The term "tonsillitis" comes from the Latin name for the tonsils or tonsils. These are special paired rounded almond-shaped formations located on both sides between the palate and the root of the tongue, on the border of the oral cavity and pharynx. Their basis is lymphoid tissue; it is responsible for the maturation of lymphocytes (immunocompetent cells) and the development of an immune response with their help.
The palatine tonsils belong to the peripheral immune organs and, together with other tonsils, form the protective lymphopharyngeal ring of Pirogov-Waldeyer. Their task is to recognize and subsequently destroy pathogens and create an immune barrier at the level of the pharynx. Such protection works both against infectious agents penetrating from outside and against one’s own opportunistic flora.
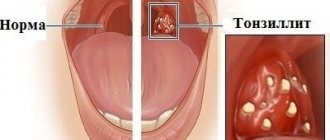
In most cases, this process is asymptomatic. But sometimes it is not possible to quickly destroy the pathogens; they begin to multiply in the natural recesses (crypts and lacunae) of the tonsils and provoke inflammation. This condition is called tonsillitis.
There are 2 forms of the disease:
- Acute tonsillitis or tonsillitis, the duration of the disease usually does not exceed 10–14 days. The nature of the inflammation can be catarrhal, follicular or lacunar. After the pathogen is destroyed, all symptoms of the disease are leveled, and the tonsils are cleared and return to their previous state.
- Chronic tonsillitis, characterized by prolonged inflammation of the tonsils. The tonsils are enlarged, and a purulent-microbial (caseous) substrate is constantly preserved in their recesses.
Chronic form of tonsillitis, why the tonsils become inflamed
Infection is the main cause of inflammation of the tonsils. The acute form of the disease in 70% of cases is caused by viruses, the remaining 30% is caused by bacterial and fungal flora. Therefore, sore throats most often accompany acute respiratory infections and are seasonal.
Damage to the tonsils in chronic tonsillitis in 80% of cases is of a bacterial nature. The main causative agents of the disease:
- β-hemolytic streptococcus.
- Group A streptococcus.
- Staphylococcus aureus.
- Haemophilus influenzae.
- Rarely encountered bacteria: mycoplasma, chlamydia, etc.
Viruses in the chronic form of the disease have a predominantly provocative, destabilizing effect. Acute and chronic recurrent viral infections weaken the immune defense, which creates conditions for the activation of bacterial flora. Hypothermia, acute intoxication, and ingestion of cold or irritating food lead to the same result.
When to see a doctor
Frequent cases of sore throat, prolonged recovery from respiratory infections, and persistent cough are reasons to immediately seek help from an otolaryngologist. The specialist will not only conduct a comprehensive diagnosis of the body, but will also tell you how to quickly and without consequences cure chronic tonsillitis. For additional consultations and examinations, you can contact the doctors of JSC "Medicine" (clinic of academician Roitber) in the central district of Moscow at the address: 2nd Tverskoy-Yamskaya lane, 10 (metro stations Mayakovskaya, Belorusskaya, Novoslobodskaya, Tverskaya, Chekhovskaya) . Experienced ENT doctors will offer an effective course of treatment for tonsillitis, taking into account the age and characteristics of the patient’s body. The selection of antibiotic drugs and physical therapy will be made based on the results of the examination and a history of diseases.
Features of the chronic form of the disease
Chronic inflammation of the tonsils can have several clinical variants:
- Latent form, when the patient does not experience significant discomfort in the throat and does not experience signs of exacerbation of the disease. Such people consider themselves healthy and are not aware of the dormant infectious-inflammatory focus in their throat.
- Periodically relapsing type of disease. Sluggish exacerbations and episodes of clearly defined inflammation of the tonsil itself, adjacent palatine arches and the pharyngeal wall are possible. Between periods of exacerbation, the inflammatory process subsides, but is not completely eliminated.
In chronic tonsillitis, the drainage and natural self-cleaning of crypts (folds) and lacunae (recesses) are disrupted in the tonsils; pus, living and dead bacteria, and toxins are constantly stored in their depths. This maintains constant inflammation, overstimulates sentinel immune cells, and provokes toxic-allergic reactions.
The immune response that forms during chronic tonsillitis is not sufficient to completely suppress the infectious process; it only restrains the activity of pathogens. Disruption of this delicate balance leads to exacerbation of the disease or triggers immune disorders.
Causes of tonsillitis
The most common causative agent of tonsillitis is hemolytic streptococcus. Less commonly, staphylococci and other bacteria, viruses or fungal infections become provocateurs. With a long and severe course of the disease or improper treatment, the tonsils themselves become a source of infection.
The tonsils contain a large number of lacunae - depressions into which food particles fall. This food serves as a favorable environment for the growth of bacteria, forms plugs and becomes inflamed.
