Professional dental care includes the removal of caries, cystic areas and many other procedures. In accordance with the protocol for providing medical care, the dentist is also required to monitor the condition of the salivary glands
. In clinical practice, their damage is quite rare. Most often, poor performance of the excretory ducts occurs due to injury or incorrect oral therapy. Quite often this happens due to insufficient hygiene.
Bougienage or treatment of the salivary gland involves intubation of a dental instrument or probe in order to examine the organ and administer appropriate substances. Saliva contains a large number of enzymes that take part in the processing of food and the removal of metabolites from the body. If appropriate manipulations are not performed, this can lead to an increased likelihood of developing caries, pain when eating and a malfunction in the digestive system.
Indications for use
Bougienage of the salivary gland ducts is performed with the following symptoms:
- Unpleasant painful sensations.
- Sharp pain when eating certain foods.
- An involuntary feeling of fullness in the mouth after eating.
In case of malfunction of the excretory duct, you must immediately contact a specialist. Otherwise, the clinical picture may worsen, and the pathological process will become chronic.
Maxillofacial Surgery
Maxillofacial Surgery
- a branch of medicine that deals with the treatment of various diseases and injuries of the head and neck. The range of these pathologies can differ significantly from each other depending on the specific medical institution and the competence of the individual doctor, which leads to the fact that not only patients, but also doctors of other specialties do not know where to refer a patient with a “non-obvious disease”.
We will try to briefly describe what pathologies we will deal with at the S.V. Center for Cosmetology and Plastic Surgery. Nudelman.
Diseases of the oral mucosa
, incl. both potentially malignant diseases (various erosive and ulcerative lesions, “white” and “red” diseases of the mucosa), and an established diagnosis of squamous cell carcinoma.
Any ulcers, formations on the mucous membrane of the tongue, cheeks, lips, oropharynx, floor of the mouth.
Diseases of the salivary glands.
Benign tumors. Salivary stone disease. Systemic diseases associated with damage to the salivary glands (invasive diagnostics).
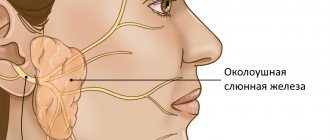
The appearance of formations or enlargement of large salivary glands - parotid (located “under the auricle, behind the lower jaw”), submandibular (under the lower jaw), sublingual (under the tongue).
Formation of soft tissues of the head and neck.
Skin formations and everything that is under it.
Congenital neck diseases.
The most common are thyroglossal duct cyst (median neck cyst), lateral neck cyst.
Long-term enlarged lymph nodes of the neck.
Diseases of the jaws. Cysts associated and not associated with tooth roots. Damages due to medication. Radiation damage to the jaws.
Abnormally positioned and supernumerary teeth.
Injuries of the upper and lower jaw, orbital walls, nasal bones.
Consequences of trauma to the bones of the facial skeleton and cranial vault.
Deformations and “retraction” of tissues and the eyeball (enophthalmos) due to a violation of bone anatomy.
Pain syndromes in the facial area.
Diseases of the temporomandibular joint.
Surgical treatment of endocrine ophthalmopathy.
A number of pathologies have a “vivid” clinical picture (for example, salivary stone disease), and a fairly clear and well-established treatment strategy. In other situations, it is necessary to “go to the diagnosis” for a long time and persistently, including invasive manipulations and operations to obtain cytological and histological material.
In all cases, the basis of treatment will be a correct diagnosis.
We actively discuss diseases that are at the “junction” of specialties, and there are definitely more than half of them. These consultations are carried out in our clinic and in some cases can be joint (neurologist, orthopedic dentist, orthodontist, ENT).
We carefully study imaging data (computed tomography and magnetic resonance imaging) with the involvement of leading specialists.
It is possible to discuss the case with your attending physician (oncologist, dentist, neurologist, rheumatologist).
This surgical procedure is aimed not only at “selecting” patients for surgical treatment, but also at “strategic” planning and long-term observation of diseases that are chronic in nature and require monitoring (photo recording of clinical manifestations, biopsy, etc.).
