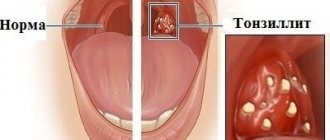
There is hardly a person who has not suffered from tonsillitis at least once in his life. The causative agents of tonsillitis are staphylococci, streptococci and pneumococci. There are acute tonsillitis and chronic tonsillitis.
Acute tonsillitis (or tonsillitis) is an infectious disease that affects the palatine tonsils, as well as the lingual, laryngeal and nasopharyngeal tonsils.
In acute tonsillitis, the throat hurts, it is difficult to swallow, the body temperature rises, general weakness, chills, aching joints, and headache appear. With proper treatment and compliance with the instructions of the otorhinolaryngologist, the disease is cured in 5-7 days.
1
Diagnosis of chronic tonsillitis in MedicCity
2 Diagnosis of chronic tonsillitis in MedicCity
3 Diagnosis of chronic tonsillitis in MedicCity
Chronic tonsillitis is a common infectious disease in which the focal infection is in the palatine tonsils. The formation of a chronic inflammatory focus in the tonsils occurs due to prolonged exposure of microbes to the lymphoid tissue of the tonsils.
Chronic tonsillitis is characterized by periodic exacerbations - sore throats, but a non-angina form of the disease also occurs.
Tonsillitis in children
According to statistics, almost half of weakened children fall ill with acute tonsillitis (tonsillitis). The tonsils in children begin to become very inflamed; the enlarged tonsils cease to perform their function - to protect the body and produce active substances that can suppress infection that penetrates from the outside.
Acute tonsillitis in children leads to fever, headache, weakness, loss of appetite, and inability to swallow food due to severe sore throat as a result of inflammation of the tonsils. Purulent plaque on the tonsils explains the putrid odor from the mouth. With tonsillitis, the tonsils in children decrease or increase in size, plugs appear in the tonsils, scars appear, and the lacunae of the tonsils are enlarged.
Why is tonsillitis dangerous?
Chronic tonsillitis is very dangerous: if you do not consult a specialist in a timely manner and self-medicate, complications may develop, among which the most dangerous are diseases of the heart and blood vessels, and rheumatic joint damage.
Tonsillitis in adults often leads to damage to the kidneys ( tonsillorenal syndrome ) and heart ( tonsillocardiac syndrome ). This is due to the fact that infectious and toxic factors that damage internal organs enter the body from the palatine tonsils. Streptococcus, for example, secretes a toxin, the effects of which can cause myocardial dystrophy and heart disease or rheumatism . In addition, purulent contents entering the gastrointestinal tract from the lacunae of the tonsils can provoke dysbacteriosis.
Causes, main risk factors
Up to 30 different colonies of pathogenic microbes can be sown on the surface of the tonsils of patients suffering from chronic tonsillitis. But in crypts and lacunae staphylo- or streptococcus is usually determined. A key role in the pathogenesis of chronic tonsillitis is played by beta-hemolytic strains of streptococcus (type A). Other flora - gram-negative coccal, fungal, viral - have an impact on local immunity, they support inflammation.
There are a number of factors contributing to the occurrence of the disease:
- hypothermia;
- decreased immunity;
- microtrauma of the tonsils;
- foci of inflammation in the mouth and in the head area (caries, sinusitis, adenoids, etc.);
- smoking;
- poor nutrition;
- allergy.
Viruses and bacteria that cause tonsillitis can come from the external environment.
Prerequisites for the development of tonsillitis
The palatine tonsils, nasopharyngeal tonsil, lingual and tubal tonsils form a protective ring (lymphoepithelial ring of Pirogov) - a powerful barrier to the air and food entering the body. The tonsils do a great job - they recognize dangerous viruses and bacteria in the air and food and trigger an immune reaction.
