Pharyngitis is an inflammatory process that forms on the back wall of the larynx and affects the mucous membrane, as well as deeper layers, tissues of the soft palate and lymph nodes. The acute form of pharyngitis can develop into chronic if the patient does not seek help from a doctor and self-medicates.
Since the pathological process in the larynx is caused by the spread of pathogenic bacteria, the risk of developing pharyngitis increases in people with a weak immune system and in those who suffer from ENT diseases or are predisposed to them.
How dangerous is pharyngitis and how does it manifest itself? Which doctor should I contact and how to treat the disease? We will answer these and other questions in this article.
ICD - pharyngitis:
- J02 - acute pharyngitis
- J02.0 - streptococcal pharyngitis
- J02.8 - acute pharyngitis caused by other specified pathogens
- J02.9 - acute pharyngitis, unspecified
- J31.2 - chronic pharyngitis
- J31.1 - chronic nasopharyngitis
Pharyngitis is rarely isolated as a separate disease; the diagnosis is usually acute respiratory viral disease (ARVI).
ARVI is a general name; the doctor usually specifies how exactly ARVI manifests itself.
This may be rhinitis (runny nose), pharyngitis (red throat), nasopharyngitis (inflammation of the nose and throat), etc.1,2
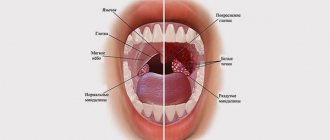
It is important not to confuse pharyngitis with tonsillitis.
To do this, let's understand the structure of the pharynx and oral cavity.
Structure of the pharynx
The pharynx is divided into 3 sections:
- upper (nasopharynx)
- middle (oropharynx)
- lower (larynx)
This division is very conditional, because There are no clear boundaries between departments. When inflammation occurs, it rarely happens that the inflammatory process is localized in one section; usually infectious processes spread and move throughout all sections of the pharynx5,7
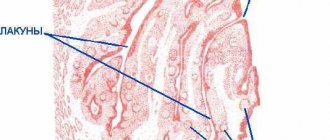
As can be seen in the picture below, the oropharynx is composed of the velopharyngeal arches, the uvula and the soft palate.
Pharyngitis usually affects:
- temples
- tongue
- soft sky
- posterior wall of the pharynx
The doctor uses a spatula to completely examine the pharynx. It is needed to improve visibility of the back of the throat.
The palatine tonsils also become inflamed with pharyngitis, because it is impossible to limit the inflammation process. This widespread nature of inflammation in pharyngitis distinguishes it from tonsillitis, where the tonsils are predominantly affected.
Afta Bednara
This is an inflammatory disease of the oral mucosa of a non-infectious nature, occurring in weak, bottle-fed infants in the first months of life.
Causes of the disease:
- permanent mechanical injury to the mucous membrane of the palate due to a nipple that is too long and too hard;
- may occur in breastfed children if the mother's nipple is very rough.
Main signs of the disease:
round or oval erosions, covered with loose plaque and located symmetrically at the border of the hard and soft palate, redness of the surrounding mucous membrane. The child becomes restless, eats and sleeps poorly.
In order to prevent the occurrence of the disease, it is necessary
promptly replace the pacifier or pacifier if irritation occurs on the oral mucosa.
If there are signs of disease, you should consult a pediatric dentist!
If any changes appear on the oral mucosa, you should visit a pediatric dentist to avoid complications and conduct a comprehensive examination and treatment!!!
How common is pharyngitis?
Pharyngitis, like a common ARVI (viral infection), occurs quite often. The incidence rate increases during the season from September to May, with a peak in February and March. A decrease in the incidence of pharyngitis by 3-5 times is observed in the summer months.10,11
Acute pharyngitis occurs more often in childhood than in adults. Children under 5 years of age suffer viral infections, including pharyngitis, 6-8 times a year.8,9
In the first year of visiting a preschool institution, the incidence of the disease is 10-15% higher than in children at home. But, unfortunately, “home” children subsequently get sick more often at school age.
Treatment
Treatment of herpetic stomatitis in children with mild and moderate forms is carried out on an outpatient basis. In severe cases and the development of complications, the baby is hospitalized. Treatment is carried out under the supervision of a pediatric dentist or periodontist.
