- Causes of salivary gland cancer and risk groups
- Symptoms of the disease
- Diagnostic methods
- Classification: types of salivary gland cancer
- Stages of the disease
- Treatment
- Complications and relapses
- Life prognosis at different stages of cancer and prevention
The salivary glands produce saliva, a liquid found in the oral cavity that performs some important functions: wetting the mucous membrane, food, facilitating articulation, swallowing, protecting against pathogenic bacteria, etc. There are two groups of salivary glands:
- Large: sublingual, parotid, submandibular.
- Small ones have a microscopic structure, scattered throughout the oral cavity - there are several hundred of them in total.
Cancer can develop in all of these glands. Most often (in 7 out of 10 cases), benign and malignant tumors arise in the parotid salivary glands. Approximately 1–2 tumors out of ten occur in the submandibular salivary glands; in 50% of cases they are malignant. In rare cases, cancer develops in the sublingual or minor salivary glands.
Causes of salivary gland cancer and risk groups
A normal salivary gland cell becomes cancerous when a certain set of mutations occurs in it. The development of malignant tumors is caused by mutations in oncogenes (genes that activate cell reproduction) or tumor suppressor genes (suppress cell reproduction, “repair” damaged DNA, trigger programmed cell death - apoptosis). In each specific case, it is very difficult to judge the reasons for the mutations that occurred in cells. It is impossible to say why exactly they happened.
There are some risk factors that increase the likelihood of developing a malignant tumor:
- The older a person is, the more changes in his genes accumulate, the higher the likelihood of developing various types of cancer.
- Salivary gland cancer is more common in men than in women.
- Irradiation of the head. For example, this may be a previous course of radiation therapy, exposure to ionizing radiation in the workplace.
- There is evidence that the risk of salivary gland cancer is increased in people who have certain occupational hazards: contact with asbestos, nickel alloy dust, work in enterprises that produce rubber and woodworking.
The role of heredity is currently considered insignificant. Most patients do not have a family history (close relatives who have been diagnosed with the same type of cancer). The role of alcohol and tobacco has not been proven. These unhealthy habits are known to increase the risk of head and neck cancer in general, but no association has been found with salivary gland cancers.
Is a mobile phone dangerous? In one study, researchers found that heavy cell phone users were more likely to have parotid tumors (usually benign). But other studies have not found such a relationship.
Causes of parotid gland tumor
The causes of tumor growths of the salivary glands are not fully understood; it is believed that they can be caused by:
- past infections (influenza, scarlet fever, measles and others);
- various chronic diseases, especially diseases of the gastrointestinal tract (the salivary glands are part of a single digestive process);
- eating disorders;
- insufficient oral care;
- genetic factors and unfavorable environmental influences.
Symptoms of the disease
Benign and malignant tumors of the salivary glands present with similar symptoms. One of the main differences is that cancer grows much faster and more often leads to a number of symptoms associated with growth into surrounding tissues and compression of nerves.
You need to visit a doctor if you are bothered by the following symptoms:
- A lump or swelling has appeared in the mouth, cheek, jaw, or neck.
- You have noticed that your face has become asymmetrical.
- I am worried about pain in the mouth, neck, ear, cheek, jaw. It doesn't last long.
- Numbness of part of the face.
- Weakness in the facial muscles, because of this, half of the face may be “lowered,” which becomes especially noticeable when baring teeth or frowning.
- I can't open my mouth wide.
- Difficulty swallowing.
Symptoms
A stone located in the duct of the salivary gland clogs the duct and prevents the flow of saliva into the mouth. In this case, saliva collects in the salivary gland, which becomes swollen and often painful. Depending on the location of the stone, pain and swelling occurs either under the jaw (submandibular gland) or in front of the auricle and in the area of the angle of the jaw bone (parotid gland). Some stones can be removed endoscopically through the mouth under local anesthesia as an outpatient procedure, but sometimes the entire salivary gland must be removed. Most often, stones are found in the submandibular gland.