Risk factors contributing to the development and maintenance of inflammation in the tonsil area:
- hereditary predisposition;
- stress;
- malnutrition;
- deviated nasal septum;
- adenoids;
- characteristics and living conditions (duration of cold weather);
- frequent colds;
- dustiness, air pollution;
- tonsil injuries;
- pathologies of the autonomic nervous system;
- allergization of the body.
Tonsillitis can also be a cause of decreased immunity. A healthy body immediately eliminates pathogenic viruses and bacteria, and they do not have time to cause harm. If you have frequent colds or respiratory diseases, it is worth visiting a doctor to understand the reasons for the decrease in immunity.
Pathogens can enter the mucous membranes of the tonsils and provoke inflammation in several ways:
- Airborne path. From sick people or carriers of infection who do not have symptoms, bacteria with droplets of mucus and saliva enter the air and spread within a meter when talking, coughing, sneezing, or screaming.
- Food route. When eating foods that contain pathogenic bacteria, they can settle on the tonsils, causing inflammation. Dairy and protein dishes and eggs are especially dangerous.
- Contract transfer. When sharing spoons, forks, mugs, or using the same hygiene items, bacteria enter the oropharynx and tonsils.
- Endogenous distribution. Pathogens are brought by blood or lymph flow from other places where there is infection (otitis media, sinusitis, caries, periodontal pathology).
Why treat chronic tonsillitis?
Chronically inflamed tonsils become a constant source of infection. With a decrease in immunity, it can spread to other tonsils and peripharyngeal tissue, invade the nasal cavity and paranasal sinuses, and descend into the underlying parts of the respiratory tract.
But the inflammatory reaction of the tonsils is not the main problem of chronic tonsillitis. Constant irritation of the immune forces not only weakens the protective response, but also creates the preconditions for the occurrence of abnormal reactions. Antibodies appear in the body, which are initially produced against β-hemolytic streptococcus, but show aggression towards connective tissue.
This secondary pathology is called rheumatism or Sokolsky-Buyo disease. It is a systemic acquired disease with an autoimmune mechanism, with the favorite targets for antibodies being heart valves and the synovium of small joints.
The key focus of streptococcal infection and the site of primary formation of rheumatic autoantibodies is the inflamed tonsils. Therefore, competent treatment of chronic tonsillitis is an effective prevention of rheumatism and its complications.
Symptoms of tonsillitis in adults
Acute tonsillitis or tonsillitis often occurs as a separate disease, or becomes a consequence of exacerbation of chronic tonsillitis. Possible causes may be overwork, decreased immunity, or hypothermia. Symptoms of acute tonsillitis or tonsillitis include:
- painful sensations in the throat, especially during swallowing;
- increase in body temperature up to 39 °C;
- redness, enlargement, swelling of the tonsils, redness of the palatine arches;
- the presence of purulent plugs on the tonsils;
- headache;
- enlargement and tenderness of the cervical and submandibular lymph nodes;
- general weakness;
- nausea, loss of appetite, drowsiness.
On a note!
Sore throat and dry cough: what disease is this “couple” talking about?
How to be treated correctly
Competent treatment of chronic tonsillitis includes a set of measures to eliminate infectious inflammation and deep sanitation (cleansing) of the tonsils. This is necessary to prevent relapses of the disease, suppress allergic and autoimmune processes, and restore the protective function of the pharyngeal lymphadenoid ring.
Common mistakes when treating tonsils:
- Only local medicine for sore throat is used, with the rejection of recommended systemic antibacterial therapy.
- The drug is selected by the patient independently, without taking into account the nature of inflammation, composition and sensitivity of the microflora.
- Drugs for the treatment of chronic tonsillitis are taken haphazardly, or instead of recommended medications, a folk remedy for the disease is used.
- Early cessation of treatment, therapy is completed soon after the sore throat subsides and other symptoms of exacerbation decrease.
- Avoidance of treatment between periods of exacerbation, refusal of proposed surgery.
- Late visit to the doctor, at the stage of complications.
This approach is the main reason for the protracted and complicated course of the disease and the formation of drug resistance in pathogens. Treatment of chronic tonsillitis in adults should be carried out comprehensively, under the supervision of a physician.
Risk factors
The risk of developing chronic tonsillitis of the throat increases if the patient has a hereditary predisposition to the disease. About 3% of all recorded cases are transmission of the inflammatory process from parents to children. Also, the protracted course of infectious diseases is caused by formations in the nasal cavity, polyps and sinusitis. The source of infection can be a carious tooth, gum disease, or periodontitis. Additionally, the body is weakened by poor nutrition, bad habits, constant stressful situations, and prolonged use of potent drugs.
Treatment without surgery
Conservative treatment includes general and local drug therapy, physiotherapy, lavage of lacunae and other methods of cleansing the tonsils. Antibacterial, anti-inflammatory, antiallergic, and immunomodulatory agents are prescribed.