Pathology of the bones of the facial skeleton
Jaw formations
Operation options: - incisional surgical biopsy (taking a section of pathological tissue for the purpose of subsequent histological verification, if without this it is impossible to immediately determine the extent of the operation) - cystectomy - removal of the cyst membrane (if the formation is of such a nature), may differ in significant variability in volume, complexity and duration - cystotomy (cyst marsupilization) - an operation to create an anastomosis of the cyst cavity with the oral cavity - used both as an independent surgical intervention and in combination with a biopsy.
— partial resection of the jaw along with the tumor
Chronic osteomyelitis of the lower jaw (in the absence of an acute inflammation phase), incl. radiation and drug-induced injuries (depending on a number of conditions, the operation can be performed both under local anesthesia and general anesthesia)
— necro- or sequesterectomy (removal of altered bone tissue)
Abnormally located and supernumerary teeth - removal of abnormally located and supernumerary teeth under anesthesia
Diseases of the temporomandibular joint - arthrocentesis, lavage of the temporomandibular joint
Surgical treatment of endocrine ophthalmopathy - bone decompression of the orbit (outer, lower, medial wall and their combinations)
Injuries of the upper and lower jaw, orbital walls - osteosynthesis of the lower jaw (mainly through intraoral access) - osteosynthesis of the upper jaw - plastic surgery of the orbital walls
THERE ARE CONTRAINDICATIONS, SPECIALIST CONSULTATION IS REQUIRED
Diagnostic methods for bougienage of the salivary glands
- Sialometry. Allows you to conduct a quantitative and qualitative study of secreted unstimulated and stimulated saliva. With this technique, a special tube is inserted into the flow part.
- Radiosialography. The study is performed by filling the ducts with special substances. The saliva is then assessed for the presence of inflammation or an autoimmune disease. For contrast diagnostics, iodine-containing substances are often used.
- Pantomosialography. An innovative procedure that involves simultaneous contrasting of four salivary glands. With its help, it is possible to identify hidden pathological processes in the organ.
Additionally, X-ray diagnostics, thermosialography and other methods can be performed. It all depends on the symptoms of the disease and the characteristics of the inflammatory process in the oral cavity.
Causes
- The presence of inflammatory processes in the oral cavity
- Mechanical factors, for example, trauma to the ducts from sharp edges of teeth or crowns
- Stagnation of saliva secretion
Currently, there are four methods aimed at eliminating stones from the salivary glands.
1. Interventional sialendoscopy.
The doctor uses a special instrument with a camera at the end - an endoscope - to remove stones from the salivary ducts. This procedure is performed under local anesthesia.
2. Extracorporeal lithotripsy.
Under the influence of ultrasonic influence on stones, they are crushed.
Thanks to this method, it is possible to extract and wash the ducts with a special solution, which will prevent the development of the inflammatory process.
3. Dissection of the duct is done if the stone is large and cannot be removed using a simple method.
4. Extirpation of the salivary gland.
This operation is used only when irreversible changes are observed in the parenchyma of the gland. The doctor performs the procedure in a hospital setting under general anesthesia.
Common diseases of the salivary glands
- Narrowing of the flow channel. An inflammatory process or traumatic injury can lead to scarring of the tissue. As a therapy, a conical probe is inserted into the flow path. The number of sessions can range from 12 to 25 depending on the clinical picture.
- Chronic sialadenitis. In this case, the outlet flow channel does not work fully. This happens most often due to infection, the penetration of a pathogenic bacterial environment. Treatment involves drug therapy using antibiotics of the appropriate spectrum of action.
- Violation of the integrity of the duct. As a therapy, a probe is inserted into the cavity to prevent clogging of the duct and ensure normal patency.
These are the most well-known pathologies. There are other cases in clinical practice. Most often, a narrowing of the flow path with severe swelling is diagnosed. A full course of dilatation allows you to achieve the required therapeutic effect.