The tumor is usually palpable as a nodule in the salivary gland and can cause swelling, pain, and facial nerve dysfunction. Even a benign tumor usually must be removed.
Diagnostic methods
During the initial appointment, the oncologist talks with the patient, questions him, trying to find out risk factors, and conducts an examination. The doctor feels the tumor on the face and cervical lymph nodes, evaluates the sensitivity of the face and the work of facial muscles. After this, the patient can be referred for additional consultation to an ENT doctor.
Computed tomography and magnetic resonance imaging help assess the size, shape and location of the tumor, and detect lesions in the lymph nodes and other organs. The current gold standard for searching for distant metastases is PET scanning. If the tumor is located near the jaw, an x-ray is taken. A chest x-ray helps detect metastases in the lungs and evaluate the condition of the lungs and heart before surgical treatment.
The most accurate method for diagnosing salivary gland cancer is a biopsy. During this procedure, the doctor receives a fragment of pathologically altered tissue and sends it to the laboratory for cytological and histological examination.
The most common procedure is fine-needle aspiration biopsy. Tumor tissue is obtained using a hollow needle similar to the one used for injections. If the required amount of tissue cannot be obtained, the doctor performs an incisional biopsy: makes an incision and removes part of the tumor.
If tumor cells are found in the sample, the diagnosis of cancer is virtually certain.
Theory and practical experience in ultrasound diagnosis of salivary gland pathology
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
In domestic and foreign literature there are many works devoted to sialogy (from the Greek Sialon - saliva and logos - study) - the science of diseases and injuries of the salivary glands, methods of their diagnosis and treatment. According to various authors, diseases of the salivary glands account for up to 24% of all dental pathologies. Currently, in clinical practice, the most common are dystrophic, inflammatory diseases of the salivary glands (sialoadenoses, sialadenitis), as well as tumors and congenital malformations of the salivary glands. In addition, pathological changes in the salivary glands often accompany other diseases (diabetes mellitus, bronchiectasis, sarcoidosis, liver cirrhosis, hypertriglyceridemia, lymphogranulomatosis, etc.).
Various instrumental methods are used to diagnose diseases of the salivary glands [1]:
- radiography (if the formation of stones in the ducts of the salivary glands is suspected, but in 20% of the stones of the submandibular salivary glands and 80% of the parotid salivary glands are non-radiographically opaque);
- sialography (examination of the ducts of the salivary glands with a radiopaque substance, is rarely useful in differentiating tumors from inflammatory processes, but it can help differentiate the mass formation of the salivary glands from formations in neighboring tissues. In patients with suspected autoimmune disease of the salivary glands, a characteristic pattern of saccular expansion may be detected ductal system. In case of acute infection of the salivary glands, sialography should not be performed [2]);
- computed tomography together with sialography;
- ultrasound method (is the most accessible, safe and informative in the process of differential diagnosis of the pathological condition of the salivary glands).
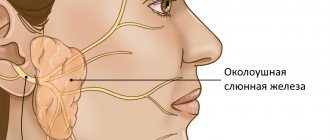
Anatomy of the salivary glands [3]
There are three pairs of major salivary glands (SG) and many small ones. The large ones include paired parotid, submandibular and sublingual SGs. The parotid salivary gland (PSG) is located on the outer surface of the branch of the lower jaw at the anterior edge of the sternocleidomastoid muscle, as well as in the retromandibular fossa. Dimensions vary widely: length 48-86 mm, width 42-74 mm, thickness 22-45 mm. The OSJ is covered by the parotid fascia, which is its capsule and is tightly fused with it. Sometimes, at the anterior edge of the parotid duct, there is an additional lobule measuring 10-20 mm, which has its own duct flowing into the parotid. The parotid duct emerges from the gland at the border of its upper and middle thirds, then it passes along the outer surface of the masticatory muscle parallel to the zygomatic arch and turns 90° inward, penetrating the fatty tissue and buccal muscle. The projection of the parotid duct onto the skin of the cheek is determined on the line connecting the tragus of the auricle and the corner of the mouth. The parotid duct opens in the vestibule of the oral cavity at the level of 1-2 large molars. The diameter of the duct is on average 1.5-3.0 mm, its length is 15-40 mm. The thickness of the gland contains the branches of the external carotid artery, the facial nerve and its branches, and the auriculotemporal nerve. There are many lymph nodes around the OUSG and in its parenchyma (Fig. 1), which can serve as a primary or secondary collector for draining lymph from teeth and oral tissues.
