Content:
- Description of the disease
- Manifestations of the disease
- How does allergic stomatitis develop?
- Why does it occur
- Establishing diagnosis
- Fighting the disease
- How to reduce the risk of developing the disease
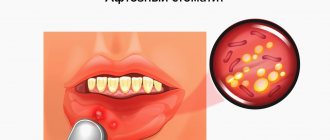
A dental disease in which the integrity of the oral mucosa is damaged - allergic stomatitis - occurs quite often in medical practice. It comes in different forms, so a person cannot always understand what caused the disease and what factors caused its negative symptoms.
Description of the disease
With the diagnosis described, the oral mucosa is damaged, the tissues become very susceptible to all irritants. The incubation period is long. This means that a lot of time passes from the moment the first signs of allergy appear to the manifestation of the disease itself. Because of this, the patient is unable to track the relationship between the symptoms that bother him.
Allergic stomatitis occurs in both children and adults. More often it is diagnosed in people who live in areas with unfavorable environmental conditions.
What is allergic stomatitis?
Allergic stomatitis is called inflammation of the mucous membrane, provoked by hypersensitivity to certain irritants. A distinctive feature of the disease is a long incubation period. That is, from the moment an allergic reaction occurs until the first signs of stomatitis appear, up to four weeks can pass. In general, read about what stomatitis is in a separate article.
People of any gender and age are susceptible to the disease, but people with allergies, workers in hazardous industries and residents of areas with poor ecology are at risk.
Manifestations of the disease
The disease negatively affects the functioning of the entire body. It doesn’t just cause inflammation of the mucous membranes—it also causes migraines, elevated body temperature, and lethargy. Many people notice dry mouth, severe pain when chewing, which is present even when the integrity of the tissues has not yet been compromised.
Saliva thickens, becomes viscous, more like foam. The gums, tongue, and inner surface of the cheeks may swell. All these symptoms deprive the patient of the opportunity to lead a normal lifestyle.
You shouldn’t wait for the disease to clear up. The sooner her treatment is started, the sooner her health will be normalized.
How does allergic stomatitis develop?
Dentists distinguish three stages of the disease:
- Primary or catarrhal. A person notices a burning sensation in the mouth, drying out of the mucous membranes. There are no ulcers or plaque yet or they are barely noticeable. If treatment is not started, the resulting ulcers will begin to grow.
- Bullous. Bubbles form on the tissues. There is a cloudy liquid inside them.
- Ulcerative-necrotic. The most dangerous stage in the development of pathology. The pain in the mouth becomes very strong, acute, and does not go away even during rest. The mucous membranes of the mouth swell, turn red, and look inflamed. Numerous ulcers are visible on them, covered with a dense gray coating. If you try to remove the top film, the wound begins to bleed.
You can't start a disease. It is much more difficult to treat the ulcerative-necrotic form of stomatitis than the catarrhal form.
Why does it occur
From the name of the disease it is clear that it is allergic in nature. The disease develops in two cases:
An allergen enters the patient's body. As a result, a pathological response of the immune system develops. We are talking about allergies to pollen, medications, mold, and food.- The tissues of the oral cavity come into direct contact with the allergen. This means that the oral cavity has been treated with something (for example, a medicinal composition, toothpaste, mouthwash) or some kind of dental structure has been installed.
Most often, allergic stomatitis is a consequence of individual intolerance to the materials used by the dentist. Thus, many people are allergic to application solutions, orthodontic appliances, metal braces, and plastic dentures.
An important role in the pathogenesis of the problem is played by advanced caries, chronic tonsillitis, and microorganisms that accumulate under the crowns and cause harm to the mucous membranes. All these are also factors that increase the risk of developing the disease.
Today it has already been proven that people who are diagnosed with allergic stomatitis are more likely to experience:
- inflammation of the stomach, colon mucosa, pancreas;
- disturbance of the gastrointestinal microflora;
- helminthiasis;
- diabetes;
- hyperthyroidism
This is explained by the fact that with these diagnoses, systemic disorders develop in the body, which negatively affect the functioning of the immune system and cause high sensitivity to various types of allergens.