Sialendoscopy as a method for removing stones from the salivary gland
Chronic obstructive pathologies of the salivary glands can be caused by the presence of salivary stones, the formation of a mucus plug, duct stenosis, the influence of foreign bodies, or anatomical variations in the gland duct system, which can result in retention of saliva in the duct, discomfort, and even infection. Specifically, sialolithiasis is a condition in which a calcified mass forms in the salivary gland. Most often, this disorder is observed in the area of the submandibular gland (in the so-called “Wharton’s duct”) and can cause swelling and pain in the affected area, especially during stimulation of salivation. If the stone does not come out of the gland on its own, it must be removed surgically.
To diagnose such pathologies, methods of radiosialography, ultrasound examination and magnetic resonance sialography can be used. Radiosialography is the most common method for identifying stones in the salivary gland duct, but its use is contraindicated in cases of acute infection or if the patient is hypersensitive to the contrast agent. Ultrasonography is a first-line diagnostic method that allows non-invasively and without the use of contrast to visualize the presence of a calculus in the salivary gland. It should be remembered that the parameters of sensitivity and specificity of this method vary depending on the stage of mineralization of the stone. For diagnostic purposes, of course, you can use more expensive methods such as computed tomography, magnetic resonance imaging or scintigraphy.
Currently, sialoendoscopy is widely used as a non-invasive approach for diagnosing and treating pathologies of the salivary glands. This method allows for direct access to the gland duct, its expansion and irrigation, as well as to establish the presence or absence of patency of the duct.
In this article, we describe the clinical cases of two patients who underwent sialolithotomy procedures using a sialoendoscope at Korea University Anam Hospital. In addition, we will describe the differences between sialoendoscopy and other methods for diagnosing and treating sialolitis.
Clinical case 1
Patient Information
An 81-year-old female patient presented to the dental clinic with a sensation of a foreign body under her tongue and symptoms of dry mouth. She was previously diagnosed with thyroid carcinoma in June 2003 and underwent a total thyroidectomy procedure. The patient's medical history included hypertension and chronic kidney disease. The stone was identified in the duct of the right submandibular gland (Figure 1).
Figure 1. Salivary stones measuring 2 × 10 mm were identified in the right submandibular gland using CBCT.
Surgical procedure
The working area was treated with betadine. After disinfection, the oral cavity was washed generously with saline solution. Local anesthesia was performed in the area of the tongue and floor of the mouth with a 2% lidocaine solution with an epinephrine concentration of 1:100,000. Afterwards, the tongue was sutured with 3-0 silk thread in order to provide optimal conditions for the operation. Using a microscope, the entrance to the duct of the right mandibular gland was found, after which it was entered with probe No. 0000, and then expanded to the size of probe No. 3 (photo 2). In order for the endoscope to penetrate the lumen of the duct, it was expanded using a dilator. The sialoendoscopy procedure was performed under copious irrigation with saline solution. The stone was removed using a three-wire ring (loop) (photo 3). The size of the opening of the duct was smaller than the size of the stone, so the doctor had to make a 0.1 cm incision at the entrance to the gland duct. After removing the stone, we examined the gland with an endoscope to make sure there was patency (photo 4). The glandular system was washed with a steroid solution. No bleeding, swelling or pain was noted in the postoperative period. The patient underwent daily dressings of the intervention area and monitoring for the development of possible wound infection.
Photo 2. a. Gland duct probe. b. Orifice dilator. c. Endoscope monitor. d. Three-portable endoscope. e. Three-wire ring (loop).
Photo 3. a. Stones in the gland duct. b. Removing stones using a loop. c. Capture the stones with a loop and remove them from the duct.
Photo 4. Removal of stones through the mouth of the submandibular salivary gland. b. View of removed stones.
Clinical case 2
Patient Information
A 66-year-old man sought dental attention due to a blocked duct of the right mandibular gland (Figure 5). Approximately 7-8 years ago, he noticed swelling and pain in the lower neck while eating. The sialolithotomy procedure was performed 4-5 years ago in another hospital, but the stones were never completely removed due to their pathological mobility during the operation. The patient had no systemic health problems.
Figure 5. Salivary stones measuring 3 × 4 mm were identified in the right submandibular gland using CBCT.