Rice. 1.
Lymph nodes in the thickness of the parotid salivary gland.
The submandibular salivary gland (MSG) is located in the submandibular triangle between the body of the mandible and the anterior and posterior bellies of the digastric muscle. The dimensions of the gland are: anteroposterior 20-40 mm, lateral 8-23 mm, superior-inferior 13-37 mm. Posteriorly, the PNJ is separated from the OSJ by a process of the fascia propria of the neck. The medial surface of the gland in the anterior section lies on the mylohyoid muscle. The submandibular duct, bending over the posterior edge of this muscle, is located on the lateral surface of the hyoglossus muscle. Then it goes between the medial surface of the hyoid gland and the genioglossus muscle to the point of its exit in the area of the hyoid papilla. The facial artery and its branches, the lingual artery and the veins of the same name pass through the gland.
The sublingual salivary gland (SSG) is located on the floor of the mouth in the sublingual region parallel to the body of the lower jaw. The dimensions of the gland are: longitudinal 15-30 mm, transverse 4-10 mm and vertical 8-12 mm. The duct of the parathyroid gland passes along its inner surface and opens in the region of the anterior section of the sublingual ridge independently or together with the submandibular duct. Sometimes the PJS duct flows into the middle section of the PJS duct.
The minor salivary glands - labial, buccal, lingual, palatine, incisive - are located in the corresponding areas of the mucous membrane. They can be a source of development of adenocarcinomas of the oral cavity.
Pathology of the salivary glands
SG malformations are rare. The most common are anomalies in the size of the glands (agenesis and aplasia, congenital hyperplasia (Fig. 2) and hypoplasia), their location (heterotopia, accessory glands), and anomalies of the excretory ducts (atresia, stenosis, ectasia, cystic transformation, ductal dystopia).
Rice. 2.
Hyperplasia of the left sublingual salivary gland.
Sialadenitis is a large group of polyetiological inflammatory diseases of the gastrointestinal tract (Fig. 3). Primary sialadenitis - sialadenitis considered as an independent disease (for example, mumps). Secondary sialadenitis is sialadenitis that is a complication or manifestation of other diseases (for example, sialadenitis with influenza). The echographic picture for different etiologies is not very specific. Etiology has clinical significance in determining treatment tactics.
Rice. 3.
Sialadenitis of the right submandibular salivary gland.
According to the etiological factor, sialadenitis is classified [4] into:
- sialadenitis developing under the influence of physical factors (traumatic sialadenitis, radiation sialadenitis (Fig. 4) occurs during radiation therapy of malignant tumors of the head and neck);
- sialadenitis developing under the influence of chemical factors (toxic sialadenitis);
- infectious sialadenitis (routes of infection penetration into the fluid: stomatogenic (through ducts), contact, hematogenous and lymphogenous);
- allergic and autoimmune sialadenitis (recurrent allergic, Sjogren's disease and syndrome, etc.);
- myoepithelial sialadenitis caused by a pathological process, previously designated as a benign lymphoepithelial lesion. The term benign lymphoepithelial lesion was first used by JT Godwin in 1952, replacing the concept of Mikulicz disease;
- obstructive sialadenitis, which develops when there is difficulty in the outflow of saliva due to obstruction of the excretory duct with a stone (Fig. 5-7) or thickened secretion, as well as due to cicatricial stenosis of the duct. According to the prevalence of the process, they distinguish between focal, diffuse sialadenitis and sialodochitis - inflammation of the excretory duct. The course of the process can be acute or chronic;
- pneumosialadenitis, which develops when there is air in the gastric tissue in the absence of a bacterial gas-forming infection. Air enters the gland from the oral cavity when the pressure there increases through the duct. Pneumosialadenitis is typical for a number of professions, primarily for glassblowers and musicians playing wind instruments.