The disease does not always occur in isolation. It is often included in the structure of Lyell's, Reiter's, Stevenson-Johnson syndromes, vasculitis, etc.
Causes of development of allergic stomatitis
The main cause of pathology is the entry of an allergen into the body. Allergies can occur due to taking antibiotics, insect bites, accumulation of dust, food or contact with materials. Depending on the cause, there are several types of allergic stomatitis.
Contact allergic stomatitis
Occurs due to the effect of drugs and materials on the mucous membrane, for example, orthodontic apparatus, prosthesis or cement for its installation. The formations are usually located only at the site of contact of the mucous membrane with the irritant. A distinctive sign is swelling of the cervical lymph nodes.
Toxic-allergic stomatitis
Appears when pathogenic organisms multiply in the oral cavity, causing toxic poisoning. It is characterized by swelling of the mucous membrane, milky or brownish coating on the tongue.
Drug-induced allergic stomatitis
Develops after taking medications orally or when applied topically. Accompanied by nausea, headache, difficulty breathing, fever and numerous rashes. With drug-induced stomatitis, it is necessary to first relieve the symptoms of intoxication and only then treat the external manifestations of the pathology.
Establishing diagnosis
If there is a suspicion that the patient has allergic stomatitis, he must be examined by a dentist. If necessary, allergists, immunologists, dermatologists, endocrinologists, gastroenterologists, rheumatologists and other specialized specialists are involved in the diagnosis. The attending physician must collect a detailed medical history to understand what caused the disorder and what substance acts as an allergen.
During an examination of the oral cavity, the dentist observes reddened and swollen mucous membranes. In some places, round ulcers are visible on it, covered with a white or gray coating. Saliva is usually very thick.
The specialist pays attention to the condition of the existing prostheses and finds out how long ago they were installed. To study the electrochemical processes occurring in the oral cavity, a saliva test is taken from the patient. It is important to determine the pH of biological material and evaluate the content of microelements in it. Allergy diagnostics involves conducting special tests - skin tests, provocative tests, etc.
If allergic stomatitis is suspected, it is important to differentiate it from a deficiency of vitamins C and B, herpes, candidiasis, leukemia, and HIV. With all these diagnoses, changes in the structure of the oral mucosa are also observed.
Fighting the disease
What therapeutic regimen the doctor will offer the patient depends on the cause of the disease and the type of provoking factor. The first thing to do is to completely eliminate contact with the allergen. But to do this, you must first establish what exactly this allergen is. If there is no answer to this question, the patient is asked:
- stop taking medications he was previously using;
- follow a strict diet;
- change your toothbrush and toothpaste;
- stop wearing dentures.
In this way, the doctor tries to eliminate the influence of the most common allergens.
Drug therapy involves the patient taking antihistamines. They are always used for allergies. The use of vitamin-mineral complexes is also indicated. It is especially important that they contain folic, nicotinic and ascorbic acid, and B vitamins.
Affected areas should be treated regularly:
- special dental anesthetics;
- corticosteroid gels;
- enzyme compounds;
- drugs that accelerate regenerative processes.
If stomatitis is a consequence of recent dental treatment, you should consult a dentist again as soon as possible. It is possible that you will have to replace the installed fillings and crowns.
Among the folk methods that are effective for stomatitis, rinsing with cabbage juice, aloe infusion, diluted sea buckthorn oil, and chamomile decoction help. You can also apply grated raw potatoes to the wounds.
Treatment of allergic stomatitis in adults and children is carried out according to the same scheme. The only difference is in the medications prescribed: not all formulations for adults are suitable for children, and vice versa.
Types of stomatitis
Stomatitis comes in different forms: it depends on the causative agent of the disease. So, it can have a viral, microbial or mycotic etiology. Accordingly, the symptoms, description and principles of treatment of the disease will be different.
