Symptoms of this disease will be:
- hyperemia, swelling, burning and hemorrhages from the gums;
- hypersensitivity to cold, hot, sour foods;
- aesthetic defect of the gums.
Often, hypertrophied gums act as a mechanical obstacle when chewing food, which contributes to injury, penetration of pathogenic microorganisms into damaged areas and aggravation of the inflammatory process. Diagnosis of hypertrophic gingivitis is carried out through examination, palpation examination of the patient’s gums, determination of dental indices, as well as based on the results of additional studies (radiography and CT of the dental system). Therapeutic tactics include the use of local anti-inflammatory drugs, physiotherapeutic procedures, sclerotherapy, diathermacoagulation of the gum papillae and surgical excision of hypertrophied tissue (gingivectomy).
According to statistical data, the children's category of the population suffers from this disease most often, especially children and adolescents in the pre-pubertal and puberty period (from the beginning to full puberty), since the phenomenon of hypertrophic gingivitis is often associated with hormonal development.
Hypertrophic gingivitis is one of the forms of gingivitis (inflammation of gum tissue) and is less common in comparison with other forms (catarrhal, atrophic, ulcerative necrotic).
Classification of gingivitis according to ICD-10
- K05.0 Acute gingivitis
- K05.1 Chronic gingivitis
- K05.11 Hyperplastic
- K05.18 Other specified chronic gingivitis
- K05.19 Chronic gingivitis, unspecified
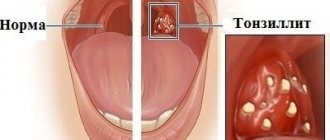
Normally, the gum reaches the crown of the tooth without covering it. It is pale pink, does not hurt or bleed. There is no noticeable distance between the tooth and the gum, however, with hypertrophic gingivitis, due to the enlargement of the gum, a “false pocket” appears between the tooth and the gum, i.e. The gum is attached to the tooth, and its enlarged part forms a pocket.
Principles of treatment
Treatment of gingivitis begins with hygiene: professional teeth cleaning. It is important to remove soft and hard dental plaque. For this, hand tools, an ultrasonic scaler, and the powder blasting method can be used. Subgingival dental plaque can be removed using the Vector device.
It is important to eliminate foci of infection - to fill teeth affected by caries, to undergo endodontic treatment in the presence of pulpitis, to remove the roots of teeth that cannot be restored and are not involved in the prosthetic process.
It is necessary not only to pay attention to the causes of the disease, but also to reduce the influence of harmful factors:
- stop smoking;
- consume food and drinks only at a comfortable temperature;
- remove spicy and smoked foods, marinades, especially those with vinegar, from the diet;
- During the treatment period, try to eat less solid food so as not to injure the loose gum tissue.
If the source of injury to the mucous membrane is the sharp edges of teeth or dentures, the doctor will immediately take measures to prevent further damage or recommend contacting a dentist of another profile - an orthopedist, an orthodontist.
Causes of hypertrophic gingivitis
Hyperplastic gingivitis can be caused by both internal disorders and local factors.
Local factors
- copious amounts of tartar and plaque
- trauma to the gums due to the edge of a crown, filling, or denture that puts pressure on the gum
- improper use of dental brushes and toothpicks also leads to injury
- malocclusion
- orthodontic devices (braces, plates): they irritate the gums and complicate oral hygiene
- old and low-quality fillings, crowns or veneers put pressure on the gums and cause them to enlarge
General factors
- taking medications to treat epilepsy, diabetes, reproductive system diseases and heart disease
- taking contraceptives
- physiological hormonal changes in adolescents, pregnant women, and women after menopause
- vitamin deficiency, especially vitamin C
- blood diseases
- endocrine diseases such as diabetes
Drugs for the treatment of gingivitis
Treatment for gingivitis may involve the use of medications in different forms. Mouth rinses based on antiseptics allow you to solve two problems at once: mechanically remove food debris and bacterial plaque, and also deliver active ingredients to inflamed tissues. Dentists recommend using ready-made pharmaceutical products; in each specific case, a specialist will prescribe a medicinal solution to quickly alleviate the condition. Ready-made formulations are more convenient to use, and the concentration of active components in them is known, this distinguishes them from traditional methods.
The most popular are rinses based on the following antiseptics:
- chlorhexidine;
- furacillin;
- chlorophyllipt;
- Metronidazole.