Rice. 4.
Post-radiation sialadenitis.
Rice. 5.
Stone of the duct of the submandibular salivary gland.
Rice. 6.
Stone in the parenchyma of the submandibular salivary gland.
Rice. 7.
Stone in the duct of the submandibular salivary gland.
Tumors of the salivary glands
Tumors of the salivary glands are divided into two groups: epithelial and non-epithelial. Epithelial tumors predominate in adults (95%). In children with SG, epithelial and non-epithelial tumors are equally common. In addition to true tumors, processes resembling tumors (tumor-like lesions) develop in the GS.
Among epithelial tumors of the gastrointestinal tract, benign neoplasms are distinguished, as well as malignant ones - carcinomas.
Benign epithelial neoplasms of the stomach include ductal papillomas, adenomas and benign sialoblastoma. SG adenomas are divided into two groups: polymorphic (the most common SG adenoma) and monomorphic (all other) adenomas. Tumors of different structure, origin and prognosis were artificially included in the group of monomorphic adenomas.
Pleomorphic (polymorphic) adenoma (mixed tumor of the gland) is a adenoma of the gland, built from two types of cells: ductal epithelium and myoepithelial cells. Macromorphological picture. The tumor is usually an elastic or firm nodule of lobulated grayish-white tissue, usually partially encapsulated. Typical of a pleomorphic adenoma is the so-called chondroid stroma, resembling hyaline cartilage. Variants of the echographic image of pleomorphic adenomas are presented in Figure 8.
Rice. 8.
Pleomorphic adenoma of the gastrointestinal tract.
Warthin's tumor is an adenolymphoma in which multiple cystic cavities are formed, covered with double-layered epithelium. The papillae protrude into the lumen of the cysts. A pronounced proliferation of lymphoid tissue occurs in the tumor stroma. This tumor almost exclusively develops in the parotid gland.
Other types of benign tumors are less common. These are benign oncocytoma (oxyphilic adenoma), basal cell adenoma, tubular adenoma, benign cystadenoma sialoblastoma.
Among benign primary non-epithelial tumors, the most common are hemangioma, lymphangioma, neurofibroma and lipoma.
Among malignant non-epithelial tumors, malignant lymphomas are more often found (they arise, as a rule, against the background of myoepithelial sialadenitis, Sjögren's disease and syndrome).
Tumor-like lesions of the salivary glands
Rice. 9.
Salivary gland cysts.
- Salivary gland cysts (mucoceles). There are two types of mucocele of the gland: the retention type (retention cyst of the small gland, formed when saliva is retained in the excretory duct) and the type of interstitial secretion, when, when the wall of the duct is injured, saliva enters directly into the fibrous tissue surrounding the gland. Mucoceles in the floor of the mouth are also called ranulae.
- Cysts of the excretory ducts of large SGs are pronounced dilatation of the excretory duct due to retention of secretions in it. Blockage of salivary outflow can be caused by various reasons: tumor, stone, thickened mucus, post-inflammatory stenosis, even cicatricial obliteration of the lumen.
- Sialoadenosis (sialosis) is a non-tumor and non-inflammatory symmetrical increase in SF due to hyperplasia and hypertrophy of secretory cells. The outcome of sialosis is often SG lipomatosis. The process has a chronic relapsing course. Sialosis occurs in a number of diseases and conditions: diabetes mellitus, hypothyroidism, malnutrition, alcoholism, liver cirrhosis, hormonal disorders (hypoestrogenemia), reactions to medications (most often antihypertensive), neurological disorders.