When examining the tonsil on its surface, you can see depressions and openings with narrow, winding and deep passages (the so-called tonsil lacunae).
| 1 - crypt (lacuna); 2 - lymphoid follicles; 3 - connective tissue capsule; 4 - mouth of the lacuna (crypt). | |
The existence of deep lacunae creates the prerequisites for the development of chronic inflammation of the tonsils. Remains of food, dead immune cells, etc. settle in the gaps, which are an excellent breeding ground for the proliferation of pathogenic microorganisms.
Features and causes of the disease
Tonsillitis occurs in acute (angina) and chronic forms. The peak incidence occurs in the autumn or spring. Children get sick twice as often as adults. Due to the structural features of the organs of the peripheral immune system, which include the tonsils of the peripharyngeal ring, they often do not perform a protective function, but themselves become a source of infection due to constant inflammation in them.
Tonsillitis occurs due to a weakened immune defense and in the presence of provoking factors. The development of the disease is promoted by:
- hypothermia of the body;
- bad habits: smoking and alcohol abuse;
- hypo and vitamin deficiencies;
- throat injuries;
- chronic inflammatory diseases of the nasal and throat cavities, paranasal sinuses;
- uncontrolled use of hormonal drugs;
- hereditary predisposition to throat diseases;
- hypoplasia of lymphoid tissues and other causes.
The disease can also provoke impaired nasal breathing and concomitant somatic diseases of various organs and systems that affect the overall reactivity of the body.
The causative agents of inflammation of the palatine tonsils are most often adenoviruses, coccal flora (streptococci, staphylococci), chlamydia, rhinoviruses, herpes viruses, parainfluenza.
Symptoms of tonsillitis
There are simple and toxic-allergic forms of tonsillitis. The simple form is characterized by only slight chronic inflammation of the tonsils, without a pronounced general reaction of the body.
In the toxic-allergic form, there are not only local signs of chronic inflammation, but sore throats, paratonsillitis, paratonsillar abscesses, as well as disorders in other systems (cardiovascular, genitourinary, etc.) develop.
General manifestations:
- fast fatiguability;
- lethargy;
- headache;
- elevated body temperature.
Local manifestations:
- discomfort in the throat when swallowing;
- sore throat;
- putrid odor from the mouth;
- formation of purulent-caseous “plugs” in the lacunae of the tonsils;
- dry cough;
- frequent sore throats;
- enlarged and painful regional lymph nodes.
EPIDEMIOLOGY
The prevalence of chronic tonsillitis among the population varies widely.
In adults it ranges from 5–6 to 37%, and in children – from 15 to 63%. In the group of frequently ill children, chronic tonsillitis is 40% or higher. It must be borne in mind that between exacerbations, as well as in the nonanginal form of chronic tonsillitis, the symptoms of the disease are largely familiar and little or do not bother the patient at all, which significantly underestimates the actual prevalence of the disease. Often chronic tonsillitis is detected only in connection with the examination of the patient for some other disease, in the development of which chronic tonsillitis plays a large role. In many cases, chronic tonsillitis, remaining unrecognized, has all the negative factors of a tonsillar focal infection, weakens a person’s health, and worsens the quality of life.
ETIOLOGY AND PATHOGENESIS
Etiology
Among the bacterial flora that constantly grows in the palatine tonsils, the causative agents of tonsillitis can be streptococci, staphylococci and their associations, pneumococci, H. influenzeae, M. Catarrhalis.
The main etiological factor in the development of chronic tonsillitis and its complications remains group A beta-hemolytic streptococcus.
According to foreign and domestic researchers, in the etiology of chronic tonsillitis its share is 30% in children and 10–15% in adults. Streptococci of serological groups C and G are less common.
Next in frequency of occurrence are Staphylococcus aureus, hemolytic Staphylococcus and obligate anaerobic microorganisms; intracellular and membrane parasites (chlamydia, mycoplasma), often detected in chronic tonsillitis, deserve special attention.
A lot of data has been accumulated on the frequent connection between two factors in chronic tonsillitis: streptococcal infection and predisposition to it.
In families of patients with chronic tonsillitis, there is a higher frequency of carriage of streptococcal infection and the prevalence of chronic tonsillitis than in the general population.
