What are lymph nodes?
Lymph nodes are structures of the immune system that act as a specific filter for microbial antigens. Lymph flowing through the nodes is filtered, and substances that could cause infection are captured and removed. The nodes are also involved in the production of antibodies. Their size depends on the age of the child. They should not be palpable in newborns and infants. Lymphadenopathy, or enlarged lymph nodes, mainly affects children of preschool and primary school age.
Contact with a large group of peers causes the child to develop immunity. It is not difficult to become infected in kindergarten, and a history of infection often manifests itself as enlarged and clearly palpable lymph nodes
. If they have enlarged as a result of illness, this should not be a cause for concern. An alarming symptom is lymphadenopathy that is not associated with a previous disease, as it can be a symptom of serious diseases, including malignant neoplasms. Pediatricians refer the child for diagnostics to an oncology clinic so as not to miss anything. Find out what causes swollen lymph nodes in your child and what diagnostic tests should be done.
Lymphadenitis in children
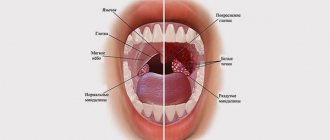
As a rule, lymphadenitis in children affects the lymph nodes in the face and neck (most often - submandibular and cervical on one or both sides, less often - parotid, buccal, occipital, behind-the-ear), in some cases - axillary, inguinal.
The serous stage of acute nonspecific lymphadenitis in children (days 1-3 of the disease) is manifested by painful, noticeably enlarged regional lymph nodes that are densely elastic to the touch, without loss of their mobility and the development of a local skin reaction. The child's general condition is not affected; the temperature ranges from normal to subfebrile values.
The transition of acute lymphadenitis to the purulent stage (days 3-6 of the disease) occurs with pronounced local signs and a sharp deterioration in the well-being of children. Signs of intoxication are observed: chills, high temperature (up to 40ºC), headache, severe weakness, lack of appetite and sleep disturbance. In the area of the affected lymph nodes, intense nagging or shooting pains, periadenitis, local hyperemia and swelling of the skin occur. The development of adenophlegmon with the appearance of foci of fluctuation and the release of purulent inflammation beyond the lymph node is possible. Adenophlegmons of the maxillofacial area can be complicated by thrombosis of the cavernous sinus, mediastinitis, and sepsis.
The chronic form of lymphadenitis in children can develop primarily if the causative agents are weakly virulent microorganisms, or become a continuation of the acute form of the disease. In a chronic course without exacerbation, the lymph nodes are enlarged, limited in mobility, quite dense, but painless; the child’s well-being is not impaired; suppuration develops rarely. If a child has a focus of chronic infection that maintains sluggish lymphadenitis for a long time, the lymph nodes are gradually destroyed and replaced by granulation tissue.
Tuberculous lymphadenitis in children has a long course and is usually limited to the cervical group of lymph nodes, collected in a dense, painless, large package, similar to a collar. Tuberculous lymphadenitis in children can be complicated by caseous decay, the formation of fistulous tracts, and cicatricial changes in the skin.
Specific lymphadenitis associated with vaccination against tuberculosis (“betsejeitis”) can develop in children with low and altered general reactivity, manifested by chronic calcific caseous lesions of the axillary lymph nodes. Generalized lymphadenitis in children is observed with disseminated pulmonary tuberculosis and chronic tuberculosis intoxication; accompanied by characteristic fibrosis of nodes (“pebble glands”).
Causes of enlarged lymph nodes in a child
If your doctor suspects that your lymphadenopathy is not the result of an infection, the first step is to perform a physical examination and take a detailed medical history. Hard, dense nodes that do not move under the fingers will be the basis for referring the child for laboratory tests, possibly also for imaging. Only if the test results are concerning, the doctor will order a histopathological examination.
Basically, there can be two reasons for enlarged lymph nodes in a child. The first is the proliferation of nodal cells, mainly lymphocytes. The second reason is infiltration caused by foreign cells - inflammatory and malignant. Neoplastic diseases that present with lymphadenopathy include lymphocytic lymphoma and Hodgkin lymphoma. However, cancer is not the main cause of enlarged lymph nodes. More often, lymphadenopathy is caused by: - viral infections;
- allergies; — vaccination; - autoimmune diseases.
