Salivary stone disease accounts for 40–60% of all diseases of the salivary glands. Often, patients find out about the presence of a stone in the salivary duct only in the doctor’s office, where they go with complaints of severe pain when swallowing, radiating to the ear or temple, with swelling in the face and neck. A stone located in the duct of the salivary gland interferes with the normal outflow of saliva and can completely block it. For more information about what a salivary stone is, why it occurs and how to treat it, read on.
What are stones in the salivary glands?
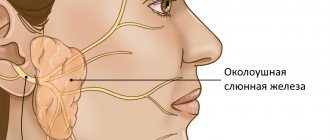
Salivary gland stones are pathological biomineral formations that block the ducts of the salivary glands. They can be single or multiple. Such formations are most often found in the submandibular gland and its excretory ducts, less often in the sublingual and parotid glands.
They are formed as a result of the deposition of organic and inorganic components:
- calcium salts;
- epithelial particles;
- sodium;
- mucin;
- magnesium;
- amino acids;
- potassium;
- iron;
- chlorine, etc.
The weight of salivary stone varies from 3–7 to 20–30 g [1, 2]. Round-shaped stones usually form in the parenchyma of the salivary glands, and oblong stones in the excretory ducts. Salivary stones often have a yellowish color, an uneven surface, and varying density.
Teeth stones are of the following types:
Stones on teeth (synonym - hard dental deposits) are usually divided into supragingival and subgingival.
- Supragingival calculus on the teeth (Fig. 1-6) – visible to the naked eye when examining the teeth, because always localized above the gum level. It may be dark or yellowish in color. A stone of such localization is not difficult to remove, which is usually carried out using ultrasound (however, very small dental plaque can also be removed using the Air-flow procedure).
- Subgingival stones on teeth (Fig. 7) are localized below the gum level, and therefore they are not visible during a normal visual examination of the teeth. However, in places where subgingival dental deposits are present, the gums usually have a bluish appearance, they are swollen and bleed easily. Also, sometimes when you press on the gum in these areas, a scanty purulent discharge may be released from under it. In the photo below you can see subgingival tartar, localized in a deep periodontal pocket.
Please note that the appearance of pink gums in the photo is completely normal. But after the gums peel off, we see a small amount of tartar and a large amount of destroyed bone around it. This picture is quite common for patients with periodontitis. Finding such stones is quite difficult. Firstly, a panoramic photograph of the teeth can help the dentist with this, because it will show the level of bone tissue around the teeth (the presence of such “bone pockets”).
If there are such pockets in the image, we immediately assume the presence of subgingival tartar in this area. The second method of detecting subgingival dental plaque is associated with the use of dental instruments. For this purpose, an air “gun” is usually used, which every dental unit has. The air flow from it moves the gum away from the root of the tooth, due to which the contents of the periodontal pockets become visible to a certain depth.
Etiology of sialolithiasis
Factors contributing to the development of pathology:
- Mechanical effects on the salivary glands (injuries to teeth and crowns). Inflammation compresses the ducts, where pathological microflora accumulates and pus appears. Over time, the stones increase significantly.
- Abnormal structure of the salivary glands and ducts.
- Disruption of calcium metabolism and, as a result, its deposition in the excretory ducts of the salivary glands.
- Hypovitaminosis, vitamin deficiency.
- Accelerated blood clotting.
- Entry of a foreign object into the gland duct. Bacteria actively multiply around the body, forming stone [2, 3].
The exact reasons for the formation of stones in the salivary gland have not yet been established. Presumably, risk factors are calcium metabolism disorders and vitamin A deficiency. Salivary stone disease most often affects men. Sialolithiasis mainly occurs in people 25–40 years old, and much less often in children.
The formation of salivary stones may be associated with a violation of the outflow of saliva or metabolism, with inflammatory processes in the salivary glands with the participation of microorganisms, poor nutrition, etc. As a rule, they are localized in the submandibular gland and its excretory duct; they are found in the sublingual and parotid glands very rare.