Children are prescribed bed rest and a diet with pureed, non-irritating food. He is given separate hygiene items and dishes. Plenty of warm fluids are recommended.
The following drugs are prescribed:
- Non-steroidal anti-inflammatory drugs (Nise, Paracetamol, Nurofen) are used to relieve temperature and inflammatory reactions.
- Antihistamines (Clemastine, Loratadine) are used to relieve swelling of the mucous membranes.
- Antiviral drugs (Famciclovir, Acyclovir, Zovirax) are used at the beginning of treatment or in severe cases.
- Immunomodulators (Lysozyme, Gamma globulin, Thymogen) are used to enhance immunity.
During treatment, vitamin-mineral complexes and fish oil are used in monthly courses.
Local drugs that act directly on the mucous membrane are widely used.
For local treatment of herpetic stomatitis the following are used:
- antiseptics (Hexoral, Miramistin) - they are used to rinse the mouth every four hours for two weeks;
- ointments and gels with anesthetics (Kamistad, Lidochlor gel) are used for pain relief, they are lubricated with mucous membranes three times a day for up to two weeks;
- antiviral agents (Ganciclovir, Acicovir) - destroy the viral cell, gums are treated with these ointments five times a day, two weeks;
- proteolytic enzymes (Trepsin, Chymotrypsin) are used to cleanse the necrotic surfaces of ulcers; they are washed with these solutions twice a day.
- rinsing with decoctions of medicinal herbs (calendula, chamomile, sage) is carried out after each meal for up to two weeks;
- epithelializing ointments (Solcoseryl, Methyluracil) are used to enhance the healing of erosions and ulcers, used in the recovery stage, used up to four times a day for ten days.
Physiotherapy is applied locally. Irradiation of affected mucous membranes with ultraviolet and infrared rays is used.
Causes of pharyngitis and tonsillitis
Etiology (origin, cause) of pharyngitis. In 70-90% of cases, pharyngitis is caused by viruses. Pharyngitis can also be caused by bacteria, fungi, allergies, injuries, and exposure to irritating factors.
The most common viruses are rhinoviruses, adenoviruses, influenza, parainfluenza, enteroviruses, Coxsackie A, coronaviruses, a group of herpes viruses (Epstein-Barr virus, cytomegalovirus, HSV).12
There are pharyngitis, which are classified as a separate diagnosis depending on the pathogen, for example streptococcal pharyngitis ICD J02.0
Classification of pharyngitis
Pharyngitis can be acute or chronic. Acute is inflammation that just arose (suddenly), and chronic is a disease that persists for a long time, and it may not bother a person, but under certain circumstances again cause complaints and anxiety.3
| CLASSIFICATION | A COMMENT | ||
| classification: | Classification of pharyngitis due to its occurrence: | a comment: | viral bacterial fungal allergic traumatic caused by exposure to irritating factors caused by gastrointestinal diseases (gastroesophageal reflux, stomach diseases, etc.) |
| classification: | Pharyngitis associated with specific pathogens: | a comment: | Epstein Bar virus for infectious mononucleosis Yersinia enterocolitica for yersinial pharyngitis gonococcus for gonorrheal pharyngitis Leptotrix buccalis for leptotrichosis of the pharynx |
| classification: | Types of chronic pharyngitis: | a comment: | hypertrophic (enlargement of the mucous membrane) atrophic (depletion of the mucous membrane) catarrhal (standard inflammation) mixed |
Diagnosis of pharyngitis
Acute pharyngitis can be determined by patient complaints and examination of the oropharynx (pharyngoscopy).
Objective symptoms of pharyngitis, which are assessed by a doctor when examining the throat:
- swelling and hyperemia (redness) of the pharyngeal mucosa
- purulent or mucopurulent plaque on the walls of the pharyngeal mucosa
- the presence of inflammation in the arches, tonsils, orifices of the auditory tubes
- the presence of bright red tubercles on the back surface of the pharynx and on the side - hypertrophied (enlarged) lymphoid follicles
- thinning of the mucosa with areas of exfoliating epithelium, crusts and viscous mucus (atrophic pharyngitis)
Based on this, the doctor can make not only a diagnosis of pharyngitis, but also suggest its cause (viral inflammation, fungal infection, etc.).