Causes of enlarged lymph nodes in children
Lymph nodes belong to the organs of the immune system.
Role of lymph nodes:
Barrier. Lymph nodes (LN) are the “first line of defense” against the penetration of various foreign agents into the child’s body. A natural reaction to this “acquaintance” is an enlargement of the lymph nodes.
Filtration. Various substances, microbial cells, and particles of the body’s own tissues settle in the lymph nodes.
Parents often call enlarged lymph nodes “glands.”
The lymph node itself is a small oval formation (several millimeters in diameter). On the outside it is covered with a special capsule of connective tissue, and on the inside it is divided into separate sections by partitions. These elements of the immune system are located in groups throughout the body at the confluence of several lymphatic vessels. In newborn babies, the capsule of the lymph nodes is still very tender and thin, so it is difficult to feel them under the skin. By the age of one year, lymph nodes can already be felt in almost all healthy children.
The maximum number of lymph nodes appears by 10 years of age. In an adult, their total number is 420-460.
The size and condition of the lymph nodes are assessed by palpation. In this case, it is necessary to palpate the lymph nodes in all groups (there are 15 of them) - from the occipital to the popliteal. If the lymph nodes are significantly enlarged, parents or the child themselves can pay attention to this symptom. When a lymph node becomes inflamed (lymphadenitis) due to the appearance of pain, children clearly indicate the localization of the process.
Normally, in healthy children, no more than three groups of lymph nodes are usually palpable.
Should not be palpable:
- chin;
- supraclavicular;
- subclavian;
- chest;
- elbows;
- popliteal lymph nodes.
Signs of normal lymph nodes:
- their size does not exceed the diameter of a small pea,
- they are isolated
- soft elastic consistency.
- mobile,
- not connected to the skin and to each other (doctors say “not fused”),
- painless.
An increase in the size of lymph nodes with a change in their consistency is called lymphadenopathy, a quantitative increase in lymph nodes is called polyadenia (from aden- gland, since previously lymph nodes were mistakenly considered glands).
Causes of enlarged lymph nodes in children:
- infections;
- tumor processes;
- a special metabolic disorder called “storage diseases”.
Local (regional) isolated enlargement of lymph nodes is always caused by changes in the corresponding zone (region) of the body from which lymph comes.
In all cases of unusual local enlargement of lymph nodes, a thorough examination of the child is necessary to determine the extent to which the process has generalized (spread).
Stages of diagnosis for isolated enlarged lymph nodes:
Clinical diagnosis. It consists in the fact that the doctor first makes a diagnosis based on the complaints of the child or parents, clinical data and the results of blood, urine, x-ray, etc. tests.
Tuberculin diagnostics. Necessary to exclude the possibility of tuberculosis.
Special (serological) blood tests (performed if another infection is suspected).
Usually, with an isolated increase in any group of lymph nodes, antibacterial agents are prescribed for 8-10 days. An improvement in the child's condition and a decrease in swelling of the lymph nodes is regarded as confirmation of the bacterial nature of the disease.
Biopsy of a lymph node or puncture with examination of the lymph node tissue under a microscope. It is carried out in the most difficult diagnostic cases.
Features of damage to lymph nodes in certain areas:
Enlarged occipital lymph nodes: found in inflammatory processes of the scalp (purulent rash, boils, osteomyelitis of the calvarial bones, fungal infection). With rubella, in addition to the occipital ones, other groups of lymph nodes are enlarged to a lesser extent.
Enlarged parotid lymph nodes: characteristic of inflammation of the middle and outer ear, purulent inflammation of the scalp (pyoderma), lice, furunculosis. Often these groups of lymph nodes react to infection of an allergic rash in atopic dermatitis and eczema, especially when it is localized behind the ears.
Enlarged lymph nodes behind the angle of the lower jaw and along the posterior muscles of the neck. Develops during inflammatory processes in the nasopharynx or after them: tonsillitis, infectious mononucleosis (as a manifestation of a generalized process), with chronic tonsillitis and adenoid growths, with tuberculosis of the tonsils.
