The inflamed soft tissue of the tooth is eliminated. - Root canal sanitation.
The procedure is a “cleaning” of bacteria and dead tissue elements. Pulpectomy and canal sanitation pursue one of the most important goals - eliminating existing inflammation. - Channel formation.
The root canal, freed from pathological contents, undergoes appropriate treatment. In addition to ensuring good passage of the canal, it is imperative to ensure that its apex reaches the apical part of the tooth. - Canal filling.
The last stage of the intervention is filling the root canal with filling material, followed by grinding.
When is endodontic intervention indicated?
Endodontic treatment is carried out in the following cases:
- Inflammation of the coronal and root pulp - pulpitis. Moreover, the form of the disease can be both acute and chronic.
- Periodontitis.
Inflammation of blood vessels and nerve fibers is observed in complicated forms of caries, with a cracked tooth. Inflammation can also be a consequence of injury.
Are there any contraindications for this procedure?
Like any dental procedure, endodontics is contraindicated in a number of cases:
- Vertical incisor fracture.
- Too narrow, impassable dental canals.
- Damage to periodontal tissue.
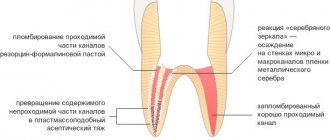
Treatment of teeth with problematic root canals
Filling dental canals
A relatively simple technology for treating tooth canals is filling with a special paste with or without a pin. According to the “gold standard” of endodontics, the canals are also filled with a latex-like material - gutta-percha. Several methods of its use have been developed, including the Termafil system, lateral condensation, injection or liquid thermogutta-percha (vertical condensation). In some cases, in particular when treating a tooth canal cyst, filling is carried out with a substance based on calcium hydroxide (copper-calcium hydroxide “depopheresis” method). However, special nanocomposite materials are increasingly used in dentistry.
Treatment under a microscope
The age-old “tough nut to crack” for the dentist is curved or branched root canals of the teeth. A dental microscope, often in combination with a laser, allows you to completely pass through them and adequately process them along their entire length to reduce tissue trauma. Sometimes it becomes necessary to treat a sealed tooth canal with the evacuation of remaining material of various nature, for example, fragments of fillings, tissue fragments and even instruments. Then a microscope also comes to the rescue. Read more about the technology in a separate article.
Broken instrument in the canal. Clinical tactics.
This article presents the author's view on the problem of broken instruments from a biological point of view.
The author created a clinical decision framework based on the following factors:
1. The tooth is vital or infected.
2. Initial or final stage of canal cleaning.
3. The tool is broken before or after bending.
Based on this pattern, doctors may decide not to remove the instrument, try to bypass it, or try to remove a broken instrument.
A broken instrument in the canal is, unfortunately, a complication of endodontic practice.
Broken instrument in the medial canal
Research shows that steel tools break off in 1 to 6% of cases. With the advent of nickel-titanium rotary tools, a marketing myth arose that they were unbreakable due to their flexibility...
However, the practical activities of endodontists around the world, unfortunately, have refuted this statement. Even among experienced endodontists, breakage of nickel-titanium instruments ranges from 0.5% to 5% of cases. Moreover, while the problem of steel instruments breaking off can be solved by observing signs of metal fatigue and removing such instruments from use, with nickel-titanium instruments, doctors are faced with a situation in which the instrument can break without showing signs of metal fatigue. This occurs either due to fracture due to bending fatigue of the metal or due to a metallurgical defect. Therefore, even one-time use of Ni-Ti tools does not completely prevent breakage.
Broken nickel titanium instrument behind a bend in the medial canal
There are no signs of any deformation on the surface of the nickel-titanium tool after breaking.
The only solution to prevent instrument fracture is to stop clinical work. All the tools break...
In the course of clinical work, doctors are faced with a situation where they may discover a broken instrument in the canal during previous treatments, or they themselves break the instrument in the canal.
Today, under the influence of marketing pressure and with the availability of certain tools and equipment, doctors automatically begin attempting to remove the broken instrument.