Calendula, chamomile, yarrow, oak bark, and St. John's wort have antiseptic properties. Doctors do not recommend preparing alcohol infusions; it is better to choose decoctions. The recipes call for using one teaspoon of dry raw materials per glass of boiling water. It is important to cool the broth to a comfortable temperature. Take into account possible allergic reactions, give preference to those herbs to which there was no previous intolerance. It is necessary to discuss with your doctor the possibility of using traditional methods.
Effective drugs for the treatment of gingivitis are ointments and gels. Multicomponent local products for applications not only help relieve inflammation, but also have an analgesic, decongestant, and antipruritic effect. The active components of such drugs can be lidocaine, antibacterial, antifungal substances, and antiseptics. The doctor will select a gel or ointment taking into account the shape and type of gingivitis. Thus, for ulcerative inflammation, it may be advisable to use regenerating agents, and acute catarrhal gingivitis will require the use of a powerful anesthetic gel.
For hypertrophic gingivitis, surgery may be required - a simple gingivectomy. This operation involves excision of excess tissue and application of a bandage, and is performed under local anesthesia.
Classification of hypertrophic gingivitis by severity2
| DEGREE OF SEVERITY | A COMMENT | ||
| severity: | Lightweight | a comment: | The gum covers less than half the height of the tooth crown |
| severity: | Average | a comment: | The edge of the gum covers the crown up to half |
| severity: | Heavy | a comment: | The gum covers more than half of the crown |
Causes
Chronic hypertrophic gingivitis is accompanied by active growth of basal cells of the gingival epithelium. The occurrence of the disease can be caused by congenital malocclusions or low attachment of the frenulum, as well as the presence of low-quality dentures, fillings, and dental plaque.
Some common factors also contribute to the occurrence of the disease:
- the presence of chronic diseases of the nervous and endocrine systems;
- long-term use of medications, including antibiotics and hormonal drugs;
- lack of vitamin C in the patient’s body, which is responsible for gum health;
- the presence of hormonal imbalance, including during pregnancy.
Mechanical trauma to the gums from a tooth fragment, poorly fitting filling or prosthesis can also cause the disease.
Most often, the disease is localized on the upper jaw, in the frontal area.
Classification of hypertrophic gingivitis by location2
| DEGREE OF SEVERITY | A COMMENT | ||
| severity: | Localized form | a comment: | The gums are enlarged only in a certain group of teeth; it occurs due to trauma, crowded arrangement of a separate group of teeth |
| severity: | Generalized form | a comment: | The entire gum is affected and occurs when taking medications or diseases. |
Treatment with folk remedies
All “grandmother’s” advice for gingivitis is of an auxiliary nature. You cannot refuse traditional treatment, relying on “time-tested recipes.” This is not stated anywhere, but in ancient times, people, using exclusively natural raw materials, lost their teeth extremely early - by modern standards. It is worth taking advantage of the achievements of science to preserve a beautiful and healthy smile for many years.
As maintenance therapy, it is allowed to use rinses with tinctures and decoctions of herbs (excluding alcohol). Chamomile, St. John's wort, and eucalyptus are beneficial. A side effect of this treatment will be rapid darkening of tooth enamel. Therefore, special herbal remedies produced on an industrial scale will be a worthy alternative to home preparations.
Treatment of generalized moderate and severe periodontitis
Catarrhal and hypertrophic gingivitis symptoms and treatment in adults
The roots of the teeth are exposed - what to do and how to treat them
Splinting teeth for periodontitis with fiberglass and tape
Laser gingivectomy in the area of one tooth
Open and closed curettage of periodontal pockets
Symptoms depend on the form of the disease:
Edema form
The gums between the teeth are red, swollen, glossy, and a false pocket forms between the enlarged gum and the tooth. There is a change in the appearance of the gums, it looks swollen, bleeds, hurts when brushing teeth, and there is a feeling of burning and swelling. The edematous form develops as a complication of catarrhal gingivitis under the influence of an irritating factor (crown edge, fillings, braces, etc.). During pregnancy, hypertrophic gingivitis develops if the woman already had catarrhal gingivitis before pregnancy. The disease may resolve spontaneously after childbirth.