Enlarged lymph nodes behind the angle of the lower jaw and in the middle triangle of the neck: severe forms of tonsillitis, scarlet fever. With diphtheria of the tonsils, there is a symmetrical increase in lymph nodes to the size of an apple. At the same time, they are elastic and painful. Swelling of the surrounding tissues develops with an increase in the size of the neck. In the case of severe angina, acute inflammation of the lymph nodes can develop - lymphadenitis and even purulent lesions. In case of cat scratch disease (caused by a special microorganism), this group of lymph nodes may increase. The combination of sore throat, lymphadenitis and peeling of the palms and feet is characteristic of streptococcal infection (streptococcal tonsillitis, scarlet fever). Several more reasons for the reaction of this group of lymph nodes: Kawasaki syndrome (combined with damage to the eyes, skin, coronary arteries, fever, rash), toxoplasmosis, tumors of the blood and lymphatic system (Hodgkin's disease - lymphogranulomatosis, non-Hodgkin's lymphoma - lymphosarcoma).
Enlarged lymph nodes in the lateral triangle of the neck may be a sign of infection in the nasopharynx, tuberculosis of the lymph nodes, or tumors.
Enlargement of the lymph nodes in the mental area develops with an abscess in areas of the jaw, with damage to the front teeth - incisors, stomatitis, inflammation of the lower lip.
Enlarged submandibular lymph nodes are characteristic of inflammation of the jaw due to dental damage, stomatitis and gingivitis (inflammation of the gums). After treatment with antibiotics, the lymph nodes shrink and restore their mobility when palpated.
Enlargement of the axillary lymph nodes occurs with infectious diseases of various causes in the arm and shoulder area (purulent skin lesions, chicken pox). Unilateral lymph node enlargement can develop after vaccination or injury to the arm, such as cat scratch disease.
Enlarged ulnar lymph nodes are a sign of infection in the hand or forearm.
Enlarged inguinal lymph nodes indicate an infection in the lower extremities, localized in the bones, muscles or skin. This symptom appears with inflammation of the joints, with severe diaper dermatitis, with furunculosis in the gluteal region, inflammation of the genitals, after BCG vaccination when the vaccine is administered to the thigh area. Moreover, an isolated increase in lymph nodes for 3 months after BCG is normal, and a longer persistence of the symptom is regarded as an indirect sign of a decrease in the activity of the immune system or high virulence of the vaccination material, or as an individual feature of the child’s reactivity. A biopsy of such lymph nodes may reveal large numbers of blood cells called macrophages. After BCG, LNs can be soaked in lime and palpated through thin skin for many years. In case of infection penetration through the skin of the leg in cat scratch disease, the group of inguinal lymph nodes also reacts.
Frequent wounds to the skin of the legs and feet, infection of these wounds in children of preschool and school age lead to the fact that in most of them significantly enlarged lymph nodes are clearly palpable in the groin area. Such children are not considered sick in the absence of other signs of pathology.
Many diseases begin with an increase in lymph nodes in any one zone, and then the lymph nodes increase in almost all groups. This picture is observed with influenza, measles, rubella, infectious mononucleosis, viral pneumonia, viral hepatitis, widespread eczema, congenital syphilis, toxoplasmosis, etc.
In addition to the lymph nodes, other formations can also raise the skin and be palpated under the skin. One of the reasons for this is lymphangioma (parents are more familiar with a nearby formation of blood vessels - hemangioma), a soft swelling under the skin without clear boundaries. Lymphangioma is localized mainly in the neck and can cause difficulties during childbirth, swallowing and breathing. Often requires surgical treatment.
It must be remembered that LNs are located both in the chest and in the abdominal cavity.
Signs of enlarged lymph nodes in the chest:
- breathing problems;
- difficulty swallowing;
- prolonged hiccups.
The reaction of lymph nodes in the abdominal cavity to a viral or bacterial infection can manifest itself as very severe abdominal pain, which sometimes requires a differential diagnosis with appendicitis.
Parents should know that if one or more enlarged lymph nodes are detected in one group, they need to carefully examine the child and palpate lymph nodes in other areas. Before consulting a doctor and having a blood test, you should not heat the lymph nodes. Children who have enlarged glands in most groups must be examined using ultrasound of internal organs to assess the condition of the liver, spleen and abdominal lymph nodes.
May our children be healthy!