Let's look at this problem from different points of view:
1. Broken instrument and failure of endotherapy.
The cause of periapical processes is infection of the root canals.
A broken instrument in itself does not naturally cause inflammation.
Studies have shown that SI is the cause of endodontic treatment failure in only 0.96% of cases (OUTCOME OF ENDODONTIC TREATMENT AND RE-TREATMENT J. Ingle, J. Simon, P. Machtou and P. Bogaerts Endodontics - 5th Ed. (2002) Chapter 13) .
Often we see old endotherapy with broken instruments without any signs of periapical
inflammation. The influence of SI on the forecast will depend on several parameters:
— The tooth is vital or infected.
— At what stage of instrumentation and canal cleaning did the instrument break?
2. Procedure for removing a broken instrument.
The procedure involves creating direct access to the instrument using a modified Gates glidden and the use of ultrasonic tips; some technicians recommend the additional use of grasping instruments, such as IRS, Masserannkit, STN, etc.
This procedure is associated with loss of root dentin, and therefore can lead to complications such as perforation and vertical root fissure due to weakening of the root wall due to dentin loss. It is dentin that provides the strength of the tooth and its loss increases root deformation. Vertical root fracture is responsible for 11% of endodontic treatment failures.
2 broken instruments in the middle part of the canal
After removing the broken instruments, the root walls are thinned and weakened, in one of the areas the root is perforated
3. The instrument broke in the apical part of the canal behind the bend.
In such a situation, no technique is usually effective.
4. Existence of the ByPass procedure.
The procedure is carried out next to a broken instrument. This procedure allows us to clean the canal more apically and thereby solve the problem of infection...
Diagnostic image. Periapical process on the M and D roots, a broken instrument in one of the M canals.
A snapshot of determining the working length. The ByPass of the broken tool is visible.
A snapshot of determining the working length. The ByPass of the broken tool is visible.
Photo at the end of endodontic treatment. Hybrid condensation method.
Follow-up snapshot after 6 months. Almost complete disappearance of periapical processes on M and D roots.
1. Vital teeth.
Breakage of the instrument behind the bend of the canal in its apical part.
The prognosis is good. There is no point in trying to remove the tool.
This solution is applicable only if modern standards of endodontics are observed: working with dental
irrigation with sodium hypochlorite and cleaning of coronal caries before starting canal treatment.
Diagnostic image of the 48th tooth with irreversible pulpitis due to deep caries.
A snapshot of determining the working length.
Image after completion of endodontic treatment. Arrows indicate a fragment of an NT instrument.
Instrument fracture in the coronal part of the canal with direct access.
A photograph after extirpation, during which the instrument broke at the dittobuccal root.
The instrument has been removed by the IRS.
Photo after canal filling is completed.
Breakage of the instrument in the middle or apical part of the canal without bending.
Try to do ByPass (removing the tool is not necessary).
Diagnostic image of the 47th tooth. Broken instrument in one of the M channels.
A snapshot of determining the working length. Bypass a broken tool.
During the process of widening the canals, the broken instrument was removed from the canal.
Photo at the end of endodontic treatment.
2. Infected tooth.
The breakage occurred at the final stage of channel formation and cleaning.
There is no need to remove a broken tool.
Diagnostic image with gutta-percha in the fistula tract (tracing). Periapical lesions on M and D roots.
Working length shot.
Photo after canal filling is completed. The arrow indicates a broken NT instrument in the Mesiobuccal
channel.
Follow-up after 6 months. Complete disappearance of periapical processes. The normal contour of the periodontal fissure has been restored.
The tool broke off in the initial stages of canal formation and cleaning.
1. Trying to pass near a broken instrument (ByPass)
Diagnostic image. Broken and in the medial canals there is a periapical process on the M and D roots extending into the furcation area.
Working length shot. SI bypassed.
Photo at the end of endodontic treatment. The broken instrument is visible in the canal.
Follow-up after 6 months. Reduction of the periapical process.