Conservative therapy is widely used in modern otorhinolaryngology. But it does not always completely cure tonsillitis. The tonsils may remain enlarged even after drug suppression of the infection and deep cleansing; the risk of relapses and complications remains. In approximately 1/3 of patients, it becomes necessary to treat the disease surgically.
Operations for tonsillitis: from traditional methods to modern techniques
Indications for surgical treatment:
- The presence of episodes of exacerbation of the disease 2 or more times a year, with a predominance of purulent inflammation.
- Frequent (more than 4 times a year) exacerbations of tonsillitis, even if they occur without complications.
- Exacerbations are rare, but there are signs of complications from the heart, joints, kidneys or other organs.
- The disease is latent (hidden), but has become the cause of the development of rheumatism and other systemic diseases.
For a long time it was believed that chronically inflamed tonsils should be completely removed. This operation is called tonsillectomy. It allows you to eliminate the source of infection, but makes an uncorrectable hole in the protective lymphoid ring of the pharynx.
Currently, tonsillectomy is rarely performed, mainly in cases of severe purulent-destructive changes in the tonsils. In all other cases, ENT doctors give preference to organ-preserving operations, trying to leave an island of functionally active tonsil tissue.
But resection (partial cutting off of the tonsils) carries the risk of relapse of the disease. After all, such a procedure does not guarantee the elimination of all inflamed and infected tissue. The use of a laser improves the result due to an additional disinfecting and immunomodulating effect in the surgical area, but still does not completely solve the problem of relapses. Nevertheless, laser technologies are recognized as a priority in the treatment of tonsillitis.
Treatment of tonsillitis in adults
When the first signs of a sore throat or exacerbation of a chronic process appear, you need to contact an ENT doctor and treatment under his guidance. Self-medication is unacceptable - it threatens the development of dangerous complications, including autoimmune organ damage.
Diagnostics
To identify typical signs of inflammation of the tonsils, the doctor performs pharyngoscopy - examination of the pharynx and tonsils using a spatula and a light. It reveals typical signs of tonsillitis - enlargement, swelling of the tonsils, plaque or purulent plugs. The doctor can also examine the tonsils using a spatula, magnifying glass, probe to determine the nature of the lesion in the crypts (recesses), remove plaque to evaluate the tissue of the tonsils underneath them. He takes samples of discharge for examination (smears to exclude diphtheria, cultures for flora, counting microbial bodies in a smear).
Blood and urine tests are important to confirm infection and rule out damage to internal organs. In the blood test, leukocytes and ESR are elevated, there are changes in the leukocyte formula.
The level of antibodies to streptococcal antigens is also determined. An increase in the level of antibodies to streptolysin-O by more than 200 IU/ml indicates a streptococcal nature.
Modern methods of treatment
The main method of treating tonsillitis is local therapy. For tonsillitis of bacterial origin, antibiotics are prescribed.
General prevention includes hardening, physiotherapeutic procedures, and outdoor exercise. However, these procedures cannot be performed during an exacerbation of the disease, but only during remission.
Treatment regimen for tonsillitis
In general, the treatment plan is developed by the doctor. It determines the duration of the course of antibacterial drugs and their type, as well as the frequency of treatment of the tonsils, the necessary solutions, and additional methods of therapy.
Anti-inflammatory and analgesic drugs are used in treatment (OKI granules or rinse solution, Tantum Verde, Stopangin, Neo-angin, Faringosept).
show more
At temperatures above 38.6 °C, antipyretic drugs are used (Nurofen, Ibuklin, Paracetamol).
show more
If swelling of the tonsils is severe, antihistamines (Suprastin, Cetrin, Loratadine, Kestin) can be used.
show more
What antibiotics can be used for tonsillitis?
For tonsillitis, broad-spectrum antibiotics are used. The most effective in this case are amoxiclav (Augmentin), azithromycin (Sumamed), clarithromycin (Klacid). If standard therapy is not effective, the doctor changes antibiotics based on flora culture data.
How to gargle for tonsillitis?
Antiseptic, anti-inflammatory and analgesic agents are used for gargling. These can be Chlorhexidine, Miramistin, Furacillin, OKI solution, Chlorophyllipt. It is also acceptable to gargle with saline solutions or a salt-soda mixture.
Surgical treatment of tonsillitis
If therapy is ineffective and complications of tonsillitis develop, surgical treatment is resorted to. In most cases, tonsil removal leads to an improvement in general condition. But today, radical removal of tonsils is treated with extreme caution; these are important organs of the immune system, and their removal is used only in extreme cases.
Folk remedies for treating tonsillitis
Tonsillitis is a serious disease. His treatment must be comprehensive. Folk remedies should only be taken in conjunction with drug therapy. In addition, before using any traditional methods, you should first discuss their use with your doctor. No attempts at self-medication are acceptable.
To the point
Sore throat in adults: what symptoms besides a sore throat should alert you