Doctor T.A. Konon
Enlarged lymph nodes in a child's neck
Enlarged lymph nodes in a child's neck are of greatest concern to parents and doctors because they may be a sign of Hodgkin's lymphoma. The disease most often occurs in adolescent children, less often in young children. In most cases, the cause of enlarged nodes in the neck is viral infections, incl. mononucleosis, that is, a disease caused by the EBV virus, and bacterial - inflammation of the tonsils and throat.
In the case of lymphadenopathy located in the neck, you can be sure that the pediatrician will prescribe basic diagnostic tests, incl. blood analysis.
However, it is worth considering that an increased level of lymphocytes in a child under 6 years of age is perceived as normal. Doctors call this physiological lymphocytosis. Additionally, you should be aware that the standards set by the laboratory apply to adults, so any test results should be discussed with your pediatrician. Comparing the data to the standards provided by the laboratory is not sufficient to correctly interpret a child's test results.
M.S. Savenkova, A.A. Afanasyeva, A.K. Abdulaev, L.Yu. Nizhko Department of Clinical Functional Diagnostics with a course in Pediatrics, State Educational Institution of Higher Professional Education, Russian State Medical University of Roszdrav, Morozov Children's City Clinical Hospital, Moscow
In recent decades, one cannot fail to note the significant progress that has occurred in the field of diagnosing various infectious diseases in children, thanks to which the clinical features of the course of infections such as chlamydia, mycoplasmosis, toxoplasmosis, bartonellosis, borreliosis, as well as herpesvirus infections (EBV, CMV) have become more clear. and others. One of the important symptoms of the above diseases is lymphadenopathy - enlarged lymph nodes of varying severity. Unfortunately, the symptom of enlarged lymph nodes is not always assessed in a timely manner by pediatricians and is not given due attention. The structure of lymph nodes Lymph nodes are peripheral lymphoid organs, consisting of cells of various types, connected to the circulatory system by afferent and efferent lymphatic vessels and postcapillary venules. Fibroblasts and their derivatives, reticular cells, form a supporting structure. Tissue macrophages, dendrites and Langerhans cells are important antigen-bearing cells. Lymphoid follicles consist mainly of B lymphocytes. Primary lymphatic follicles are populated by IgM and IgD-bearing B cells and helper T lymphocytes (inducers) even before the antigenic stimulus. Secondary lymphatic follicles are formed as a result of antigenic stimulation and contain an internal zone (germinal center) consisting of activated B cells, macrophages, follicular dendrites and helper cells. The areas between follicles and paracortical areas consist mainly of T lymphocytes. The co-location of a large number of macrophages, dendrites, Langerhans cells and lymphocytes allows the lymph node to perform the main function of a specialized structure that integrates all these cell types to create an effective cellular and humoral immune response of the body. Enlargement of the lymph node may be due to: 1) an increase in the number of benign lymphocytes and macrophages during the immune response to the antigen; 2) infiltration by inflammatory cells during infections affecting the lymph node (lymphadenitis); 3) proliferation in situ of malignant lymphocytes and macrophages; 4) infiltration of nodes with metastatic malignant cells; 5) infiltration by macrophages loaded with metabolic products in various storage diseases.
Pathogenesis of lymphadenopathy Back in 1980, the term lymphadenitis was commonly used to mean “inflammation of the lymph nodes that occurs as a complication of various purulent-inflammatory diseases and specific infections (tuberculosis, plague, actinomycosis). In previous years, pyogenic cocci were considered the main etiological causative agents of the development of lymphadenitis. Later, different types of microorganisms (bacteria, viruses, fungi) were described as pathogens. There is acute inflammation of the lymph nodes, which is characterized by a short prodromal period, fever, local pain on palpation, and chronic, which is usually characterized by a longer duration, absence of pain or its low severity. In chronic inflammation, unlike acute inflammation, the lymph nodes are usually separated from the surrounding tissues. Lymphadenitis can be local, regional, generalized. Regional lymphadenitis has been described in streptococcal and staphylococcal infections, tularemia, tuberculosis, syphilis, and genital herpes. Generalized enlargement of lymph nodes is described in infectious mononucleosis, cytomegalovirus infection, toxoplasmosis, brucellosis, tuberculosis, AIDS, storage diseases, etc. Enlargement of lymph nodes occurs as a result of the accumulation of microbes or viruses and their toxins in them by lymphogenous, hematogenous and contact routes. In acute lymphadenitis, serous edema is observed, and inflammatory phenomena do not extend beyond the capsule of the lymph node. During destructive processes, inflammation can spread to surrounding tissues and, by the nature of the inflammation, be serous and/or purulent.