Risk factors for chemotherapy:
- age;
- climatic and geographical conditions;
- state of local and general immunity;
- the frequency of respiratory diseases that lead to the loss of the normal structure of the lymphoid organ and the development of hypoxic changes;
- childhood infections: measles, scarlet fever, chicken pox;
- malnutrition and poor living conditions;
- state of the environment, including the level of air pollution from industrial waste;
- carious teeth, chronic purulent sinusitis, difficulty nasal breathing (hypertrophic rhinitis, adenoids).
Pathogenesis
According to pathogenesis, two forms are distinguished:
a) chronic tonsillitis as a consequence of repeated sore throats suffered in childhood, which disrupted the mechanisms of tissue immunity and created favorable conditions for the constant vegetation of pathogenic flora in the palatine tonsils;
b) primary developing chronic tonsillitis without acute anginal excesses.
Both forms of development of chronic tonsillitis are caused by a number of external and internal reasons.
In healthy people, various microorganisms are constantly present in the lacunae of the tonsils; this is where the presentation of antigens (AG) and the induction of an immune response occur. In the lacunae, Ags are recognized, phagocytosed and presented to B and T cells of the lymphoid tissue of the tonsils, where antigen-specific T and B cell reactions develop. Under normal conditions, microorganisms (MO) living on the mucous membrane of the oropharynx cannot penetrate into the deep layers of tissue and develop an infectious-inflammatory process.
The introduction of MO is due to the synthesis of invasive enzymes, which is possible during the formation of dysbiosis of the mucous membrane due to various unfavorable factors, the main of which is the inhibition of specific and nonspecific factors of the natural resistance of the macroorganism.
According to many researchers, one of the factors in the occurrence of chronic tonsillitis is the anatomical structure of the palatine tonsils, in particular the presence of deep crypts in which associations of pathogenic flora accumulate, multiply and have a necrobiotic effect on the surrounding lymphadenoid tissue.
An important condition for the development of chronic inflammation in the palatine tonsils is the anatomical conditions in which they are located: covering the lacunae with triangular and semilunar folds, deep niches of the palatine tonsils and their pinching between the anterior and posterior palatine arches, the presence of additional niches in which tonsil tissue is located. Under these conditions, the mucous glands that produce washing and disinfecting mucus cease to perform this important role due to obstruction.
Another factor contributing to the development of chronic tonsillitis is impaired nasal breathing. Inhaling cooled air through the mouth or drinking cold drinks plays a dual pathogenetic role - it directly affects tissue biochemical processes (reduces or even stops them) and causes a number of physiological reactions (cold vascular spasm, reflex disturbance of the autonomic regulation of trophic functions). In the pathogenesis of chronic tonsillitis, a significant role is played by violations of the protective mechanism that delimits the source of inflammation. When the barrier function is partially or completely lost, the focus of inflammation turns into an entrance gate for infection, and damage to a number of other organs and systems becomes possible, which is determined by the reactive properties of the body.
Speaking about the pathogenesis of chronic tonsillitis, it is also important to note that the natural role of the palatine tonsils in the formation of immunity is completely distorted, because with chronic inflammation in the tonsils, new antigens are formed under the influence of pathological protein complexes (virulent microbes, endo- and exotoxins, products of destruction of tissue and microbial cells, etc.), which causes the formation of autoantibodies against one’s own tissues.
Chronic tonsillitis often causes the development of other diseases or aggravates their course. Numerous studies conducted over the past decades confirm the connection of chronic tonsillitis with rheumatism, polyarthritis, acute and chronic glomerulonephritis. sepsis, systemic diseases, dysfunction of the pituitary gland and adrenal cortex, neurological diseases, acute and chronic diseases of the bronchopulmonary system, etc.
CLASSIFICATION
In domestic medicine, two classifications of chronic tonsillitis that have practical significance are most widespread: I.B. Soldatova (1975) with the division of chronic tonsillitis into compensated and decompensated forms.