Fibrous form
The gum, as normal, is pale pink, there is no pain or bleeding, but its growth is observed, there are false pockets between the tooth and the gum. Abundant dental deposits are found above and below the gum. The fibrous form often develops when taking medications or in the presence of general diseases, i.e. this is the reaction of the gums to internal changes.
Publications in the media
Gingivitis is an inflammation of the gums caused by the adverse effects of general and local factors, occurring without compromising the integrity of the periodontal attachment.
Etiology • Infectious factor (dental plaque) • Mechanical trauma • Chemical irritation, etc.
Risk factors • Malocclusion • Shallow vestibule of the oral cavity • High attachment of labial frenulum.
Pathogenesis. Catarrhal gingivitis develops as a reaction to irritation. Hypertrophic is caused by endocrine disorders and usually develops during puberty and pregnancy. Ulcerative gingivitis is associated with a decrease in the body's resistance and impaired trophism of gum tissue, often associated with immunodeficiency conditions (leukemia, radiation sickness, etc.). Vitamin C deficiency in the body and the use of certain medications (phenytoin, cyclosporine, etc.) are important.
Classification. According to the form, catarrhal, hypertrophic and ulcerative are distinguished, according to the course - acute, chronic, aggravated, remission. According to the severity of the process, mild, moderate, and severe gingivitis is distinguished; according to its prevalence, localized and generalized.
Clinical manifestations
• Chronic catarrhal gingivitis. The disease often occurs without pronounced subjective sensations, but sometimes patients complain of bleeding gums when brushing their teeth or eating solid food. During the examination, hyperemia and swelling of the interdental papillae and gingival margin are detected, which loses its natural pattern (scalloping disappears). Instrumental examination reveals bleeding gums, abundant soft plaque and pockets of subgingival tartar, and the absence of pathological periodontal pockets.
• Hypertrophic gingivitis. Hypertrophic gingivitis is characterized by an increase in gingival papillae, which can reach the cutting edge of the teeth. Hypertrophied gums can be hyperemic, swollen, bleed easily (granulomatous form) or be dense, pale pink in color with the formation of false pathological periodontal pockets (fibrous form).
• Ulcerative gingivitis (Vincent's ulcerative-necrotizing gingivitis). Against the background of hyperemic and edematous gums, foci of necrosis of the gingival papillae or the entire gum margin are determined. In severe cases, the mucous membrane of the retromolar space is involved in the pathological process (ulcerative necrotizing gingivostomatitis). Necrotic tissues are dirty gray in color, easily disintegrate, after which ulcerative surfaces are formed, covered with a dirty gray coating. Characterized by bad breath and enlarged regional lymph nodes. A disturbance in the general condition of the patient is observed, with an increase in body temperature, sometimes up to 39 °C.
Diagnostics. Diagnosis of gingivitis is carried out according to basic (clinical) and additional research methods. Particular attention is paid to oral hygiene, which is always broken (hygiene index more than 1 point). The depth of the gingival groove is determined with a special graduated probe from four surfaces of the tooth. Special research methods include the Schiller-Pisarev test, the Kulazhenko method and rheoparodontography to determine the functional state of blood vessels. An X-ray assessment of the condition of the bone tissue is required: no abnormalities are detected with gingivitis.
Differential diagnosis • Chronic periodontitis • Periodontal disease.
TREATMENT
Local treatment (carried out under anesthesia) includes the elimination of irritating and traumatic periodontal factors: removal of dental plaque, selective grinding of the occlusal surfaces of teeth, elimination of malocclusions, etc. Drug treatment includes antiseptics, antimicrobial and decongestant drugs, and agents that increase local immunity. Preference is given to long-acting preparations: gels, plates. For ulcerative gingivitis, treatment with proteolytic enzymes is carried out, for hypertrophic gingivitis - sclerosing therapy or diathermocoagulation of the gingival papillae; it is possible to use high-energy laser radiation. Physiotherapeutic means used include low-energy laser radiation, UV irradiation, electrophoresis of drugs and all types of gum massage (automassage, hydromassage, vibration massage, vacuum massage).
General treatment includes vitamin therapy (vitamins C, P, PP, etc.). For ulcerative gingivitis, antibiotics and metronidazole are prescribed. With hypertrophic, there is often a need to correct hormonal levels.
The prognosis is favorable, except for cases of hypertrophic gingivitis caused by taking anticonvulsants.