Clinical picture and diagnosis The clinical symptoms of lymphadenitis are the same and are characterized by pain on palpation, an increase in size, and an increase in body temperature. Hyperemia of the skin over the lymph node appears later, as the process progresses and the serous transition to the destructive stage. For the convenience of assessing the inflammatory reaction of the lymph nodes, we have identified three degrees of their enlargement: (Sav 2003):
I degree – from 0.5 to 1.5 cm in diameter; II degree – from 1.5 to 2.5 cm in diameter; III degree – from 2.5 to 3.5 cm in diameter and more.
Lymphadenopathy is characterized, as a rule, by an enlargement of a number of groups of lymph nodes without signs of hyperemia of the skin over them. However, palpation often reveals not one enlarged lymph node, but several, or a conglomerate consisting of lymph nodes of different consistency and size. In this regard, the group of lymph nodes (cervical, axillary, inguinal, etc.) should be indicated. To clarify the nature of the damage to the lymph nodes, determine their quantitative and qualitative characteristics, it is advisable to conduct an ultrasound examination. Ultrasound examination of lymph nodes makes it possible to clarify their size and determine the duration of the pathological process and its severity. In acute inflammation, the hypoechogenicity and homogeneity of the lymph nodes is determined. Adhesive lymph nodes suggest a disease duration of more than 2 months. With the chronic course of the process, their echogenicity increases. In practice, pediatricians have repeatedly encountered underestimation of the symptom of enlarged lymph nodes. Unfortunately, children do not always arrive (apply) for examination in a timely manner; as a result, a chronic course of the infectious process is formed, and often transformation into hematoblastosis. Considering the increase in the number of lymphadenopathy in recent years, we examined children admitted to the hospital or outpatients with the main complaint of enlarged lymph nodes for the period from 2004 to 2008. to determine the predominant pathology and select adequate antibacterial therapy. The examination plan for children with lymphadenopathy (Fig. 1) must be comprehensive. You should start by assessing changes in the peripheral blood test: leukocytosis and a shift of the formula to the left indicate the course of a bacterial process (staphylococcal, streptococcal, Pseudomonas aeruginosa, hemophilic etiology). The predominance of lymphomonocytes in the blood count is usually characteristic of diseases of herpetic and intracellular etiology. To clarify the etiology of the disease, a complex of serological and microbiological examinations is required, which includes the most common diseases in children. The main diseases that occur with enlarged lymph nodes include: chlamydia, mycoplasmosis, toxoplasmosis, Epstein-Barr virus (EBV) infection, cytomegaly, as well as herpes types I, II, VI. If negative results are obtained, the examination is further carried out to exclude less common diseases: listeriosis, bartonellosis, borreliosis, parasitic diseases (toxocariasis, echinococcosis, opisthorchiasis, giardiasis, etc.). Microbiological examination should be carried out in children with a history of frequent respiratory diseases, sore throats, inflammatory diseases of the oropharynx, croup, and bronchitis. As a rule, with a localized process in the oropharynx, the regional group of cervical lymph nodes increases in the clinic. Polyadenopathy is characteristic of a generalized infection. One of the objective auxiliary methods for additional assessment of enlarged lymph nodes is ultrasound. If a generalized reaction develops, it is recommended to test the blood for sterility and conduct an ultrasound examination of the intra-abdominal lymph nodes. In children with respiratory pathology, an X-ray examination of the chest organs is performed. If hemoblastosis is suspected, a consultation with a hematologist is necessary, who will indicate the indications and the need for a puncture biopsy.