Abdusalamov M. R., Doctor of Medical Sciences, Professor of the Department of Traumatology of the Maxillofacial Region of the Moscow State Medical and Dental University named after A. I. Evdokimov [4]
Causes
The reasons for the occurrence of tartar, which cannot be removed at home, are:
1. Insufficient and poor-quality oral hygiene does not ensure sufficient removal of microbes that begin to actively multiply and “freeze”;
Note! This also includes incorrectly selected toothpaste, brush, brushing teeth “in haste,” and the absence of dental floss, brushes, rinsers, or irrigators in rituals.
2. Hard plaque occurs due to excessive consumption of soft foods and fast carbohydrates (flour and confectionery products). They promote abundant salivation, which provides favorable microflora for the proliferation of bacteria;
3. Bad habits - smoking, drinking alcoholic beverages (especially coloring ones, such as red wine), unhealthy diet;
4. Metabolic disorder, which leads to a change in the composition of saliva and an increase in free salt ions.
A combination of one or more reasons influences the success of tartar removal.
Plaque appears on all teeth, but the most common are the lower teeth on the inside. This is due to its proximity to the large salivary glands.
Symptoms of the disease
If a person is not attentive to the hygiene of his teeth, he is unlikely to examine the oral cavity with a flashlight to assess the degree of neglect of the situation.
Therefore, you can determine the presence of a problem not only visually, but also by indirect signs:
- bleeding gums - often completely painless and occurs only when brushing your teeth (naturally, after the impact of a toothbrush on sensitive gums, unpleasant sensations arise);
- bad breath - if there are no problems with the stomach, but the smell is present, it is worth considering that perhaps an impressive amount of stone has accumulated, since the active activity of microorganisms is associated with the release of sulfur compounds;
- swelling and soreness of the gums - a feature of the accumulation of plaque, which will be discussed below, affects the soft tissues, developing inflammatory processes.
Important! It is very important to remove tartar before gum recession begins - a decrease in soft tissue, “lowering” or “raising” of the gums. This leads to exposure of the tooth root and increased sensitivity.
Types of Tartar
Based on their location, there are two types of plaque:
- Supragingival - visible stone, located above the gum, often found on the lower front teeth on the inside and in the area of the upper molars;
- Subgingival - as the name suggests, plaque, which is located in the periodontal pocket, in the groove between the tooth and the gum, cannot be seen with the naked eye;
- Stone bridge - microbes can cover the enamel of several teeth in a row, the most advanced case.
Cleaning tartar will also depend on the method of its attachment to the surface:
- with the inclusion in the process of organic pellicles on “cement” (this is a specific tissue covering the root part of the tooth);
- with the inclusion of organic pellicles on the enamel in the process;
- synthesis on uneven abrasive surfaces, for example, in the early stages of caries disease, or at chipped sites (and also, as mentioned earlier, during the formation of food plaque);
- attachment in the depressions and ridges between teeth on the enamel or tooth root.
Consequences of dental plaque
Dentists know how to remove tartar to avoid damaging your smile.
What complications threaten?
- inflammation of the gums and gingivitis - tartar, especially the subgingival type, has a direct effect on the tissue, promoting softening and redness, then the pocket between the gum and tooth begins to increase, increasing the formation of new bacteria;
- periodontitis - in which bone tissue is also involved, which gradually begins to break down, which ultimately leads to complete loss of teeth.
Therefore, it is important to pay attention to the formation of tartar in a timely manner and contact a dental clinic to remove it.
Tartar removal
There are several ways to get rid of future diseases.
Ultrasound
Ultrasonic tartar removal is the most common and safe method used in dentistry today.
The principle of operation is small, rapid vibration of the tip of the device - the scaler. When it comes into contact with a tooth, it creates enough resonance to destroy hard plaque.
Additionally, the nozzle treats the tooth surface with a chlorhexidine solution or water, thus polishing the surface to prevent the attachment of new plaque.