Adenomatoid hyperplasia of small SGs leads to their increase to 0.5-3.0 cm in diameter. The causes of adenomatoid hyperplasia are trauma and prolonged exposure to ionizing radiation.
Oncocytosis is age-related changes in secretory cells and epithelium of the ducts of the gastrointestinal tract. In this case, the SF may slightly increase, but usually their value does not change.
To summarize, I would like to note that ultrasound using Doppler sonography in many of our observations helped to accurately determine the nature of the pathological process in the gastrointestinal tract. However, this diagnostic method does not allow one to unambiguously confirm or refute the malignant nature of the formation of the salivary glands.
Literature
- Benign and malignant tumors of soft tissues and bones of the face. A.G. Shargorodsky, N.F. Rutsky. M.: GOU VUNMTs, 1999.
- Topographic anatomy and operative surgery. I.I. Kagan, S.V. Chemezov. M.: GEOTAR-Media, 2011.
- Salivary glands. Diseases and injuries. V.V. Afanasiev. M.: GEOTAR-Media, 2012.
- Inflammatory diseases of the tissues of the maxillofacial area and neck. A.G. Shargorodsky. M.: GOU VUNMTs, 2001.
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Classification: types of salivary gland cancer
The salivary glands are made up of different types of cells, any of which can give rise to a malignant tumor. Therefore, there are different types of cancer:
- Mucoepidermoid carcinoma of the salivary gland is the most common type. Most often it is found in the parotid salivary glands, less often in the submandibular and small ones. These tumors are rarely aggressive.
- Adenoid cystic carcinoma is characterized by very slow growth and rare metastasis. However, this malignant tumor can be very difficult to get rid of: it can recur a long time after treatment.
- Adenocarcinoma is a malignant tumor that develops from glandular cells. Different types of adenocarcinomas can occur in the salivary glands: acinic cell carcinoma, low-grade polymorphic adenocarcinoma, basal cell adenocarcinoma, clear cell carcinoma, cystadenocarcinoma, etc.
- Rare types of malignant cancers of the salivary glands include: squamous cell carcinoma, epithelial-myoepithelial carcinoma, anaplastic small cell carcinoma, undifferentiated carcinomas.
Removal of the parotid, submandibular gland, removal of cervical lymph nodes
The salivary glands are divided into minor and major salivary glands. There are 3 pairs of large salivary glands: the parotid salivary glands, located below and in front of the auricle directly under the skin, the submandibular salivary glands and the sublingual glands, located under the mucous membrane of the floor of the mouth. The minor salivary glands are located in the mucous membrane of the mouth, palate, cheeks and lips. Various tumors, stones, and recurrent infections are the most common reasons for operations on the salivary glands.
Stages of the disease
Salivary gland cancer, like other malignant tumors, is classified into stages according to the generally accepted TNM system. The letter T in the abbreviation denotes the characteristics of the primary tumor: the size and degree of its growth into surrounding tissues, N - spread to the lymph nodes, M - the presence of distant metastases. Depending on these indicators, the following stages are distinguished during salivary gland cancer:
- Stage 0 is “cancer in situ” (carcinoma in situ). The tumor is located within the layer of cells that form the salivary gland and does not grow into neighboring tissues.
- Stage I is a tumor that is located within the salivary gland and measures no more than 2 cm.
- Stage II - the tumor reaches a size of more than 2 cm, but not more than 4 cm.
- Stage III - a tumor that reaches a size of more than 4 cm and/or spreads into surrounding tissues, or a tumor of any size that has grown into surrounding tissues, has spread to one cervical lymph node on the same side, and the focus in the lymph node is no more than 3 cm and does not extend beyond its borders.
- Stage IV includes substages IVA, IVB or IVC. The first two are characterized by varying degrees of spread of the malignant tumor to the anatomical structures of the head, neck, and lymph nodes. If stage IVC is diagnosed, it means that there are distant metastases.