Research Based on the main purpose of the work, 164 children (101 boys and 63 girls) aged from 6 months to 16 years were examined. The age of the children is shown in Fig. 2. The largest number of children (76.8%) with lymphadenopathy were admitted to the hospital or were treated as outpatients at the age of 1-9 years. The maximum occurred at the age of 3-9 years. The etiology of the disease was confirmed by a comprehensive examination of patients, which included: microbiological examination of microflora from the oropharynx (before treatment); serological blood test using ELISA and PCR (at the G.N. Gabrichevsky Moscow Research Institute of Epidemiology and Microbiology, NPF "Litekh" for the following diseases: chlamydia, mycoplasmosis, toxoplasmosis, herpes group viruses (I, II, IV, V, VI types) A serological examination was carried out in 164 children, a microbiological examination (throat cultures) in 93 (Fig. 3, 4). Today, knowledge of the prevailing pathogens is fundamentally important. Based on the results of the examination, 2 groups of etiologically significant pathogens were identified - herpes viruses and intracellular. In the herpetic group, Epstein-Barr viruses (61.8%) and cytomegaloviruses (54.9%) predominated; in the intracellular group - chlamydia (49.5%). In the majority of children, lymphadenopathy was of a mixed nature - 126 (76.8 %), while monoinfection was detected in 38 (23.2%). It should be noted that with mixed variants, a combination of 2-4 pathogens was noted: • mixed herpesvirus (EBV, CMV, herpes types I, II) – 30 (18.2%); • mixed intracellular (chlamydia, mycoplasmosis) – 11 (6.7%); • 2 pathogens each: herpes viruses + intracellular – 19 (11.5%); • 3 pathogens each: herpeviruses + intracellular – 34 (20.7%); • 4 pathogens each: herpes viruses + intracellular – 27 (16.5%). “Pure” bacterial lymphadenopathy was detected in only 5 (3%) people.
However, as a result of a comprehensive examination, a combination of positive serological and microbiological markers was revealed - as a result of a mixed course of the disease in 3/4 of the children. It turned out that some pathogens in the same child can simultaneously be in different forms. Table 1 presents the main (predominant) pathogens depending on the severity of the disease. In the acute form of the infectious disease, chlamydia, mycoplasma and EBV predominated in 5.8-11.6% of children. During exacerbation of the chronic course (11.6-21.5%), the same pathogens predominated. A persistent course was identified in most children, especially with CMV, EBV, and chlamydia. Among the predominant pathogens in acute and chronic forms, intracellular pathogens - chlamydia and mycoplasma - stand out. In persistent cases, CMV and EBV predominated. Thus, both in frequency and severity of the disease, chlamydia and Epstein-Barr viruses predominate. When determining cultures from the throat, the main pathogens in the majority were gram-positive cocci: streptococci, Staphylococcus aureus and Neisseria. Considering the presence of a number of pathogens, pharynx dysbiosis can be diagnosed in 82.8% of children. By the number of pathogens: 1 pathogen – in 17.2%, 2 pathogens – in 35.5%, 3 pathogens – in 21.5% (see Fig. 4). It becomes obvious that due to the mixed course of a number of diseases, the children’s history revealed frequent diseases of the ENT organs and lungs: respiratory diseases and bronchitis - in 51 (31.0%), tonsillitis, adenoiditis, otitis - in 21 (12.8%) , past pneumonia – in 5 cases (3%). 11 (6.7%) children were previously hospitalized. Most children from the group with lymphadenopathy are often ill children. The reason for this is the unfavorable course of pregnancy in 16 (9.7%) mothers, due to the presence of various infectious diseases (CMV, chlamydia, ureaplasmosis, herpes, toxoplasmosis, rubella), diagnosed during pregnancy in 17 (10.4%), pyelonephritis - in 10 (6%), ankylosing spondylitis – in 1 (0.6%) and lymphogranulomatosis – in one mother (0.6%). In general, we can distinguish four main groups of children in whom the disease manifested with the following clinical symptoms:
• with respiratory disease, cough – 65 (39.6%); • with enlarged lymph nodes – 60 (36.7%); • with prolonged low-grade fever – 21 (12.8%); • with sore throat 18 (10.9%).