ICD-10 • K05 Gingivitis and periodontal diseases
Colored plaque
The brightest color is painted on the denser plaque; it is in these areas that teeth are most often not cleaned, which leads to gum inflammation.
After the final diagnosis, the dentist selects treatment tactics depending on the identified form of gingivitis.
Hypertrophic gingivitis
The essence of the disease is reflected in the name - the gums and gingival papillae grow and become oversized. This occurs either through tissue swelling or due to internal proliferation of connective tissue with the formation of scars - fibrosis.
Accordingly, hypertrophic gingivitis can be edematous and fibrous.
The incentives are:
- Hormonal changes in the body during pregnancy;
- Injury to the gums by the edges of dentures and crowns;
- Progression of catarrhal gingivitis;
- Changes in hormonal levels during adolescence.
Edema form of gingivitis
This type of disease is often associated with internal changes in metabolism in women and growing children. The interdental papillae look loose and engorged. At the beginning of treatment, the oral cavity is sanitized, plaque and stones are removed, then anti-inflammatory procedures begin.
Sclerotization is most often used. After applying anesthesia, a special solution containing calcium chloride, magnesium sulfate and glucose is injected into the patient’s gums. The course takes 6-8 days with one or two day breaks.
Advanced swelling of the gums can change; the patient’s mucosa becomes scarred with the formation of fibrous cords.
Fibrous form of gingivitis
The source of troubles are internal changes in living tissues. Surgery is indicated here; unfortunately, fibrosis is not amenable to conservative therapy. First, external irritants are corrected - tartar is removed, the shape of the crown is corrected. Then the hypertrophied tissues are excised. Subsequently, healing bandages are applied.
Types of gingivitis
Based on how the disease progresses, the following types of gingivitis are distinguished:
- Acute - when it appears suddenly and its course sharply intensifies.
- Chronic - the inflammatory process proceeds slowly and the condition worsens gradually.
- Aggravated gingivitis - an increase in symptoms of chronic inflammation.
- Gingivitis in remission is a state of subsidence of symptoms.
According to the form, it is customary to distinguish the following types of gingivitis:
- catarrhal, manifested by swelling and redness of the gums;
- ulcerative, when dead areas of gum appear;
- hypertrophic, characterized by a sharp increase in gums and bleeding;
- atrophic, manifested in thinning of the gums;
- desquamative, characterized by redness and severe detachment of the upper layer of the mucosa.
According to the degree of prevalence in the oral cavity, gingivitis is divided into local (partial) and generalized (extensive).
Gingivitis – gum disease
Gingivitis is the most common gum disease, which is characterized by redness, bleeding of the gums, and swelling. According to statistics, only 3% of the population have completely healthy gums. To get into this percentage, you need to take care of your gums and regularly see a doctor so as not to miss the initial signs of the disease.
Gingivitis is a stage of gum disease when it is still possible to prevent the development of the inflammatory process and completely stop it. The next stage is periodontitis, in which inflammation spreads to the following periodontal tissues. After the onset of periodontitis, a complete cure is no longer possible; here we are talking about relieving the symptoms, bringing the disease into remission and delaying the situation when it is necessary to remove teeth. In this regard, it is necessary to be attentive to the health of the gums, to prevent their disease, and if problems arise, immediately consult a doctor to prevent serious damage to the periodontium.
Diagnosis of gingivitis
It is always important to collect a complete history of the disease, because gingivitis is often a chronic disease that occurs in childhood.6
It is also worth paying attention to the general condition of the body; the dentist may refer you to other specialists.
Consultation with an endocrinologist – in diseases of the endocrine system (diabetes mellitus, hyperfunction of the thyroid gland and adrenal glands), gum inflammation is more active.
Consultation with a hematologist – in case of blood diseases, gum inflammation is only a symptom of the underlying disease. Consultation with a hematologist is required for differential diagnosis and comprehensive treatment.
Consultation with a gastroenterologist – gingivitis is usually accompanied by chronic diseases of the digestive system.
Related doctors, in turn, prescribe a number of other tests to treat pathology, for example, a general blood test, biochemical blood test, gastroscopy, ultrasound, etc.
The dental office conducts diagnostic tests such as:
- Probing is a diagnostic method in which the characteristics of the attachment of the gums to the teeth are determined.
- Staining the gums with iodine-containing solutions: this shows whether the gums are inflamed. With gingivitis, the gums turn shades of brown.