Surgical procedure
The working area was treated with betadine. After disinfection, the oral cavity was washed generously with saline solution. The patient was given full anesthesia via nasotracheal intubation, and the tongue was sutured with 3-0 silk suture. The intervention protocol was similar to the one we have already described in the first clinical case (photo 6). No bleeding, swelling or pain was noted in the postoperative period. The patient underwent daily dressings of the intervention area and monitoring for the development of possible wound infection.
Photo 6. View of the removed stone.
Discussion
Symptoms of obstructive salivary gland pathologies include recurring, painful swelling of the major salivary glands, which can negatively affect the patient's quality of life. Previously, radiosialography, sonography and MR sialography methods were used to diagnose diseases of the salivary glands. Radiosialography is the main method for examining the salivary glands, which can be used to diagnose sialolithiasis by analyzing images obtained after the injection of contrast into the gland duct. Contraindications to the use of this method are similar patient reactions to the contrast agent and the presence of an acute infectious lesion. Sonography is a non-invasive method for diagnosing stones in the structure of the salivary glands, however, the effectiveness of this approach largely depends on the experience of the doctor conducting the diagnosis. MR sialography allows for complete visualization of the entire salivary gland system, however, the resulting diagnostic images may be characterized by the presence of various types of distortions and artifacts, especially in cases of adjacent localization of dental restorations. However, all of the above-mentioned limitations characteristic of different diagnostic methods can be overcome using the sialoendoscopy method. It is less invasive than other approaches to diagnosing salivary gland pathologies and can be successfully used to assess the condition of their ducts and internal structure.
Several research groups have examined how satisfied patients were with the sialoendoscopy treatment process. Kroll et al, using the short version of the SF-36 questionnaire, found that patients reported a high level of satisfaction after sialoendoscopy. Aubin-Pouliot et al, using a questionnaire designed to assess chronic obstructive sialadenitis, demonstrated similar results. In addition, an interesting fact was established that after sialoendoscopy on the submandibular gland, the symptoms decreased much more pronounced than after a similar manipulation on the parotid salivary gland.
Recent studies have shown that microsialoliths play an important role in the pathogenesis of chronic sialadenitis. They can accumulate in normal salivary glands and provoke the development of obstructive atrophy. The latter, in turn, promotes the colonization and proliferation of microbes, causing inflammation in the peripheral ductal system, accompanied by even more severe atrophy and progressive infection, leading to chronic sialadenitis. According to Quinn et al, intraductal placement of antibiotics facilitates their penetration into the parenchyma of the glands, allowing the existing symptoms of the lesion to be completely eliminated. However, the same results were obtained when irrigating the internal structure of the glands with saline solution.
Radioactive iodine (RAI) therapy is another cause of salivary gland disease. According to Kim, chronic sialadenitis is the most common complication of RAI, especially in cases after thyroidectomy. The prevalence of chronic sialadenitis associated with RAI is 11–65%. Damage to the salivary glands caused by radioactive iodine leads to the development of obstructive sialadenitis and recurrent swelling with or without pain during meals. This chronic condition subsequently causes hyposalivation and associated symptoms, such as difficulty swallowing, taste disturbances, oral candidiasis and caries. Currently, chronic sialadenitis caused by radioactive iodine therapy is treated conservatively by maintaining a good level of oral hygiene, frequent hydration, the use of saliva substitutes, and stimulation of the salivary glands.
According to Kim's study, sialoendoscopy demonstrates similar effects to sialocentesis (intraductal irrigation with sterilized saline) and can improve obstruction symptoms as early as 3 months after mechanical dilatation with an endoscope. However, in patients with chronic sialoadenitis caused by radioactive iodine therapy, sialoendoscopy has been found to have limited ability to relieve existing symptoms of xerostomia.
This article described examples of using the sialoendoscopy method to remove stones from the salivary glands. This method is more effective compared to other approaches to the treatment of sialolithiasis, and at the same time less uncomfortable. In the two clinical cases analyzed, patients did not demonstrate any significant complications or similar effects after performing the manipulation.