The advantage is minimal impact on the native enamel.
Air Flow
In fact, the method is based on the destruction of plaque by a thin jet directed under high pressure, consisting of water and air, non-abrasive particles.
If necessary, additional antiseptic substances are used.
Laser
It is rarely used due to the high cost of the equipment, and the principle of operation is the same as that of ultrasound - a directed beam destroys the stone, and air or water “washes” it out of the dental spaces.
Mechanical cleaning
Sometimes a mechanical, that is, manual cleaning method is used using:
- hand scalers - metal sticks with straight and curved attachments;
- excavators - sticks with attachments, similar to spatulas;
- chisels - so called precisely because of their external resemblance to their larger brother;
- curette - thin metal hooks;
- rasps - the ribbed attachment is designed for scraping.
This type of cleaning is quite unpleasant and painful, but it is the most effective, especially with complex deposits.
However, if the doctor is careless, he can irreversibly damage the tooth enamel, so it is important to choose a dental clinic with professionals in the field of hygienic cleaning.
Which method to choose
The cleaning procedure most often includes several stages, which vary depending on the quantity and quality of plaque. But the standard set of actions looks like this:
- Ultrasound;
- Air-flow;
- Polishing with a brush;
- Remineralizing therapy.
Finally, the doctor will polish the surface of the tooth and coat it with fluoride to prolong the effect of the manipulation.
How tartar is removed in a particular case depends on the diagnosis. It is important that the dentist use a microscope to detect the early stages of plaque.
As a rule, even after improving nutrition and oral hygiene, it is necessary to come for a preventive examination, which includes professional cleaning every six months. This will avoid problems with gums, and will also allow timely detection of caries and other disorders.
Symptoms of a stone in the salivary gland
The onset of the disease occurs unnoticed (from several months to several years). Upon examination, the patient does not show any abnormalities. The first symptoms of the disease appear when the flow of saliva is disrupted during food intake, especially sour or spicy food.
Patients note the periodic appearance of swelling in the area of the salivary gland. Increased pain during eating is associated with difficulty in the outflow of saliva due to the presence of a stone in the duct. After eating, pain and swelling in the gland area gradually decrease.
The following symptoms are observed:
- increased body temperature;
- dry mouth, secretion of a small amount of saliva;
- a feeling of fullness in the part of the oral cavity where the stone has formed;
- difficulty opening the mouth;
- frequent pain when eating;
- swelling and redness on the face;
- discomfort when chewing and swallowing.
Over time, changes in the gland increase: the disease passes into a clinically pronounced and late stage, when clinical signs of chronic sialadenitis are visible. The submandibular salivary gland enlarges, becomes dense and painful.
What it is
Tartar is a hardened plaque that forms in adults and very rarely in children, and even then in the presence of a history of serious diseases such as heart disease or diabetes. Usually, if you spend enough time on hygienic procedures to remove plaque, stones will not form on your teeth. If plaque is not allowed to harden, stones cannot form. Therefore, thorough brushing of teeth is the best means of prevention.
Tartar can occur on one single tooth or on several teeth. The lower front teeth, as well as the upper and lower molars, are most susceptible to tartar formation.
Signs:
- Tartar causes bad breath;
- gums begin to itch and bleed;
- Dark stains appear on the visible surfaces of the teeth that cannot be removed with a brush.
Tartar can form not only on enamel, but also on crowns or dentures. Therefore, those who do not have their own teeth in their mouth, but only dentures, should not relax - stone can form on them, just like on the surface of the enamel. It, of course, will not lead to caries on the crown, but it can provoke inflammation of the gums, and also significantly spoil the appearance of the dentures.
Plaque from tea and cigarettes can provoke the formation of tartar. The constant presence of such plaque on hard-to-reach enamel surfaces inevitably leads over time to the formation of dense deposits, including stones.
Diagnostics
If you suspect sialolithiasis, you should consult a dentist.