The compensated form of chronic tonsillitis is characterized by local signs of chronic inflammation of the tonsils without a pronounced general reaction, a history of periodic acute streptococcal tonsillopharyngitis (no more than once every 1–2 years) or a nonanginal course of inflammation; the decompensated form is characterized by frequent ATP (several times a year), history of paratonsillitis and paratonsillar abscesses, the presence of associated (metatonsillar) diseases.
B.S. Preobrazhensky and V.T. Palchuna (1964) with a division into a simple form and two toxic-allergic forms.
The simple (compensated) form of chronic tonsillitis is characterized by the absence of a visible reaction from the whole organism, exacerbations (repeated tonsillitis) and occurs only with local symptoms, subjective complaints and objective (local) signs of the disease.
Toxic-allergic forms occur with local and general complications.
Toxic-allergic form I (TAF 1) is characterized by a history of periodic sore throats, all the above-mentioned signs of a simple form of chronic tonsillitis in combination with general toxic-allergic phenomena.
Toxic-allergic form II (TAF II) is characterized by more pronounced signs of the first toxic-allergic form.
DIAGNOSIS
Clinical signs and symptoms
Patients with chronic tonsillitis complain of frequent acute streptococcal tonsillopharyngitis, discomfort in the throat, discharge of “purulent” plugs and bad breath.
In chronic tonsillitis, moderate symptoms of general intoxication are observed - such as periodic or constant low-grade body temperature, sweating, increased fatigue, incl. mental, sleep disturbance, moderate dizziness and headache, loss of appetite, etc.
One of the most reliable signs of the disease is the presence of a history of acute streptococcal tonsillopharyngitis. In this case, it is necessary to find out the frequency and severity of ATP from the patient.
Physical examination
There is no pathognomonic symptom of chronic tonsillitis.
The diagnosis of chronic tonsillitis is established based on the presence of several subjective and objective signs of the disease.
Local signs
The most reliable local signs of the disease:
- hyperemia and roller-like thickening of the edges of the palatine arches;
- cicatricial adhesions between the tonsils and palatine arches;
- loosened or scarred and hardened tonsils;
- caseous-purulent plugs or liquid pus in the lacunae of the tonsils;
- regional lymphadenitis – enlargement of the cervical lymph nodes.
General signs:
- low-grade fever (intermittent);
- tonsillogenic intoxication (weakness, weakness, fatigue, etc.);
- joint pain and functional disorders of the heart against the background of tonsillogenic intoxication.
Clinical and diagnostic characteristics of individual forms of chronic tonsillitis are presented in table. 1.
Possible regional diseases caused by chronic tonsillitis:
- paratonsillar, parapharyngeal and retropharyngeal abscesses;
- cervical lymphadenitis;
- mediastenitis;
- inflammation of the middle ear and paranasal sinuses.
Common diseases:
- Acute and chronic tonsillogenic sepsis.
- Rheumatism, the formation of heart defects.
- Glomerulonephritis.
- Infectious nonspecific polyarthritis.
- IgA nephropathy.
- Psoriasis.
- PANDAS – pediatric autoimmune neuropsychiatric associated with streptococcal infection (children's autoimmune neuropsychiatric disorders associated with streptococcal infection).
- Movement disorders (chorea, tics, dystonia, parkinsonism).
- Mental disorders (especially emotional).
- Sleep disorders.
- Infectious and allergic diseases of the urinary system, joints and other organs and systems.
Examples of diagnosis formulation:
- Chronic tonsillitis, simple form.
- Chronic tonsillitis, toxic-allergic form of the II degree, rheumatism in the inactive phase.
Laboratory and instrumental studies
Basic laboratory tests:
- Complete blood count - hypochromic anemia, neutrophilic leukocytosis, monocytopenia, leukopenia, and increased ESR can be detected. However, more often chronic tonsillitis is not accompanied by changes in the peripheral blood.
- Biochemical blood test (rheumatic tests) (SBR, RF, ASLO).
- General urine analysis.
- Bacteriological examination of the contents of tonsil lacunae (detection of pathogenic and opportunistic microorganisms and the most common pathogen - group A beta-hemolytic streptococcus).
