- Location and functions of the facial nerve
- Causes
- Symptoms
- Diagnostics
- Treatment
- Otogenic neuritis of the facial nerve
- Folk remedies
- Possible complications
- Prevention
Pathology of the facial nerve is registered annually in 2–3 people out of 10 thousand people. It occurs due to various reasons, the nature of which largely determines the treatment of facial neuritis. Taking into account the anatomical connection of this formation and the ENT organs, with neuritis of the facial nerve the patient needs to consult not only a neurologist, but also an ENT doctor.
Facial nerve, anatomy
The facial nerve, nervus facialis , the 7th pair of cranial (cranial) nerves is a motor nerve.
The facial nerve innervates the facial muscles of the face (except for the musculus levator palpebre superioris), as well as the muscles of the auricle and skull, the posterior belly of the digastric muscle (musculus digastricus), the stylohyoid muscle (musculus stylohyoideus), the stapedius muscle (musculus stapedius), the subcutaneous muscle of the neck (musculus platysma).
The nucleus of the facial nerve is located on the border of the lower part of the pons with the medulla oblongata, outward and anterior to the nucleus of the abducens nerve. The axons of the cells of this nucleus rise in the dorsomedial direction to the bottom of the rhomboid fossa, then loop around the nucleus of the abducens nerve located here, forming the internal knee of the facial nerve in the area of the facial tubercle . The root of the facial nerve exits the base of the brain in the cerebellopontine angle between the pons and the medulla oblongata, lateral to the olive, then, together with its companions and the cochlear part of the 8th pair of cranial nerves, enters the internal auditory foramen (miatus acusticus internus), then the nerve and its companions enter facial canal (canalis facialis) of the pyramid of the temporal bone (fallopian canal). The canal initially has a horizontal direction (parallel to the apex of the temporal bone pyramid), then bends vertically. It then opens at the base of the skull with a stylomastoid opening (foramen stylomastoideum). The bend of the facial nerve in its canal is called the “external genu of the facial nerve.” In this place there is the knee ganglion (ganglium geniculi), where the cells of the first taste sensitivity neuron for the intermediate nerve are located. After emerging from the stylomastoid foramen, the facial nerve penetrates the parotid gland and divides into many terminal branches to innervate the corresponding muscles, forming the pes anserinus. The companions of the facial nerve in the canal are the parasympathetic lacrimal fibers - the greater petrosal nerve (nervus petrosus major) and the intermediate nerve (nervus intermedius), the 13th pair of cranial nerves, the Wriesberg nerve.
Parasympathetic lacrimal fibers originate from the secretory nucleus, which is located near the nucleus of the facial nerve. Together with the facial nerve, they enter the facial canal, then are the first to leave it as part of the nervus retrosus major, which innervates the lacrimal gland. Loss of function of the greater petrosal nerve is accompanied by the following symptoms - dry eye, eye irritation, lacrimation.
The intermediate nerve is mixed, consists of efferent parasympathetic salivary fibers for the sublingual and submandibular salivary glands, afferent taste fibers for the anterior 2/3 of the tongue. Salivatory fibers originate from the superior salivatory nucleus (nucleus salivatorius superior), leave the brain in the cerebellopontine angle and enter the facial canal next to the facial nerve, then leave the canal in its descending part as part of the chorda tympani (chorda tympani). Sensitive taste fibers begin from the cells of the knee ganglion, the dendrites of which go in the facial canal along with the facial nerve, then depart from it in the descending part of the canal, participate together with salivary fibers in the formation of the tympanic chord, then enter the system of the 3rd branches of the trigeminal nerve (nervus lingualis ) and reach the taste buds of the anterior 2/3 of the tongue. The axons of the cells of the knee bridle leave the pyramid of the temporal bone through the internal auditory foramen, pass through the cerebellopontine angle and end in the taste nucleus of the solitary tract (nucleus tractussoliterii), common with the glossopharyngeal nerve, located in the medulla oblongata. Damage to the intermediate nerve and the chorda tympani, which is its continuation, leads to hypofunction of the sublingual and submandibular salivary glands and impaired taste in the anterior 2/3 of the tongue. Between the two companions in the facial canal, motor fibers are separated from the trunk of the facial nerve, which form the stapedius nerve (nervus stapedius). The stapedius nerve penetrates the tympanic cavity and innervates the stapedius muscle, which provides a certain degree of fixation of the stapes and tension of the tympanic membrane, which creates conditions for the best audibility. Damage to the stapedius nerve is accompanied by a symptom such as hyperacusis. Hyperacusis is an increased unpleasant perception of sounds, especially low tones.
The first to leave the facial canal is the facial nerve's companion, the greater petrosal nerve. The second branch of the facial nerve to leave the facial canal is the stapedius nerve. The third to leave the facial canal is the companion of the facial nerve - the intermediate nerve in the form of the chorda tympani.
There are features of connections between the facial nerve and the cerebral cortex - the lower third of the precentral gyrus. The upper half of the nucleus, which provides innervation to the facial muscles of the upper part of the face, has a bilateral cortical representation due to the partial supranuclear decussation of the corticonuclear fibers. Fibers to the lower half of the nucleus, from which the facial muscles below the palpebral fissure are innervated, originate from the opposite hemisphere. This point is an important criterion in making a topical diagnosis.
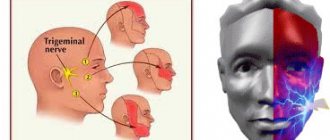
Trigeminal nerve
Trigeminal nerve: symptoms of inflammation and treatment methods
Inflammation of the trigeminal nerve does not threaten the patient’s life, but becomes a real test of fortitude.