The following methods are used for diagnosis:
- X-ray examination is currently the main diagnostic method. To identify a stone in the duct, an X-ray of the facial skeleton is taken in a direct projection. If the stone is localized in the anterior part of the duct, an x-ray of the floor of the mouth is shown; if it is located in the posterior part of the duct or in the submandibular gland, an x-ray of the lower jaw in a lateral projection is shown.
- Ultrasound - a study is carried out if there is a discrepancy between clinical manifestations and radiographic data to clarify the diagnosis.
The indicated diagnostic techniques are usually sufficient to establish a diagnosis and determine the location of the stone. There are other methods for studying the salivary glands, which are used less often in practice - CT and MRI. Their diagnostic value for calculus detection is close to 100%, since it allows one to determine the spatial location of the salivary stone.
Treatment
Treatment for stones consists of removing them; there are simply no other methods of treatment. Sometimes it happens that tartar is removed from the surface of the teeth by itself under the influence of solid food, but you should not hope for this. It is better to consult a specialist in a timely manner, a hygienist who will quickly and painlessly remove dental deposits from the surface of the enamel.
If earlier tartar removal was carried out mechanically, that is, it was simply scraped off the surface of the enamel, today there are more modern and painless methods for removing deposits. Among them, the most common is the ultrasonic method of teeth cleaning.
Using the ultrasonic method, the dentist will quickly and effectively remove all dental plaque without injuring either the gums or the enamel surface. The procedure for removing tartar is completed by polishing and grinding the enamel, during which the teeth become shiny and their surface is smooth.
Treatment of stones in the salivary gland
In order to remove stone from the salivary gland duct, use:
- conservative therapy;
- surgical treatment.
First of all, the following are assigned:
- antibiotics;
- drugs that stimulate saliva production;
- anti-inflammatory drugs.
Re-inflammation often occurs and the process can become chronic. In such cases, the only treatment method that eliminates the root cause of inflammation is surgery.
Removal of a stone in the salivary gland from the duct is carried out under general anesthesia. The stone itself and the capsule surrounding it are excised. This surgical intervention is called sublingual extirpation and lasts 40–60 minutes. The main risk when performing surgery on the salivary glands is due to the fact that the facial, lingual and hypoglossal nerves pass in close proximity to them.
There is a less invasive method - sialoendoscopy. It allows one to penetrate the ducts of the salivary glands through the thinnest endoscopes without dissecting tissue and visualize the salivary system at high magnification. The endoscope is inserted into the opening of the gland duct in the mouth. Next, using micro-instruments, the surgeon examines the ducts, removes the stone, injects medicinal substances into the gland and performs other necessary manipulations.
Stone removal methods
1. Conservative. Can only be used at the initial stage of disease development. The specialist prescribes medications that provoke a good flow of saliva, which can stimulate the dissolution of the stone.
2. Surgical method. Removal of salivary gland stones is carried out through surgery. The doctor makes an incision at the site of the tumor and removes the object.
3. Removal of salivary glands. Such operations are used extremely rarely in practice; they take place only if, for a number of reasons, surgical treatment is ineffective.
Prevention of salivary stone formation
It is worth taking note of a few rules to prevent the occurrence of salivary stones:
- Avoid disruption of mineral and vitamin metabolism.
- Give up bad habits, which will have a beneficial effect on other body systems.
- Protect yourself from maxillofacial injuries.
- Carefully follow the rules of oral hygiene: brush your teeth 2 times a day, follow the dentist’s individual recommendations. Perhaps you need a toothpaste with a certain composition, mouth rinses, or dental floss.
- Choose the right toothbrush (medium-hard bristles with artificial bristles).
- Visit the dentist regularly to monitor the condition of the oral cavity, timely detection of lesions and effective treatment.
Sialolithiasis is a fairly common pathology, for the treatment of which conservative and surgical methods are used. With timely detection of the disease and subsequent proper treatment, the prognosis is favorable. This will also prevent complications and speed up the healing process.