Conclusion
This article describes two clinical comparisons of non-invasive sialolithotomy procedures using sialoendoscopy. This approach can be effectively used not only to treat cases of sialolithiasis, but also for ductal stenosis and sialadenitis. At the same time, sialoendoscopy is a minimally uncomfortable procedure, which is characterized by a low level of complications. To formulate any definite recommendations regarding the use of sialoendoscopy in cases of stones in the salivary glands, it is necessary to ensure that studies are carried out with the participation of a larger number of subjects.
Authors: Dong-Keon Lee, Euy-Hyun Kim, Chang-Woo Kim, Mong-Hun Kang, In-Seok Song, Sang-Ho Jun
Features of the procedure
If the flow channels are narrowed, appropriate therapy is prescribed using a probe to bougienage the salivary gland
. The procedure itself is as follows. First, an instrument is selected, a probe of the appropriate diameter, then it is inserted into the flow channel and left there for 12–16 minutes. In this case, the diameter of the probe increases each time. Thanks to this, it is possible to expand the duct as painlessly as possible. Before the procedure, the patient is advised to refrain from eating for 2.5 hours.
In order to consolidate the result, it is recommended to adhere to a special salivary diet; in addition, electrophoresis with potassium iodide and the required physiotherapeutic manipulations may be prescribed. The recovery period takes from several weeks to several months.
The specialists of the AlfaDent clinic will help solve any dental problem. Doctors use high-quality pharmaceuticals and advanced techniques. Timely detection of pathology and its treatment will help maintain the elements of the dental system and salivary glands in a healthy condition. We will help you get rid of any disease painlessly and with minimal time.
Pleomorphic adenoma (mixed tumor). This benign tumor is the most common, occurring in 72% of all epithelial tumors of the salivary glands. In terms of frequency of lesions, the parotid salivary gland is in first place, the mucosalivary glands of the palate are in second place, then, respectively, the submandibular, sublingual and minor salivary glands, glands of the lip, cheek, and tongue.Pleomorphic adenoma grows painlessly, slowly, over several years and can reach large sizes. When the adenoma is localized in the parotid salivary gland, paresis of the facial muscles is not observed. Upon examination, a tumor is detected in the area of the salivary gland, mobile, often with a bumpy surface. Its consistency is densely elastic, sometimes with areas of softening due to the mucus-like component. The skin above it does not change, it folds freely. The salivary function of the affected gland is usually not affected. Pleomorphic adenoma has a capsule, but may not be completely encapsulated, in which case the tumor cells penetrate into the adjacent glandular tissue. This explains tumor recurrences after extracapsular removal. Sometimes tumor growth accelerates significantly (within 1 month), and pain may appear. Such symptoms are characteristic of tumor malignancy; in such cases it is interpreted as carcinoma in pleomorphic adenoma.
The diagnosis of a tumor is clarified by cytological examination of the punctate, which is obtained in the needle in the form of a crumbly whitish mass.
Macroscopically, pleomorphic adenoma is a tumor in a thin translucent capsule, on a section in the form of a pasty mass of white-gray color with areas of mucus and compaction.
Microscopically, the tumor, in addition to pronounced epithelial tissue, contains mesenchyme-like areas consisting of myxoid or cartilage-like structures, the presence of which is explained by the accumulation of mucoid or hyaline substance between the myoepithelial cells.
Treatment is surgical. If the tumor is localized in the submandibular and sublingual salivary glands, the tumor is removed along with the gland. Tumors located on the palate, cheek, lips, tongue are excised within unaffected tissues. The peculiarity of the operation on the parotid salivary gland is associated with the branching of the facial nerve in the thickness of the gland. The nature and extent of surgical intervention depend on the size and location of the tumor. In all cases, it is necessary to excise the tumor with adjacent glandular tissue. Some authors suggest extracapsular tumor removal. When the tumor is localized in the lower pole of the gland, resection of this section is used. If the tumor occupies the anterior section and lies in the gland above the branches of the facial nerve, subtotal resection of the gland is performed in the plane of the branches of the facial nerve. Parotidectomy with preservation of the branches of the facial nerve is performed when most of the gland is affected and the tumor recurs, as well as when there is a tumor of the pharyngeal part of the gland. Access to the gland is carried out by two well-known methods - Kovtunovich and Redon. In the first case, the operation begins with exposure of the peripheral part of the facial nerve (middle branch), in the second - the central trunk.