Aphthous stomatitis: treatment
The exact reasons why this type of stomatitis occurs have not yet been established. Some experts consider staphylococci and adenoviruses to be the source of ulcers, while others attribute the disease to a viral disease. Some doctors equate aphthous stomatitis with herpetic stomatitis, with the only difference being that in the first case, instead of ulcers, aphthae appear - round white or yellow plaques with a red frame. Aphthae are concentrated on the cheeks, lips, and tongue.
The disease occurs against a background of decreased immunity and can transform into an ulcerative-necrotic form.
Treatment of aphthous stomatitis in adults is as follows:
1. Local treatment, including treatment of aphthae and rinsing the oral cavity with disinfectants and antiphlogistic agents, such as hydrogen peroxide (diluted 1:1 with water), furatsilin tablet, boric acid, sea buckthorn oil.
2. Drug therapy aimed at detoxification and desensitization.
3. Vitamin therapy.
4. Use of sedatives and antihistamines.
5. Physiotherapy.
6. Diet, which consists of excluding spicy, allergenic and rough foods from the diet.
Aphthous stomatitis in adults often occurs against the background of exacerbation of pathologies of the nervous, endocrine systems and diseases of the gastrointestinal system. Therefore, its prevention will be the treatment of concomitant diseases.
Since aphthous stomatitis is often caused by staphylococcus, a pathogen that multiplies in dental plaque and teeth affected by caries, a thorough improvement of the oral cavity is necessary. With surgical dental treatment and removal of dental plaque, the problem of aphthous stomatitis in adults is minimized.
Herpetic stomatitis: symptoms
Herpetic or herpes stomatitis is the most common form of manifestation of the disease. Almost 90% of the adult population are carriers of the herpes virus, which in itself does not cause any discomfort. But with a decrease in immunity, exacerbation of chronic pathologies or trauma to the oral cavity, it can intensify and manifest itself in the form of herpetic stomatitis.
This type of stomatitis most often affects the cheeks, tongue, and palate. The clinical description of the oral cavity will be as follows: the mucous membrane becomes swollen and red. Against this background, small rashes appear.
The disease lasts about ten days, during which the adult usually does not experience any acute reaction to the appearance of ulcers. Body temperature remains normal, no symptoms of intoxication are observed, and the person feels relatively well. In case of reduced immunity or in a child, general intoxication, malaise and high fever are possible.
Discomfort is caused only by the process occurring in the mouth, consisting of:
• formation of bubbles;
• merging them into a group;
• bursting of ulcers and the formation of painful erosion (it hurts a person to drink, eat, talk).
The disease is also often accompanied by enlarged lymph nodes.
Sometimes herpetic stomatitis can develop into gingivitis, characterized by sharp redness of the gums around the teeth. Also, with gingivitis, rashes can affect the red border of the lips. Treatment for gingivitis is problematic, so it is better to prevent herpes from developing into gingivitis.
Treatment of stomatitis consists of taking medicinal anti-inflammatory, anesthetic and antiviral drugs. It should be remembered that herpes is not sensitive to conventional disinfecting infusions, so herbs and chlorhexidine are not a help here.
Local treatment and vitamin therapy also help. It should also be borne in mind that this form of the disease is contagious, therefore, during the period of illness, close contacts associated with kissing, drinking from the same cup, etc. should be limited. This especially applies to people whose disease has progressed to gingivitis.
Candidal stomatitis: treatment
This is already a fungal manifestation of a disease that is characteristic only of people with a very weakened immune system, suffering from chronic diseases or taking steroid hormones.
The causative agent of the disease is the Candida fungus, which is always present in the oral cavity. Its reproduction and manifestation in the form of a cheesy coating and white spots begins only in the presence of provoking factors.
The treatment regimen for stomatitis in adults consists of the following measures:
• taking antifungal medications;
• treatment of lesions with antifungal gels and ointments;
• if you have dentures, treat them with antiseptic solutions;
• rinsing the mouth;
• exclusion of easily digestible carbohydrates from food;
• visiting a gastroenterologist and endocrinologist, since the disease is often caused by pathologies characteristic of these medical areas.