Despite the fact that 70% of acute pharyngitis is a viral disease, sometimes it is necessary to exclude a bacterial cause. This is very important for further treatment tactics and prevention of complications. To do this, you should conduct a rapid test to exclude the streptococcal nature of pharyngitis.
In some cases, with fever, long-term complaints, or a temperature exceeding 3 days, it is also necessary to take a general blood test to understand the cause of acute pharyngitis.
Complications of pharyngitis
Acute pharyngitis usually responds well to treatment. The prognosis for viral pharyngitis is recovery.
Bacterial (streptococcal pharyngitis) can be complicated by the formation of a retropharyngeal abscess, and subsequently have a negative effect on the heart and kidneys, causing endocarditis and glomerulonephritis.
Symptoms of pharyngitis can persist even with proper treatment, if the true cause of pharyngitis is not eliminated. For example, if gastroesophageal reflux disease (damage to the gastrointestinal tract) is not treated, then pharyngitis will constantly remind itself.
Acute pharyngitis can become chronic.
Prevention of pharyngitis
To prevent pharyngitis, it is recommended:
- avoid hypothermia and dress appropriately for the weather
- avoid contact with tobacco and chemical irritants
- carry out frequent ventilation of working and living spaces
- walk outdoors more often. Walking will help strengthen the body's defenses in the fight against pharyngitis.
- don't drink ice water
- do not share food and cutlery, cups
- avoid crowded places and, if possible, stay in them for as little time as possible
- use disinfectants, including in public places,
- transport, etc.
- wash your hands often
Drug-induced stomatitis
Occurs when there is an allergy to a drug. Often, allergies can occur to antibacterial, antimicrobial drugs, vaccines, iodine. The mucous membrane is red, swollen, the lips and tongue also often swell, blisters appear, which burst, leaving erosion. The gums are inflamed and bleed when touched. General manifestations are possible, such as urticaria, nausea, vomiting. In severe cases, anaphylactic shock occurs (an emergency condition manifested by decreased blood pressure, shortness of breath, fainting, suffocation), Quincke's edema (an atypical reaction of the body, manifested by rapid and severe swelling)
Both conditions are extremely dangerous and require immediate action and calling an ambulance!
Pharyngitis in pregnant women
During pregnancy, a woman's body's protective properties decrease. In this regard, the risk of contracting infectious diseases, as well as exacerbation of chronic diseases, greatly increases.
Pregnant women need to carefully monitor their health and prevent diseases: avoid contact with people with respiratory diseases, avoid crowded places, wash your hands, eat regularly and properly.
If you develop acute pharyngitis or exacerbation of chronic pharyngitis, treatment is required. It is not recommended to use drugs that can affect the entire body. They can pass through the placenta to the baby and cause harm to him. To treat pharyngitis, pregnant women are advised to consult a doctor and use saline mouth rinses.
Causes of hematoma formation on the oral mucosa
The general scheme of hematoma formation is as follows: a rupture of a vessel causes the leakage of a certain amount of blood, followed by its compaction and the appearance of a blood clot. A bubble forms, noticeable on the smooth surface of the mucosa due to its dark coloring and relief. Often a similar picture can be observed during teething, when the gums bleed and become inflamed. The formation of multiple small hematomas, covering the entire surface of the mucous membrane in the mouth with unattractive dark spots, looks very unpleasant for the patient. But don’t panic if you suspect you have a serious illness. As practice shows, most of these phenomena occur due to mechanical trauma to the mucous membrane. But there are exceptions when the symptom indicates:
- allergic reaction;
- chronic injury;
- consequences of stressful situations;
- burns or cuts to the mucous membrane.
There have also been cases when multiple hematomas in the oral cavity are signs of:
- diabetes mellitus;
- hypertension;
- renal failure;
- complex types of stomatitis;
- blood diseases;
- vitamin deficiency, which causes fragility of blood vessels.