Enlarged lymph nodes were detected both during examination by a doctor and by the children’s parents themselves. Attention should be paid to the fact that 17 (10.6%) children with symptoms of enlarged lymph nodes were not examined for a long time (from 6 months to 2 years). The explanation for this circumstance was a misunderstanding on the part of both doctors and parents that enlarged lymph nodes are not always a “normal phenomenon”, and even more so when its duration is obvious. The majority of children had grade I (50%) and II (48.2%) enlarged lymph nodes, and only 1.8% had grade III enlargement. As a result of the examination, the following clinical diagnoses were established (Table 2). In the table presented, the main diseases include lymphadenopathy and lymphadenitis (37.8%), bronchopulmonary diseases (40.9%), lesions of the oropharynx (18.2%), hematological diseases (3.0%). In recent years, knowledge about the etiology of lymphadenopathy and lymphadenitis has expanded significantly. In previous years, the history of studying the problem of enlarged lymph nodes was closely connected, first of all, with the most studied disease - Epstein-Barr viral infection, which has an acute and chronic course, can occur in the form of infectious mononucleosis or mononucleosis-like syndrome, and is accompanied by a significant increase in parenchymal organs. However, in our study, infectious mononucleosis in only one of 22 children was caused by the Epstein-Barr virus. For all the rest, the etiology was mixed herpetic (herpes types 1, 2 + CMV, EBV + herpes types 1, 2, etc., in combination with chlamydia - in 3 children). As our studies have shown, along with herpes viral infectious agents, one of the main pathogens for lymphadenitis today are chlamydia and mycoplasma.
Specificity of lymphadenopathy of chlamydial etiology The study of lymphadenitis and lymphadenopathy of chlamydial etiology revealed the following features: the disease began with respiratory symptoms. Catarrhal symptoms preceded enlarged lymph nodes 1-2 weeks before presentation. Hyperthermia was observed only in the case of the development of lymphadenitis, i.e., a suppurative process. With chlamydial infection, along with catarrhal symptoms, children (1/3) were identified with mononucleosis-like syndrome. At the same time, the onset of the disease was acute, with a rise in temperature to 38 ° C with moderately severe catarrhal symptoms, difficulty in nasal breathing due to adenoiditis. During this period, children complained of weakness and pain when swallowing. The development of sore throat with plaque on the tonsils after 7-12 days was caused by mixed microflora (strepto- and staphylococci). In 1/3 of the patients with chlamydial infection, the blood count showed monocytosis of more than 15% with an average number of monocytes of 9.2 ± 0.038%. Thus, mononucleosis-like syndrome due to chlamydial infection is practically indistinguishable from that of other etiologies; its etiology can only be determined on the basis of a comprehensive examination. On palpation, the majority of children detected enlarged lymph nodes of grade I - in 82 (50%), grade II - in 79 (48.2%) and grade III in only 3 (1.8%). With grade III lymph node enlargement (polyadenopathy), the lymph nodes were palpated in the form of lymph nodes fused to each other. Conglomerates of lymph nodes of the cervical group were palpated more often during infection associated with disease of the oropharynx. At the beginning of the disease, the consistency of the lymph nodes was elastic. With late admission to the hospital (3-4 weeks of illness), the consistency of the lymph nodes changed - from elastic (at the beginning of the disease) they became denser and more painful. The most accurate examination of lymph nodes (size, consistency, echo density) can only be determined by ultrasound examination. Ultrasound examination of lymph nodes was carried out using an Aloca 2000 device (Japan) with a 7.5 MHz linear sensor and was performed in 54 children. At the same time, conglomerates of cervical lymph nodes of different sizes were determined in 27 (50%), chains of enlarged lymph nodes in the abdominal cavity - in 16 (29.6%), less often - small multiple ones - in 11 (20.3%). The presence of lymph nodes in the abdominal cavity indicates a generalized infection. When analyzing the patient data, a mixed infection was identified in all children. On average, the duration of the disease ranged from 18.5 to 27.5 days (for polyadenopathy). Treatment of children with lymphadenopathy requires a thoughtful attitude and a mandatory comprehensive examination. As shown above, the main pathogens are intracellular pathogens (chlamydia) and herpes viruses (EBV), and various combinations of them. Taking into account the analysis performed, as well as the results of serological and microbiological examinations, the treatment of lymphadenopathy was as follows.