- Determining the level of hygiene, that is, how well a person brushes his teeth.
- Panoramic X-ray of the teeth: This is necessary to see whether the inflammation has affected the bone or not, and also shows the condition of all teeth, fillings and crowns.
Prevention of gingivitis
It's always easier to prevent something than to treat it. Therefore, it is very important to follow the recommendations below:10
- You need to brush your teeth 2 times a day: morning and evening
- After each appointment, it is not necessary to brush your teeth, but you should rinse your mouth with water
- It is very important to use all personal hygiene products and do it correctly, you need dental brushes and dental floss
- Visit your dentist once or twice a year for a checkup and professional cleaning. It will remove plaque and be able to recognize gingivitis at an early stage
- Treat all concomitant diseases of the body.
- If installed structures in the mouth (fillings, dentures, braces) injure the mucous membrane, consult a doctor.
- Lead a healthy lifestyle: exercise, exercise, eat right
These measures will help you avoid gum disease and keep your mouth healthy.
Symptoms of gingivitis
- Bleeding gums are the main symptom of gingivitis. Bleeding can occur both while brushing your teeth and when eating. Spontaneous bleeding also occurs
- Swelling and swelling of the gums, which can make teeth appear smaller.
- Pain of varying severity
- Change in gum color: it becomes bright red or blue.
- Deterioration of general condition, fever, weakness, headache
The presence of symptoms and their severity depends on the form and severity of the disease.
Catarrhal gingivitis: symptoms and treatment
The main reason for its development lies in poor hygiene. Plaque accumulates on the surface of the teeth, including on their necks, which gradually hardens, turning into stone.
In addition to neglect of hygiene, catarrhal gingivitis can be caused by a lack of vitamin C in the body, hormonal imbalances and blood diseases. This form of the disease is the most common, occurring very often in women carrying a child.
The disease can be distinguished by the following symptoms:
- swelling of the gum edge, its redness or cyanosis;
- bleeding and pain during cleaning;
- plaque visible to the naked eye.
Catarrhal gingivitis can be:
- acute - this condition is characterized by the rapid development of symptoms;
- chronic, when the symptoms are mild, exacerbating only during periods of weakened immunity (for example, during a cold).
Catarrhal gingivitis: treatment in adults
Since the cause of gingivitis is plaque, the first step is to eliminate it. You can get rid of it by using a regular brush, but if the plaque has managed to mineralize and turn into stone, then you will have to spend time visiting the dentist.
Plaque mineralizes within less than 16 hours from the moment it forms: this is how tartar appears.
So, the main stages of treatment:
- Removing plaque and tartar. Ultrasonic cleaning has proven itself to be the best, after which it is imperative to undergo the procedure of polishing the teeth and treating the gums with gel. Typically, the total session duration is one hour. As practice shows, even after completing this stage of the treatment process, the patient feels much better.
- Anti-inflammatory therapy. Since catarrhal gingivitis affects only the surface of the gums, treatment can be carried out at home. It takes 10 days, then you will need to visit the doctor again for a follow-up examination. In most cases, anti-inflammatory gels are prescribed, which should be applied to the gums, rinses with Chlorhexidine, and a special toothpaste.
Description of anti-inflammatory therapy
For gingivitis treatment to be effective, it is recommended to treat the gums twice a day. Of the wide variety of gels, it is worth using “Cholisal Gel”, and using Chlorhexidine 0.05% as a rinse solution. The widely advertised Metrogyl Denta gel is slightly less effective.
The procedure is as follows: after waking up, routinely brushing your teeth (it is better to buy a Soft brush during treatment) and breakfast, you should thoroughly rinse your mouth with Chlorhexidine, then dry the surface of the gums with gauze and rub it with your finger. The gel should be applied both from the outside of the teeth and from the tongue. After treating your gums with gel, you should not drink or eat for at least half an hour. Some components of the product can cause salivation: saliva can be swallowed without fear, since it does not contain anything harmful to health.
It is necessary to clearly understand that curing gingivitis and then returning to your previous lifestyle means dooming yourself to the recurrence of symptoms in the near future. To prevent this from happening, prevention is important, which consists of properly brushing your teeth after every meal. Minimizing the risk of relapse is also influenced by the absence of caries, so carious cavities must be healed.