The exact cause and stage of formation of the pathology can only be determined after a thorough examination and diagnosis. For this reason, you should not self-medicate, so as not to further injure damaged tissues.
FAQ
Can pharyngitis be treated at home?
Pharyngitis usually does not require hospitalization (hospital treatment). You can treat strep throat at home on your own by using topical remedies to relieve sore throat and sore throat. If, after self-treatment, the sore throat does not go away within 3 days, then you should consult a doctor. If you have a fever in addition to a sore throat, you should immediately consult a doctor.
Which doctor should I contact if I have a sore throat?
If you have a sore throat, sore throat, or difficulty swallowing, you should first consult a therapist or pediatrician if you are a child. If there are indications, the doctor will prescribe a consultation with an ENT doctor.
Very severe sore throat. Are you sure I don't have a sore throat?
With pharyngitis, the pain syndrome may be more pronounced than with tonsillitis (tonsillitis). To treat pharyngitis, it is good to use a remedy that has an analgesic effect, for example Tantum® Verde. To exclude sore throat (streptococcal tonsillitis) or streptococcal pharyngitis, it is recommended to conduct a rapid test (streptotest).
Do you need an antibiotic for pharyngitis?
The antibiotic is indicated ONLY for bacterial pharyngitis. For a quick diagnosis, perform a rapid test for streptococcus. It will allow you to exclude or confirm the bacterial nature of pharyngitis. If streptococcus is detected, the doctor will prescribe antibiotics.
Is strep throat contagious?
Most often, strep throat is a viral disease, so a person can shed the virus and infect other people. A sick person is contagious, so you should stay at home until you recover.
What happens if pharyngitis is not treated?
Complications may arise. If pharyngitis is not treated, complaints persist much longer, inflammation does not go away and begins to become chronic.
Is it possible to get vaccinated for pharyngitis and when?
Against the background of an acute illness or exacerbation of chronic pharyngitis, vaccination is contraindicated. Wait until you have fully recovered and then you can get vaccinated. The exception is vaccination against influenza. It can be done when the temperature is normalized, i.e. There is no need to wait for all symptoms to disappear.
Is it possible to eat cold food if you have a sore throat?
If you have pharyngitis, it is not recommended to eat very cold foods, including ice cream. This can increase inflammation and slow down recovery.
A dental disease that causes a red rash in the mouth
Stomatitis is a disease that can cause the formation of red dots on the upper palate. This is an inflammatory process that occurs in the oral mucosa. It can be of fungal, viral or bacterial origin - it all depends on what specific pathogen has penetrated the mucous membrane.
Viral stomatitis
Caused by the herpes virus, small rashes appear not only on the palate, but also on the inside of the cheeks and lips, and tongue. The first two days of illness, the rash remains red and large, and then it transforms into blisters that are filled with serous fluid - clear or cloudy.
Viral stomatitis in each case is accompanied by elevated body temperature, weakness, lack of appetite and pain, a burning sensation in the mouth. This form of the disease is mainly diagnosed in adults and newborns.
Bacterial form of pathology
Most often, the oral mucosa is affected by staphylococcus and streptococcus. It is the latter that is considered the most dangerous, because it provokes various kinds of complications, including general blood poisoning. Bacterial stomatitis in almost every case ends with the development of tonsillitis, tracheitis or pharyngitis.
Red dots appear on the white palate, they never merge, but cause some discomfort to the patient: they itch, there is a burning sensation, the sensitivity of the mucous membrane to hot and cold, sour and salty increases. After a few days, the rash becomes barely noticeable, but the patient’s body temperature rises, and one of the above diseases rapidly develops.
Fungal stomatitis
Most often, the fungus affects the mucous membranes of those people who have weakened immune systems. In an adult, this can happen due to prolonged use of certain medications or a long course of the disease. Children often suffer from fungal stomatitis. “Thrush” develops due to constant licking of toys, pieces of furniture and imperfect immunity due to age.
There are not only red rashes in the mouth, but also a white coating. It is characteristic of this disease and helps to make an accurate diagnosis and prescribe effective treatment. Additional symptoms include pain and burning in the mouth, restlessness in a child, and a feeling of fatigue in an adult.