In addition to stages, there are three degrees of malignancy of salivary gland cancer:
- Grade I - low degree of malignancy. Such tumors are called highly differentiated. Tumor tissue is as similar as possible to normal salivary gland tissue. It grows slowly, and the prognosis for such patients is most favorable.
- Grade II are moderately differentiated tumors. Tumor tissue differs more significantly from normal tissue. This cancer is more aggressive and has a poorer prognosis.
- III degree - poorly differentiated tumors. Cancer cells almost completely lose the features of normal ones. Such tumors behave the most aggressively.
Determining the degree of malignancy helps the doctor predict how the cancer will behave and plan treatment correctly.
Performing surgery to remove the salivary gland
With the traditional method of surgery, the patient assumes a lying position with his head thrown back and to the side. The operation involves local infiltration anesthesia. Several parallel incisions are made in the submandibular area, the tissue is lifted, and the capsule of the salivary gland is discovered, which is opened, and the gland tissue is extremely carefully removed and removed. When a malignant tumor grows together with nearby tissues, the latter are also removed. After this, stitches are applied.
During endoscopic surgery, both local and general anesthesia can be used. Through small punctures in the tissue, manipulators and a video probe are inserted, which projects all the actions performed on the screen. When the manipulators reach the gland, small incisions are made with their help, through which pathological tissue is removed. The endoscopes are then removed and sutures are placed at the puncture sites.
Postoperative care of the surgical site includes:
- hygiene - no water or dirt should get into the wounds;
- special diet - the diet will consist of semi-liquid warm food, no hot or cold drinks, no alcohol;
- smoking ban;
- special treatment - it is recommended to regularly treat the seams with antiseptics, and the oral cavity after each meal should be rinsed with a mixture of antiseptic and water.
If all the recommendations of the attending physician are followed, complete wound healing occurs within a few months.
Treatment
The patient is treated by a team of doctors, which may include: a clinical oncologist, an ENT doctor, an oncologist-surgeon, an oral and maxillofacial surgeon, a chemotherapist, a radiotherapist, etc. The treatment program is determined by the stage of cancer, the histological type of the tumor, its location (which gland is affected) , age, general condition and concomitant diseases of the patient.
Surgery
If the tumor has not grown much into the surrounding tissue, then it is resectable, that is, it can be removed surgically. The surgeon’s task is to excise the tumor while capturing the surrounding tissue so that there are no cancer cells left on the cut line, that is, to ensure a negative resection margin. If tumor cells have spread to the lymph nodes, or a biopsy reveals aggressive cancer, the lymph nodes are also removed.
For parotid salivary gland cancer, surgery presents certain difficulties, because the facial nerve passes through the gland, which controls the work of facial muscles. If the tumor affects only the superficial lobe of the gland, you can remove it separately - perform a superficial parotidectomy. There is no risk of damaging the facial nerve. In some cases, it is necessary to remove the entire gland, and if the tumor has grown into the facial nerve, then it too.
For cancer of the sublingual and submandibular gland, the surgeon removes the gland itself and some of the tissue located around it, including, possibly, bone tissue. In some cases, it is necessary to excise the nerves that control sensitivity, movements in the lower part of the face, in the tongue, and the sense of taste.
For cancer of small glands, the affected gland and part of the surrounding tissue are removed. The extent of the operation depends on the size and location of the tumor.
Radiation therapy
Indications for the use of radiation therapy for malignant tumors of the salivary glands:
- To combat malignant tumors that cannot be removed surgically due to their location or size. Sometimes radiation is supplemented with courses of chemotherapy.
- After surgical treatment. This type of radiation therapy is called adjuvant and is sometimes combined with chemotherapy. Radiation after surgery helps destroy remaining cancer cells and prevent recurrence.
- For advanced cancer. In this case, radiation therapy is aimed at combating pain, difficulty swallowing, bleeding and other symptoms.
Radiation is typically given five days a week for 6–7 weeks. If radiation therapy is used for palliative purposes, the course will be shorter.