Instrumental studies
Pharyngoscopy: the presence of local signs - liquid pus or caseous plugs in the lacunae, Giese's sign - hyperemia of the edges of the anterior arches, Zach's sign - swelling of the edges of the upper parts of the palatine arches, Preobrazhensky's sign - infiltration of the edges of the anterior arches, as well as fusion and adhesions of the tonsils with the arches.
Additional diagnostic measures:
- Cytomorphological study of discharge lacunae.
- Methods for specific diagnosis of infection caused by group A beta-hemolytic streptococcus.
- Immunoserological tests (determination of titers, anti-DNase B, antistreptokinase.
- ECG.
Differential diagnosis
In differential diagnosis, you need to keep in mind that some local and general signs characteristic of chronic tonsillitis can be caused by other foci of infection, for example pharyngitis, gum inflammation, dental caries. With these diseases, inflammation of the palatine arches and regional lymphadenitis can also be observed.
It is also necessary to carry out a differential diagnosis between chronic tonsillitis and non-inflammatory hypertrophy of the palatine tonsils. The size of the tonsils itself does not indicate chronic tonsillitis. In children, the presence of enlarged NM indicates only rapidly occurring processes of the formation of natural immunity. In rare cases, nonspecific chronic tonsillitis requires differential diagnosis with specific processes (tuberculosis, syphilis, etc.). With pronounced (especially unilateral) hypertrophy of the palatine tonsils, we must not forget about the likelihood of oncological and lymphoproliferative diseases (cancer, lymphosarcoma).
Differential diagnostic signs of chronic tonsillitis and chronic pharyngitis are given in table. 2.
TREATMENT
Non-drug treatment
The widespread prevalence and significant impact of tonsillar pathology on many human organs and systems determine the relevance of the problem of chronic tonsillitis. Considering the extremely important role of the palatine tonsils in the processes of immunogenesis, indications for tonsillectomy must be strictly defined. In the absence of absolute indications for tonsil removal, conservative treatment that preserves the immunological functions of the tonsil lymphoid tissue seems most appropriate.
Treatment must begin with sanitation of the mouth, nose and paranasal sinuses, pharynx, etc.
Surgery
Surgical treatment (tonsillectomy) is carried out in case of ineffectiveness of conservative therapy and in case of chronic tonsillitis, toxic-allergic form of the II degree.
With regard to indications for tonsillectomy, all patients can be divided into three groups:
The first, largest group includes patients who periodically experience exacerbations of the disease in the form of ATF, peritonsillar abscesses, which deprive them of their ability to work and gradually worsen their general condition.
The second group consists of patients with various diseases otologically and pathogenetically associated with chronic tonsillitis and its periodic complications. These are toisillogenic rhinitis, sinusitis, conjunctivitis, dacryocystitis, cervical lymphadenitis, pharyngitis, laryngitis, tracheobronchitis, gastroenteritis, appendicitis, colitis, etc.
The third group includes patients with metatonsillar complications that occur “at a distance”, caused by the presence of an infectious-allergic focus of infection in the palatine tonsils (infectious polyarthritis, cardiovascular and renal complications, damage to the nervous system, etc.).
If indicated, there is no alternative to tonsillectomy. In some cases, patients may undergo organ-preserving operations - if conservative treatment is ineffective, with a compensated form of chronic tonsillitis, with contraindications to tonsillectomy, with a decompensated form of chronic tonsillitis, and as a trial treatment for relative indications for tonsillectomy.
Drug treatment
Therapy for chronic tonsillitis, as a rule, includes a whole range of local and systemic therapeutic effects. An effective way is to wash the lacunae of the palatine tonsils (with a syringe, using hardware) with solutions of antimicrobial agents, treatment using the Tonsilor device, and physiotherapy. If the results are effective, courses of conservative therapy are carried out 1–3 times a year.
In addition, immunostimulating agents are used - bacterial lysates (for example, Imudon, lozenges). The use of local immunomodulators promotes faster relief of symptoms.