Principle of treatment of lymphadenopathy The main drugs for the treatment of lymphadenopathy in children should be etiotropic drugs that are effective and safe: macrolide antibiotics, aminopenicillins, cephalosporins, antiviral and immunomodulatory ones. The principle of treatment is as follows. If there are pronounced changes in the oropharynx or mild, as well as severe forms, treatment with protected aminopenicillins or cephalosporins should be started without waiting for the test response. After receiving serological and microbiological results (after 5-7 days) and determining the etiology of the disease, treatment with etiotropic drugs (macrolides and antiviral drugs) continues. In mild and moderate forms of the disease, macrolides may be the drugs of choice from the first days of the disease.
Experience in the use of josamycin for the treatment of lymphadenopathy Over the past years, some experience has been accumulated in the use of josamycin in its various forms: suspension in children, tablets in adults. The complexity of treatment also lies in the fact that 25.6% of children before admission to the hospital received: penicillins, cephalosporins, macrolides and antibiotics of other groups. This circumstance should also be taken into account because it is known that dysbiosis develops during antibiotic therapy. In this regard, there is an active search for drugs that minimally affect the normal intestinal microflora. The main groups of antibacterial drugs in the treatment of lymphadenitis were macrolides. In total, 79 children received drugs from the macrolide group: josamycin - 26, midecamycin - 25, roxithromycin - 23, other groups - 4 people. 25 children received cephalosporins, 21 children received aminopenicillins, 39 children received antiviral drugs (33 acyclovir and 6 arbidol). We conducted a comparative study of the effectiveness of the therapy in groups of children receiving macrolides: josamycin (group I), midecamycin (group II), roxithromycin (group III). The duration of the course of antibacterial therapy was 10 days. The effect of the treatment was assessed using a combination of serological and clinical indicators. When assessing clinical data, we took into account the dynamics of lymph node shrinkage, the degree of intoxication, improvement of condition, normalization of blood counts, and the development of dysbacteriosis. The dynamics of serological parameters were assessed before treatment and after 1.5 months by the presence or absence of serological markers. After antibacterial treatment, a positive result was achieved in all groups (Table 3). In the group of children receiving josamycin, only one child on the 3rd day of treatment developed complaints of abdominal pain, which went away on their own and did not require additional prescriptions. The effect of treatment in the other two groups was slightly lower. In each of the other two groups, 2 children had longer persistence of enlarged lymph nodes and persistence of positive serological markers, which required a repeat course of treatment. In case of mixed lymphadenopathy and the presence of herpes viruses, a long course of therapy is recommended with the simultaneous administration of the following drugs: acyclovir, arbidol. Comprehensive therapy should also include immunomodulator drugs: lykopid, viferon, cycloferon. Thus, the diagnosis of lymphadenopathy in children requires the mandatory exclusion of a group of intracellular and herpetic diseases, which are the main ones today. Given the mixed nature of lymphadenopathy in most children, complex treatment is necessary. This group of children requires dynamic observation and control, since 3% of children may have a manifestation of hemoblastosis. The success of treating children with lymphadenopathy will depend on the timely administration of etiotropic therapy in combination with antiviral drugs and immunomodulators.
Symptoms of the disease
The main symptom of the disease is pain in the abdomen (in the upper part or in the navel area). The pain can be paroxysmal and last a long time, it can be dull and not particularly pronounced. Painful sensations become more pronounced with sudden turns of the body, lifting weights, sneezing, coughing. Often there is a feeling of nausea, there may be vomiting, and intestinal disorders.
The presence of an inflammatory process in the body causes signs of intoxication: an increase in the number of heart contractions (tachycardia) and general weakness; body temperature in acute mesadenitis can rise to 390C. In chronic cases, it is usually not high, it can rise to 37 or 37.5 and lasts a long time. With chronic mesadenitis, pain lasts for weeks or months, the child becomes lethargic, tired, and performance and mental activity decrease.
What causes lymphadenitis?
The cause of lymphadenitis in children is always an infection that has entered the body, most often staphylococcal or pneumococcal, which the immune system is not able to cope with. Since the lymph glands are directly involved in protecting the body, they respond to infection by swelling.
Cost of consultation with a pediatrician in Moscow clinics:
- The first clinic of Izmailovo, Dr. Bandurina
1700 ₽
- Family Clinic
1950 ₽
- SM_clinic
2100 ₽
- Make an appointment by phone:
(499) 685-47-75
Another 159 clinics