Catarrhal stomatitis: causes of occurrence
This is the mildest and most common form of stomatitis. Often this is where other types of disease begin. With timely rinsing of the mouth, the disease will subside within a couple of days. Otherwise, it may develop into a more severe form. The patient only has to follow one simple rule: you need to rinse your mouth for at least a minute.
Externally, the disease looks like a light coating on the mucous membrane and is accompanied by slight swelling and redness. You may also experience bad breath, increased salivation, and a severe burning sensation in the mouth.
The main reason why catarrhal stomatitis occurs is oral candidiasis, which occurs against the background of a general inhibition of the body's defenses. The causes of the disease also include:
• inadequate oral care;
• diseases in the gastrointestinal tract of a chronic nature;
• damage to the body by worms;
• dental problems – untreated caries, periodontitis, dental plaque.
Regular visits to the dentist will help eliminate the problem of the development of catarrhal stomatitis and its transition to another form of the disease.
Allergic stomatitis
Allergic stomatitis in adults is not an autonomous disease: it can accompany any allergic reaction in a person. Particularly susceptible to illness are individuals who react with allergies to food or medications when there is direct contact of the allergen with the oral mucosa. People also often react to dentures with allergic stomatitis.
Allergic stomatitis comes in several types:
• viral;
• bacterial.
It depends on the causative agent of the infection. Often, due to allergies, aphthous stomatitis can occur, which is called aphthous allergic stomatitis.
Signs of stomatitis are manifested by the appearance of white spots or small blisters in the mouth. The mucous membrane turns slightly red and becomes covered with pinpoint hemorrhages. The person may experience pain, burning, severe itching, or dry mouth.
Treatment of stomatitis comes down to taking medicinal antihistamines and eliminating the main cause of the allergy.
Prosthetic stomatitis: causes
Prosthetic stomatitis in adults manifests itself in two types: allergic and bacterial. In both cases, the clinical picture is manifested by a sharp reddening of the mucous membrane of the prosthetic bed. And with the allergic type, redness also occurs in all areas of the mucous membrane that are in one way or another in contact with plastic.
The causes of prosthetic stomatitis depend on its type:
1. Allergic
This is a common allergic reaction to dentures. The main reason for this is the monomer included in the structure of acrylic plastic, which is used in the manufacture of prostheses. Also, the reason for the body’s reaction to dentures may not be the competence of the dental technician, who committed a violation in the selection of the proportion of components in the manufacture of plastic.
Replacing a low-quality prosthesis can solve the problem.
2. Bacterial
In this case, the “owner” of the prostheses himself becomes the culprit of the disease. It must be remembered that removable dentures require the same care as teeth. They must be constantly cleaned after eating. Otherwise, pathogenic elements may form on the surface of the product, which, in addition to the proliferation of bacteria, become a source of unpleasant odor.
Therapy for denture stomatitis consists of disinfecting rinsing of the oral cavity and treating the inner surface of the denture and the mucous membrane underneath it. It is enough to apply a small layer of antiseptic to relieve the painful condition.
Vincent's ulcerative necrotizing stomatitis
The main difference between ulcerative stomatitis is the presence of large, small-sized ulcers in the oral cavity coupled with the death (necrosis) of gum tissue. The disease is quite rare and may be a consequence of untreated catarrhal stomatitis.
Favor the development of Vincent's stomatitis:
• bacterial growth due to poor oral hygiene;
• weakened immunity;
• smoking;
• previous viral diseases.
The cause of the disease is often gastric ulcers and various poisonings.
The development of pathology occurs according to the following scheme:
1. Changes in the oral cavity
The patient notices dryness of the mucous membrane, bleeding gums, the appearance of ulcers on the hills between the teeth, which are later covered with plaque. Inflammation affects the inside of the cheeks, palate, and tongue, making eating and talking painful.
2. General health
The disease is accompanied by fever, weakness, and loss of appetite. The lymph nodes may become enlarged and tender to the touch.