Chemotherapy
Chemotherapy is used quite rarely for malignant neoplasms of the salivary glands. Anticancer drugs can reduce the size of the tumor, but are not able to completely destroy it. They are most often prescribed for advanced cancer as palliative treatment or in addition to radiation therapy.
Depending on the type and other characteristics of the cancer, the doctor may prescribe combinations of different chemotherapy drugs: carboplatin, cisplatin, 4-fluorouracil, doxorubicin, paclitaxel, cyclophosphamide, vinorelbine, docetaxel, methotrexate. Chemotherapy for cancer is always given in cycles. The patient is administered the drug, then takes a “break” for several days. The course of treatment may consist of several cycles.
Rehabilitation
After treatment, some problems associated with nerve damage may persist: dysfunction of the facial muscles, speech disorders, swallowing, and cosmetic defects. Some side effects of chemotherapy and radiation therapy go away after treatment is completed, while others persist for a long time. In such cases, rehabilitation courses are indicated. The doctor draws up a rehabilitation treatment program individually, depending on the severity and nature of the disorders.
Complications after surgery
During surgery to remove the parotid gland, the facial nerve can be impacted, sometimes causing facial nerve palsy, usually the inferior branch, which can cause the corner of the mouth to droop. Typically, facial nerve paresis recovers within a few weeks with facial exercises, and only in rare cases does the facial nerve fail to recover.
Sometimes the cancer affects the facial nerve and then the facial nerve is completely removed, in which case the paralysis is permanent. However, the condition can usually be improved through various surgical interventions.
After removal of the parotid salivary gland, the pinna of the ear is usually partially numb, but over time some sensitivity returns. Due to the risk of frostbite, the auricle must be properly protected from the cold.
During surgery to remove the submandibular gland, the facial nerve may be injured (stretched), causing temporary dysfunction of the corner of the mouth, but permanent damage caused by this branch of the facial nerve is very rare. Damage to the sensory and motor nerves passing under this gland is extremely rare.
After parotid surgery, saliva may leak from the wound, especially when eating. Salivary secretion is harmless and usually ends spontaneously. Surgery to remove one salivary gland does not cause noticeable dry mouth.
Complications and relapses
Even if the treatment is successful and the examination results show no signs of the presence of cancer cells in the patient’s body, a relapse may occur in the future. Therefore, you need to regularly see an oncologist, come for examinations, undergo various studies and take tests.
Typically, the doctor prescribes examinations once every few months for several years, then less frequently.
- If cancer recurs, treatment options may vary:
- If the tumor can be removed, surgery is performed followed by a course of radiation therapy.
- If the tumor cannot be removed surgically, the doctor prescribes radiation therapy in combination with chemotherapy.
- If there are distant metastases, chemotherapy becomes the main treatment method. Radiation therapy and surgery can be used to control some symptoms.
With advanced cancer with metastases, achieving remission becomes extremely unlikely. In this case, treatment will be aimed at slowing the progression of cancer, combating symptoms, and prolonging the patient’s life.
Euroonco doctors undertake cancer treatment at any stage. For us there are no hopeless patients. You can always help, and we know how to do it correctly, we have all the necessary technologies, the latest generation drugs.
Additional images
- Lower jaw. Inner surface. Side view.
- Distribution of the maxillary and mandibular nerves and submandibular ganglion.
- Mucus cells are identified by the lack of color in their cytoplasm, while serous cells are basophilic in color.
- Inflammation of the submandibular gland on ultrasound
Dissection images
- Submandibular gland
- Submandibular gland
- Submandibular gland, lateral view
- Submandibular gland
- Submandibular gland - right view
- Submandibular gland - front view
- Submandibular gland
- Muscles, arteries and nerves of the neck. Neonatal dissection.
- Muscles, arteries and nerves of the neck. Neonatal dissection.
- Muscles, nerves and arteries of the neck. Deep dissection. Front view.
- Submandibular gland