2. If ByPass fails and the tool breaks off before bending.
Diagnostic image of the 37th tooth. The SI in the apical part of the canal partially extends into the periapical region. The patient has persistent sensitivity when chewing.
Picture after SI extraction. Gates Glidden technique and ultrasonic tips were used.
Photo after completion of filling the distal canals.
3. If the ByPass attempt was unsuccessful and an experienced doctor was unable to remove the instrument within an hour, or
the instrument broke behind the bend and attempting to remove it is dangerous from the point of view of weakening the root and perforations.
Intracanal attachment based on Ca(OH)2 for a period of 2 to 4 weeks. Canal filling and follow-up after 6 and 12 months.
If the periapical process increases, the decision is about apical surgery or tooth extraction.
When re-treating the 36th tooth with SI in the M channel behind the bend, it was not possible to make ByPass.
Canal filling after 4 weeks of using Ca(OH)2.
Follow-up after 6 months. Reduction of the periapical process.
The clinical tactics I have proposed are based on an understanding of the biological processes underlying periapical pathologies and dental biomechanics.
I believe that the mechanistic approach to solving the problem of a broken instrument - attempting to remove it in any case - is not correct. The procedure for removing a fragment of a broken instrument is associated with the loss of healthy root dentin. During this procedure, there may be perforations, or, as a delayed complication due to weakening of the tooth, a vertical root crack may occur.
Of course, in practice there may be cases that do not fall 100% under this scheme, and the doctor must make decisions based on a biological understanding of the situation, and not due to marketing pressure.
Author:
Dr. Solomonov Mikhail
If your tooth hurts after root canal treatment
If after root canal treatment your tooth hurts when you press it, this is normal. This phenomenon is associated with insufficient anesthesia in the area of endodontic intervention. Another reason why a tooth hurts after canal treatment is excessive treatment with the instrument moving beyond the apical foramen.
How long does a tooth hurt after root canal treatment? Sometimes pain persists for several days due to intensive intervention in the tissue structure in such a limited area. A similar situation occurs when an excess amount of filling material is placed into the canal, which causes discomfort when pressure is applied to the walls. As a result, the tooth “aches” after canal treatment. In any case, the presence of post-filling pain signals the need for a second visit to the dentist.
What complications do impacted teeth cause and why do they need to be “extracted”?
It is difficult for the patient to immediately understand what danger “hidden” teeth can pose, but it is really serious.
Semi-retinated teeth cause inflammation of the “hood” with which they are covered and adjacent tissues, and this provokes purulent inflammation.
Fully impacted teeth that lie in the jaw can behave like a foreign body; they put pressure on neighboring teeth, causing their displacement and a number of other problems.
In this case, the patient experiences pain and fever in case of inflammation, a feeling of pressure and discomfort in the jaw, neuralgia or numbness of part of the face.
If we list the diseases that can result from impacted teeth, it will become clear that this is a real “time bomb” that can detonate at any moment.
What diseases can be caused by an impacted tooth:
- periodontal cyst,
- caries of neighboring teeth and their roots,
- pulpitis,
- pericoronitis,
- periostitis,
- periodontitis,
- purulent lymphadenitis,
- inflammation of the trigeminal nerve,
- odontogenic sinusitis,
- abscess,
- phlegmon,
- resorption (resorption) of the roots of adjacent teeth,
- bad habits: mouth breathing, infantile swallowing, inserting the tongue into a dental defect,
- problems with biting food,
- malocclusion, displacement of interdental contacts, crowding of teeth.
Possible complications
Not all cases go smoothly. Let's consider the main problems that arise after the procedure.
- Perforation.
The phenomenon is the formation of holes between the dental canals and surrounding tissues. Treatment of perforation consists of medicinal treatment and filling. - Cheek swelling.
The reason why the cheek is swollen after root canal treatment is believed to be the impregnation of the periodontal tissues and mucous membranes with an anesthetic drug, which themselves are quite loose and easily absorb liquid. - Instrument fracture.