To treat ulcerative stomatitis, the help of a specialist is necessary. Under anesthesia, he will remove dead tissue, bacterial plaque and tartar. Otherwise, you can get exposure of the roots of the teeth and massive necrosis of the gums.
Further therapy consists of the use of antibiotics and antihistamines, disinfectant rinsing and local treatment of the mucous membrane. If necessary, antipyretic and painkillers help. A course of vitamins also has a therapeutic effect.
Stomatitis acute and chronic
Stomatitis in adults differs not only in the form of manifestation. There are also differences in the nature of the disease. So, it can be acute and chronic. The first is characterized by the following description:
• swelling and hyperemia of the mucous membrane;
• formation of ulcers, erosions and plaque.
Stomatitis transforms into a chronic form if it becomes acute. And if a person’s immunity is weak, then the causative agent of the disease remains in the oral cavity constantly even after treatment. As a result, inflammation takes on a chronic form, characterized by a sluggish course with relapses.
The most common chronic form of the disease is characteristic of herpetic stomatitis. The herpes virus, even despite complete recovery, continues to constantly remain in the nerve endings of cells and is activated at the slightest weakening of the immune system.
Microbial carious stomatitis
There is another type of major stomatitis, which is an accompanying disease and manifests itself during the development of infectious diseases - microbial carious stomatitis. The origin of the disease in this case may be related to:
1. With any dental problems that are a source of infectious processes
Tartar, caries, dental plaque - all this is a place where carious bacteria - streptococci and staphylococci - are concentrated. At the slightest trauma to the mucous membrane, carious infection leads to the development of stomatitis.
2. With scarlet fever or sore throat
Scarlet fever is accompanied by a strong white coating on the tongue, which after a few days is replaced by a bare, bright red surface of the mucous membrane. In this case, they also talk about bacterial microbial stomatitis. A white coating on the tongue also accompanies a purulent sore throat. In the case of stomatitis, inflammation spreads not only to the mucous membrane and throat, but also to the gums, which look reddened, swell and hurt.
Therapy for microbial carious stomatitis consists of antiseptic rinsing and diet.
How to reduce the risk of developing the disease
If stomatitis has already occurred, the likelihood of it reoccurring is very high. To avoid illness, you should follow the recommendations:
Pay maximum attention to oral hygiene. It is unacceptable to brush your teeth only occasionally. This should be done in the morning after meals and in the evening before bed. After each snack, it is advisable to rinse your mouth with warm water. To prevent plaque from accumulating in the interdental spaces, they need to be cleaned daily with dental floss or an irrigator.- Strengthen immunity. During the cold season, you need to take a vitamin-mineral complex. Proper nutrition is of particular importance. The diet should be enriched with fresh fruits and vegetables.
- Give up bad eating habits. You need to stop consuming large amounts of spices and alcohol.
- Combine medications wisely. If you need to take antibiotics for a long time, it is advisable to include antihistamines in the course - drugs that reduce the likelihood of developing allergic reactions.
- Have professional oral hygiene every year. This is a general strengthening measure. It keeps teeth and gums healthy for many years.
Regular visits to the dentist allow you to detect all dental diseases at the earliest stages. Therefore, even if nothing bothers you, do not forget to visit your doctor once every six months.
Prevention
If a patient once experiences allergic stomatitis, there is a high probability of it developing again. To prevent pathology, you need to pay attention to the following points.
- Immunity.
To strengthen the immune system and general health, it is recommended to take a course of comprehensive vitamin intake. - Nutrition.
It is better to exclude allergenic foods and hot spices from food and create a balanced menu. - Medicines.
When taking strong medications, especially antibiotics, it is necessary to include antihistamines, that is, antiallergic agents, in the list of medications. - Oral care.
If a toothpaste, brush or mouthwash causes discomfort, irritation or itching, you need to change the products yourself or choose the right ones together with your dentist.
The risk of developing allergic stomatitis and other diseases is minimal if you visit the dentist every six months for the prevention and timely treatment of pathologies in the early stages!