The inclusion of the drug Imudon® in the treatment regimen in patients with chronic tonsillitis is also characterized by restoration of the function of phagocytosis (decrease in indicators of incomplete phagocytosis) and a tendency to normalize antibody formation. Phagocytosis in the pathogenesis of infectious and infectious-allergic diseases is one of the key links in immune reactions that determine the outcome of diseases - recovery or chronicity.
According to indications, adaptogens, antioxidants, herbal remedies, immunotropic therapy, and homeopathic remedies are used.
The use of immunotropic therapy makes it possible to increase the effectiveness of complex treatment of patients with chronic tonsillitis. Among the wide variety of immunomodulators, one can highlight the drug Galavit (Selvim LLC, Russia), which has a multidisciplinary mechanism of action: immunomodulatory, anti-inflammatory, antioxidant, regenerative. The mechanism of the immunomodulatory action of Galavit is associated with the ability to selectively regulate (increasing or decreasing depending on the initial values) the functional and metabolic activity of innate and adaptive immune cells (monocytes, macrophages, neutrophils, natural killer cells, etc.). By enhancing the phagocytic activity of monocytes and macrophages, the bactericidal activity of neutrophils and the cytotoxic activity of NK cells in case of its initial deficiency, the drug increases the body’s nonspecific resistance to infectious diseases of bacterial, viral and fungal etiology, promotes faster elimination of the pathogen from the body, reduces the frequency, severity and duration infections. In addition, Galavit stimulates the production of endogenous interferons (IFN-α, IFN-γ) by producer cells; normalizes antibody formation, increases the functional activity of antibodies. Anti-inflammatory effect: realized by reversible (6-8 hours) inhibition of the production of pro-inflammatory cytokines (IL-1, IL-6, TNF-α) by hyperactivated monocytes/macrophages, reducing the severity and duration of the intoxication-inflammatory process. The antioxidant effect is realized through direct inactivation of a number of radical compounds, blocking the production of reactive oxygen species by hyperactivated macrophages, regulating the activity of antioxidant enzyme systems, thereby reducing the level of oxidative stress and protecting tissues and organs from the destructive effects of radicals. The drug helps to increase the production of growth factors by monocytes/macrophages at the site of inflammation and thus accelerate regeneration processes.
The results of clinical studies have confirmed the effectiveness of complex treatment of chronic tonsillitis with the inclusion of the immunomodulator Galavit in terms of increasing the efficiency of eliminating the infectious agent from the body, reducing the frequency of relapses, and increasing the duration of clinical remission.
Concomitant therapy
To increase the effectiveness of therapy, accelerate recovery and prevent exacerbations of chronic tonsillitis, the use of the immunomodulatory drug Anaferon/Anaferon for children is recommended. The drug stimulates the humoral and cellular immune response, increases the production of antibodies (including secretory IgA), the functional activity of phagocytes and natural killer cells (NK cells). When treating chemotherapy, Anaferon/Anaferon for children is prescribed as part of complex therapy in a dosage of 1 tablet once a day.
Evaluation of treatment effectiveness
The criteria for the effectiveness of treatment of chronic tonsillitis are: reducing the number of exacerbations, preventing the development of complications and associated diseases.
Complications and side effects of treatment
Complications and side effects of treatment correspond to the adverse side effects of drugs and treatment methods used to treat chronic tonsillitis.
FORECAST
With timely and adequate treatment, the prognosis is favorable. Without treatment, there is a high risk of developing systemic infectious and allergic diseases. It should be noted that pharmacotherapy for chronic tonsillitis TAF degrees I and II cannot guarantee relief from tonsillogenic intoxication and the development of systemic infectious-allergic complications, because the persistence of pathogenic microflora in the tonsils is not eliminated.
Diagnostics
Diagnosis of tonsillitis in children, as well as tonsillitis in adults, is carried out using the following methods:
- examination by an ENT doctor, collecting an anamnesis of the disease;
- throat swab for flora with determination of sensitivity to antibiotics and bacteriophages;
- general blood test, general urinalysis;
- blood test for antistreptolysin-O, rheumatoid factor, C-reactive protein;
- ECG;
- According to indications, ultrasound of the kidneys, Echo-CG, consultation with a cardiologist, urologist.