The probes for passing through the channels are very thin. If they break during medical procedures, the fragments are removed with special devices. Modern dental instruments made of nickel-titanium alloys are less susceptible to wear and break less often. - Adverse reactions to medications.
The range and severity of side effects of modern anesthetics are minimal. Before treatment, the doctor must collect an allergic history - information about drug intolerance - and the likelihood of a full-blown allergic reaction is practically reduced to zero. Adverse reactions of moderate and minor degrees are mostly short-term, can be easily corrected or can be overcome by changing the drug. - Other complications.
Situations such as swallowing particles of fillings, tooth dust, and small instruments now practically do not occur thanks to the use of a rubber dam - a latex plate that separates the tooth or teeth being treated from the oral cavity.
How are impacted teeth diagnosed?
Impacted teeth are often “found” by accident during an X-ray diagnosis for another dental reason. If a patient asks about orthodontic treatment and is missing some teeth, or has symptoms that may be caused precisely by the presence of hidden impacted teeth, then a special diagnosis is carried out.
The problem of impacted teeth is solved by two specialized dentists - an orthodontist and a surgeon, so the patient will have to undergo diagnostics by an orthodontist and diagnostics by a surgeon. Most of the diagnostic procedures will be general, and the key is x-ray diagnostics, and it is preferable to do CT - computed tomography (3D diagnostics). Unlike an orthopantomogram (OPTG), it shows the spatial location of the impacted tooth in the jaw and relative to other teeth, which is very important for the surgical stage of traction - exposing its crown, because allows the surgeon to choose the optimal “approach”.
When is tooth extraction necessary after root canal treatment?
It happens that you have to part with a treated tooth. Typically, such a sad outcome is due to the following factors:
- initially unsatisfactory root canal treatment with the development of poorly controlled inflammation;
- some cases of wisdom teeth treatment;
- the complexity of the anatomical structure of roots and canals in a particular patient;
- late request of the patient for specialized help, in which adequate therapeutic measures do not lead to the desired result.
What are the types of tooth impaction?
There are two types of retention - partial, in which part of the tooth is visible from the gums, and complete - in which the tooth is completely located under the gum tissue and/or jaw bone.
Such teeth can also be positioned differently, both being in “their” place in the dentition and occupying an incorrect position outside the dentition.
- Vertical
- Horizontally.
- At an angle to the jaw
If a tooth does not erupt in the right place beyond the border of the dentition, they speak of tooth dystopia.
There are even reverse retentions, when the tooth lies “upside down,” that is, upside down with its roots.
There may be only one impacted tooth in the dentition, or two impacted teeth may be located symmetrically. This problem concerns both milk and permanent teeth.
What is the cost of treatment?
How much does root canal treatment cost? The cost largely depends on the method used and the quality of the materials. When using laser and microscopic technology, nanocomposites and other advanced developments, the cost of tooth treatment with canal filling increases significantly. Approximate prices for root canal treatment in Moscow with gutta-percha filling and composite filling are presented in the table below.
| View | Price |
| Single channel tooth | 9,500 – 12,5000 rubles |
| Double channel tooth | 11,000 – 14,500 rubles |
| Three-channel tooth | 13,500 – 17,000 rubles |
The cost of root canal treatment should not be the determining factor in choosing a clinic. Contact only dentistry with a good reputation and experienced specialists who use modern equipment and the latest techniques in their work. Remember - the future fate of your teeth and the aesthetics of your smile depend on the quality of canal treatment!
How is surgery performed to expose the crown of an impacted tooth?
- As a preliminary stage, preparation for the operation is carried out. The patient undergoes professional hygiene and sanitation to reduce the amount of infection in the oral cavity and speed up postoperative healing.
- The operation to expose an impacted tooth is performed under local infiltration anesthesia and is considered a fairly serious surgical intervention.
The operation to expose the crown of an impacted tooth and install an orthodontic element on it can be carried out according to 2 schemes:
I Delayed bracket installation.
- The mucous membrane in the projection of the crown of the impacted tooth is excised, the entire crown of the tooth is exposed, and a special tampon is installed in the wound.