The operation is parotidectomy with preservation of the branches of the facial nerve. A skin incision is made in front of the auricle 2-3 mm, starting from the scalp of the temple, bordering the earlobe and continuing in the retromaxillary and submandibular areas. the skin-fat flap is prepared and retracted anteriorly. The parotid-masseteric fascia and the anterior edge of the gland are exposed. When approaching the peripheral branches of the facial nerve, the location of the middle branch is determined: it is located next to the duct of the parotid gland along the line connecting the tragus with the angle of the mouth. The middle branch is dissected to the point of division of the trunk, then the upper and lower branches are isolated from the gland, holding them with threads to reduce trauma. The surface layer of the gland is removed, bandaged and the salivary duct is crossed. By lifting the branches of the nerve, the deep and pharyngeal parts of the gland are dissected and removed along with the tumor, and the external carotid artery is ligated along the way.
In an operation using the Redon method, after removing the skin-fat flap, the posterior edge of the gland is released and the external carotid artery is ligated. Then the trunk of the facial nerve is found deep in the wound between the mastoid process and the posterior edge of the mandibular ramus. The location of the nerve branch is determined and all three main branches are prepared. The further course of the operation is identical to that described.
An operation that involves removing only the superficial layer of the gland along with the tumor located above the branches of the facial nerve is called subtotal resection of the glands in the plane of the nerve branches.
In case of resection of the lower pole of the parotid salivary gland, a skin incision is made bordering the angle and body of the jaw, moving downwards by 1.5-2 cm, so as not to damage the marginal branch of the facial nerve. This must also be remembered during excision of the gland due to its location in this area. Subcutaneous tissue is dissected, m. platysma and fascia. The lower part of the gland, where the tumor is located, is exposed and removed. The wound is sutured in layers.
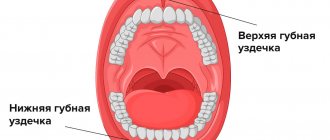
A mucous retention cyst most often forms in the minor mucosalivary gland of the lower lip, less commonly in the cheek, the anterior floor of the mouth, the lower surface of the apex of the tongue and palate. The predominant localization on the lower lip is associated with biting it.
The cyst is located under the mucous membrane, has the appearance of a hemispherical elevation with clear boundaries, ranging in size from 0.5 to 2 cm, with a bluish tint. Sometimes the mucous membrane over it is whitish in color, which is due to the presence of scar changes due to injury. Palpation of the cyst is of elastic consistency with ripple, painless. Biting the mucous membrane over the cyst can lead to its emptying, releasing a clear, viscous fluid. When the contents become infected, inflammation occurs.
Pathohistologically, the cyst wall is a connective tissue with granulations, turning into fibrous tissue, sometimes the inner side of the wall is partially lined with stratified squamous epithelium.
A mucous retention cyst must be differentiated from tumors of the minor salivary glands, which are less common, have an elastic consistency, sometimes with a bumpy surface, without fluctuation. In some cases, it is necessary to differentiate it from cavernous hemangioma, which is characterized by a purplish-bluish coloration and a symptom of filling.
Treatment consists of removing the cyst. Two converging semi-oval incisions are made in the mucous membrane above the cyst. Using a hemostatic mosquito clamp, the membrane is separated semi-bluntly from the surrounding tissues, the connective tissue bridges are cut with scissors and the cyst is isolated. Injured small glands protruding from under the edges of the wound and interfering with suturing are removed with tweezers or a “mosquito”, each separately and entirely. Using a scalpel for these purposes can lead to their dissection, incomplete removal and recurrence of the cyst. The operation is completed by applying catgut sutures to the mucous membrane.