List of sources:
- Gamataev I. I. Study of human salivary stones. New challenges of modern medicine, 2013 // URL: https://moluch.ru/conf/med/archive/86/3883/ (access date: 11/04/2020).
- Dmitrienko E. V., Shashkevich V. A. Algorithm for the diagnosis and treatment of salivary stone disease. Journal "Bulletin of the Smolensk State Medical Academy", 2010 // URL: https://cyberleninka.ru/article/n/algoritm-diagnostiki-i-lecheniya-slyunnokamennoy-bolezni (access date: 11/04/2020).
- Kartashov R. Sialolithiasis: the stumbling block is in the salivary gland. European Medical Center // URL: https://www.emcmos.ru/disease/sialolitiaz-kamen-pretknoveniya-v-slyunnoy-zheleze/ (access date: 12/13/2020).
- Gamataev I. I. Study of human salivary stones. Intl. scientific Conf., 2013 // URL: https://moluch.ru/conf/med/archive/86/3883/ (date of access: December 26, 2020).
Medicines to replace saliva
Saliva substitutes commonly available in spray form can be divided into two groups:
- based on mucin - a gel-like protein that provides the drug with the necessary viscosity and surface tension to imitate real saliva;
- based on lactoperoxidase, an enzyme of the salivary glands with antibacterial properties [1].
The solution, like natural saliva, contains mineral salts. Its pH value is also close to natural.
Release form: compact bottles (50–100 ml), which are convenient to carry with you. The spray is used to irrigate the mucous membranes of the oral cavity as needed.
Recovery after sialoendoscopy
After the procedure, patients should drink a large volume of water to stimulate salivation and thus flush the cleansed salivary ducts. Typically, the function of the salivary glands is fully restored after a certain recovery period, thus allowing the gland to be preserved.
When the procedure is performed under local anesthesia, patients can go home within a few hours. When using anesthesia, it is recommended to stay in the clinic overnight. No special rehabilitation is required in this case. Patients should not overexert themselves or exercise for several days. The recovery is going well and if medical recommendations are followed, complications of the operation are excluded.
Tartar and oral hygiene –
After eating, a large amount of food debris remains in the mouth (primarily in the interdental spaces), and they cannot be removed by rinsing or chewing gum alone. For their vital activity, bacteria primarily use easily digestible carbohydrates, which are found in sweet and flour products. It has been established that in the absence of proper hygiene for only 1 day, the amount of bacterial plaque in the oral cavity increases at least 2 times.
But bacteria use nutrients not only for reproduction, but also for the production of special enzymes (enzymes), which allow bacteria to firmly attach to the surface of the tooth (24stoma.ru). In the absence of proper hygiene, individual pinpoint bacterial colonies attached to the teeth merge, forming a significant mass of bacterial plaque (Fig. 8-9). At this stage, plaque is still soft and can be removed with a regular toothbrush.
Accumulations of soft microbial plaque –
Next, there will be a gradual mineralization of soft microbial plaque, which will eventually turn into hard tartar. Mineralization (calcification) of soft dental plaque occurs through the deposition of proteins and calcium salts contained in saliva on the surface of bacterial colonies. The mineralization process occurs in combination with the layering of new bacterial colonies.
In parallel, microbial plaque releases toxins and inflammatory mediators, which trigger inflammatory phenomena in the gums. The main signs of gum inflammation are –
- bleeding when brushing teeth,
- redness or bluishness of the gums,
- pain in the gums,
- in later stages - suppuration from periodontal pockets, tooth mobility.
Pathogenic bacteria are very cunning, and gum inflammation is vital for them. The fact is that in the place where the gums adhere to the tooth there is a so-called periodontal groove, into which periodontal fluid is constantly produced from the gums in small quantities. This liquid contains a large amount of salts and proteins necessary for bacteria to quickly grow colonies. The launch of inflammation processes in the gums leads to a sharp increase in the production of periodontal fluid, and as a result, microbial colonies receive even more proteins and salts necessary for the calcification of tartar.