- After 2-3 days, a button or bracket is installed on the crown of the exposed tooth, which is tied to the orthodontic arch and traction begins.
II Bracket installation during surgery
- The dentist-surgeon peels off a small mucoperiosteal flap and exposes part of the crown of the impacted tooth, onto which the locking element is immediately fixed.
- The bracket is tied to an orthodontic arch or additional devices.
- After installing the orthodontic element, the flap of tissue is placed in place and the wound is sutured.
The disadvantage of this method is that in this case, repeated surgical intervention is possible if the bracket on the tooth comes off.
After surgery, the patient is prescribed antibiotics and antiseptic rinses, if necessary, to speed up healing. Light, non-traumatic food is recommended.
Pain after a filling falls out and other unpleasant consequences
Simple recommendations for patients on what to do when a filling falls out and a tooth hurts:
- You need to rinse with a solution of baking soda and salt.
- You can take a painkiller, it could be Ketanov or Analgin.
- During the inflammatory process, the temperature may rise. It must be knocked down after exceeding 38.5° C. For this, antipyretics are used.
- If there is bleeding from a tooth, you should immediately consult a doctor. There can be many reasons for this phenomenon, and it will be possible to accurately determine the possible problem only after an appropriate examination.
You can find many tips on how to numb a tooth at home, but the most effective option is to rinse and take appropriate medications.
When a filling with arsenic falls out, you need to carefully remove the remaining medication with a cotton swab and rinse the tooth cavity with a soda solution.
Diagnostic methods
Diagnosis of tooth perforation is based on patient complaints and visual examination of the oral cavity. In most cases, perforation in the crowns of teeth can be recognized using an x-ray. If there is a suspicion of perforation localized in the area of the bottom of the dental cavity, an X-ray with contrast is performed. In any case, an image is taken that allows you to determine not only the presence of perforation, but also to identify complications caused by the pathology.
When holes form in the dental canal, additional equipment and tools are required to identify them. It is easier to diagnose perforation when there are already symptoms: sharp pain, mild bleeding, changes in the movement of the instrument during dental treatment.
With old perforation formed in the canal, symptoms appear, which in their manifestations resemble periodontitis. It is diagnosed along with inflammation, which affects the tissues located near the roots of the teeth. In the presence of such perforation of dental units, characteristic pain in the tooth is observed, which appears when pressing on the damaged segment, swelling of the gums, concentrated in the area of inflammation.
Tooth perforation, localized in the root of the teeth, is diagnosed using a paper pin by immersing it in the canal. The location of the perforation is determined by the trace of blood that remains on the paper.
What happens if you leave the problem without a solution?
Tooth perforation is a fairly serious problem leading to various dental problems. If a cavity forms in the root canal, root apex or tooth walls, immediate treatment is required. Lack of therapy can lead to the following consequences:
- the development of a granuloma - a cavity filled with pus, which can grow, gradually affecting nearby tissues;
- if left untreated, granuloma can develop into a cyst;
- if the tooth structure is severely damaged, root fracture may occur, which is difficult to detect without x-rays;
- development of inflammatory processes with severe painful symptoms that complicate chewing food;
- Aggravated tissue inflammation can affect speech, causing speech defects.
The perforation options don't end there. Various inflammatory and destructive processes can develop, which lead not only to dental diseases, but also to their loss.
Is it possible to close a hole in a tooth yourself?
The question often arises as to what can be used to seal a temporarily opened cavity if a filling falls out. People use a wide variety of materials for these purposes - from cotton wool to chewing gum, in general - everything that can be used to fill a hole at home. Under no circumstances should this be done. Before you tape a tooth, you should think about the consequences. The cavity will not be closed hermetically, which means food debris and bacteria will get into it.
Before you think about how to plug a tooth at home, it is worth considering that any material will create extremely favorable conditions for the proliferation of microbes and the occurrence of infection or inflammation. Therefore, the question of how to cover the tooth should not arise. To avoid the accumulation of food debris in the cavity, it should be rinsed regularly at least 6-7 times a day.