Treatment of chronic tonsillitis
Many people wonder: how to treat tonsillitis and is it really necessary to remove tonsils? The therapeutic tactics on which the treatment of tonsils depends depends on the form of the disease, the degree of dysfunction of the palatine tonsils and the presence of diseases associated with chronic tonsillitis.
Conservative treatment of tonsils
Conservative therapy consists of the following measures:
- sanitation of the upper respiratory tract (removal of adenoids, hypertrophic rhinitis, deviated nasal septum, sinusitis) and oral cavity (treatment of caries, gingivitis, etc.);
- prescription of means that help increase the body's defenses: (hardening procedures, daily routine, balanced nutrition, vitamin therapy, physical activity, spa treatment);
- prescription of hyposensitizing drugs;
- prescription of immunocorrectors;
- the use of reflex effects: acupuncture, manual therapy of the cervical spine;
- washing the tonsils with antiseptic solutions to remove the pathological contents of the tonsils (plugs in the tonsils, purulent masses);
- treatment with the “Tonsilor” device;
- introduction of medicinal substances into the lacunae (various emulsions, pastes, ointments, oil suspensions are introduced using a syringe with a cannula);
- lubrication of the tonsils (with solutions of protargol, collargol, oil solution of chlorophyllipt, Lugol, etc.);
- gargling with antiseptic solutions (performed independently by the patient);
- use of physiotherapeutic treatment methods.
1 Sanitation of the upper respiratory tract in MedicCity
2 Acupuncture of the cervical spine in MedicCity
3 Manual therapy of the cervical spine in MedicCity
Very effective in the complex treatment of tonsillitis is washing the lacunae of the palatine tonsils using vacuum aspiration. A similar device is equipped with a specialized ENT unit in the MedikCity otolaryngologist’s office. The essence of the procedure is mechanical cleansing with the help of a special nozzle under the influence of vacuum from the lacunae of the tonsils from caseous plugs and purulent discharge and subsequent treatment of the tonsils with an antiseptic. This procedure is not performed during periods of exacerbation of sore throat and other infectious diseases of the respiratory tract, as well as during acute toothache. Carrying out courses of 5-10 procedures twice a year allows patients to forget about relapses. If there is no effect after 2-3 courses, the issue should be resolved radically (tonsil removal).
Conservative treatment is carried out in courses and includes a combination of the methods listed above, which are selected individually.
Usually, to fully consolidate the result, 2-3 courses of treatment of 10 sessions each with an interval of 6-12 months are sufficient.
Operations for tonsillitis: from traditional methods to modern techniques
Indications for surgical treatment:
- The presence of episodes of exacerbation of the disease 2 or more times a year, with a predominance of purulent inflammation.
- Frequent (more than 4 times a year) exacerbations of tonsillitis, even if they occur without complications.
- Exacerbations are rare, but there are signs of complications from the heart, joints, kidneys or other organs.
- The disease is latent (hidden), but has become the cause of the development of rheumatism and other systemic diseases.
For a long time it was believed that chronically inflamed tonsils should be completely removed. This operation is called tonsillectomy. It allows you to eliminate the source of infection, but makes an uncorrectable hole in the protective lymphoid ring of the pharynx.
Currently, tonsillectomy is rarely performed, mainly in cases of severe purulent-destructive changes in the tonsils. In all other cases, ENT doctors give preference to organ-preserving operations, trying to leave an island of functionally active tonsil tissue.
But resection (partial cutting off of the tonsils) carries the risk of relapse of the disease. After all, such a procedure does not guarantee the elimination of all inflamed and infected tissue. The use of a laser improves the result due to an additional disinfecting and immunomodulating effect in the surgical area, but still does not completely solve the problem of relapses. Nevertheless, laser technologies are recognized as a priority in the treatment of tonsillitis.