Cyst of the sublingual salivary gland (ranula). This cyst is located, as a rule, in the anterolateral part of the floor of the mouth near the frenulum of the tongue. Clinically defined as an oval bulge, covered with unchanged mucous membrane or translucent with a bluish tint. The cyst is always intimately associated with one of the areas or the entire sublingual salivary gland. Its former name ranula (“frog tumor”) is determined by the type of cyst and its resemblance to the laryngeal bladder of a frog. It grows slowly, over months, and does not cause pain. When it reaches a significant size, speech is impaired and eating becomes difficult. Sometimes the cyst can extend beyond the midline of the floor of the mouth, displacing the tongue posteriorly or into the submandibular region. In the latter case, it is difficult to differentiate from a cyst of the submandibular salivary gland. On palpation, the cyst often appears as a formation with fluctuation, sometimes it is more elastic. When the membrane breaks through, a viscous transparent fluid is released abundantly from the cyst, and it is not contoured. After time, the cyst fills with fluid again and becomes visible.
Microscopically, the cystic fluid contains protein substances (clumps) and sometimes so-called cystic cells, apparently of epithelial origin.
Macroscopically, the cyst shell is thin, bluish-white. In terms of its microstructure, it is fibrous and granulation tissue associated with the interlobar connective tissue layers of the gland. The inner lining of the membrane rarely has cubic or columnar epithelium.
Diagnosis of a sublingual salivary gland cyst is usually not difficult. It should be differentiated from a cyst of the submandibular salivary gland, a dermoid cyst and vascular tumors (lymphangiomas and hemangiomas) localized at the bottom of the oral cavity.
Treatment: given the close connection of the cyst with the parenchyma of the gland, they are completely removed. The previously recommended cystotomy has limited use due to the frequent development of relapses. A cyst of the sublingual salivary gland, which spreads in the lower part of the floor of the oral cavity in the form of an hourglass, is operated on in two approaches: through an incision in the submandibular triangle, the lower part is bandaged and removed; from the side of the oral cavity, the sublingual gland with the remaining part of the cyst is excised.
A cyst of the submandibular salivary gland is much less common than a ranula. It is located in the submandibular triangle and is a painless formation of soft consistency. It grows slowly and is detected by chance when a swelling is detected in the submandibular region. A large cyst pierces the mylohyoid muscle (m. mylohyoideus) or bends around it from behind and spreads to the upper part of the floor of the mouth. In these cases, its bulging into the sublingual area is also determined. The salivary function of the gland is not affected.
Diagnosis of a cyst of the submandibular salivary gland is sometimes difficult. To clarify the diagnosis, a puncture is used: obtaining a yellowish mucous fluid suggests the presence of a cyst.
A cyst of the submandibular salivary gland is differentiated from lymphangioma, lipoma, lateral neck cyst, dermoid cyst.
To determine the topography of the cyst, a double contrast method is used: cystography and sialography. Different X-ray projections allow you to determine the relationship between the cyst and the gland
Treatment. The cyst of the submandibular salivary gland is removed along with the gland.
Parotid salivary gland cyst. This is a rare disease, localized in the superficial and deep layers of the gland, mainly in the lower pole. The cyst grows slowly. It is often discovered by accident.
The cyst is a limited, painless swelling in the parotid region of soft elastic consistency. The skin over the cyst is of normal color and gathers loosely into a fold. Unchanged saliva is released from the gland duct. The contents of the cyst are yellowish liquid, sometimes cloudy, mixed with mucus. Histologically, the walls of parotid salivary gland cysts do not differ from the walls of cysts of other salivary glands.
A parotid salivary gland cyst is differentiated from organ-specific tumors, lipomas, vascular tumors of the gland, as well as from a branchial cyst caused by pathology of the first branchial cleft.
Treatment consists of removing the cyst. Due to the close connection of the cyst shell with the parenchyma of the parotid gland, the adjacent section of the latter is excised. The complexity of the operation is related to the location of the branches of the facial nerve. Surgical access to the gland is the same as when removing benign tumors of the parotid salivary gland.
"Surgical Dentistry" edited by Robustova T.G.
Fourth edition. Moscow "Medicine" 2010
Clinical cases:
Pleomorphic adenoma of the left parotid salivary gland.