The disease is accompanied by painful symptoms and significantly impairs the quality of life. Anxious anticipation of paroxysms of trigeminal neuralgia provokes depression, and some people experience suicidal thoughts. Insomnia is a typical condition for this pathology, which can be caused by both severe pain and deterioration of the emotional background. Among the accompanying changes are decreased performance, fatigue, and frequent headaches. The publication discusses the main causes of trigeminal neuralgia, clinical signs and features of diagnosing the disease, and the main methods of medical and surgical care. The possibilities and methods of treating trigeminal neuralgia using physiotherapeutic methods and folk remedies will be considered.
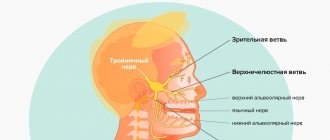
Trigeminal Nerve: Relationship Between Anatomy and Symptoms
The trigeminal facial nerve forms the fifth pair of cranial nerves (cranial nerves). It contains not only afferent sensory fibers, but also motor fibers. Sensory fibers provide superficial and proprioceptive (deep) sensitivity and transmit information to the brain from the skin of the entire face, mucous membranes of the eyes, nose and mouth, muscle and connective tissue structures, teeth and bones of the facial skeleton. Motor fibers go to the masticatory muscles.
Nervus trigeminus received its name due to the peculiarities of its anatomical structure. It is formed by three branches. The first is the orbital nerve. The second is called the maxillary nerve, and the third is the mandibular nerve.
The orbital, also the first branch of the nervus trigeminus, contains only sensory fibers. There are no motor neurons in its composition. The innervation zone includes the frontal zone, temples, eyebrow, upper eyelid, cornea and conjunctiva. Accordingly, with neuralgia of the ophthalmic branch, pain, numbness of the skin and paresthesia are localized in the forehead, eyebrows and eyelids. There may be a weakening or loss of reflexes, the adductor arc of which passes as part of the superior branch (suprabrow reflex, corneal reflex).
The second branch, like the first, contains exclusively sensory afferent fibers. The endings of sensory neurons are directed to the cheekbones and cheeks, wings and back of the nose, and lower eyelids. They also transmit signals from the mucous membrane of the nasal passages, maxillary bone, upper lip and upper teeth. With neuralgia of the second branch, pain, numbness of the skin and paresthesia are concentrated in the central part of the face on the right or left (the pain is always one-sided). Pain in the teeth of the upper row is typical.
The third branch, or mandibular nerve, contains not only sensory fibers, but motor (motor) neurons. This branch transmits information from the lower part of the face - the chin and mandibular bone, teeth, lower lip. Motor fibers transmit signals and coordinate the movements of many masticatory muscles and their antagonists. Also, the efferent fibers of the inferior branch go to the temporal muscle.
When the mandibular branch of the trigeminal nerve is affected, the epicenter of pain, skin numbness, hyperesthesia and paresthesia is located in the lower third. One of the symptoms is weakening or loss of the mandibular reflex. And since the lower branch also contains axons of motor neurons, an attack of neuralgia can be accompanied by motor disorders - spasm or paralysis of the muscles of the masticatory group and their antagonists.
Causes of trigeminal neuralgia
The pathogenesis of trigeminal neuralgia involves compression of one of its branches. The cause of root compression may be infection and inflammation, abnormal location or pathology of blood vessels; less commonly, the cause of compression is a tumor. Trigeminal neuralgia can be a symptom of multiple sclerosis. The following changes in the body and pathological conditions contribute to the development of inflammation of the trigeminal nerve:
- Hypothermia.
- Acute or chronic stress.
- Weakening of the immune system.
- Nervous fatigue and exhaustion.
- Hormonal imbalances.
- Chronic sinusitis, frontal sinusitis.
- Vascular pathology.
- Head injuries.
- The presence of foci of chronic infection in the body.
Very often, the true cause of trigeminal neuralgia is diseases of the oral cavity and teeth. In this regard, odontogenic inflammation of the trigeminal nerve is separately distinguished, which is secondary, and the cause of which is dental pathology. With single-gene neuralgia, as a rule, the maxillary or mandibular branch is affected, and among the symptoms of the disease there is a painful toothache.
Note. In 95% of cases with neuralgia n. trigeminus affects the 2nd or 3rd branches! This indicates a close connection between pathology and dental diseases.
Odontogenic neuralgia of the trigeminal nerve develops with the following dental diseases and anomalies of the development of the dentofacial system:
- Caries.
- Pulpitis.
- Periodontal disease, inflammation of periodontal tissue.
- Gingivitis.
- Osteomyelitis of the jaw bone.
- Retained and dystopic teeth.
- Poor quality dentures.
If you have inflammation of the trigeminal nerve, you must undergo an examination by a dentist to identify the above and other dental diseases. It is extremely important to sanitize foci of chronic infection - cure pulpitis, periodontitis, treat carious teeth, remove retained and dystopic teeth, replace low-quality orthopedic structures (prostheses).
For many patients, oral sanitation has helped to completely cure inflammation of the trigeminal nerve. It is also necessary to undergo an examination by an otolaryngologist, diagnose the paranasal sinuses, and treat chronic sinusitis or sinusitis.
Trigeminal nerve: clinical picture of the disease
The key clinical sign of inflammation of the trigeminal nerve is severe pain. The specifics of pain (localization, character) may differ, but one thing remains unchanged. The pain is always excruciating. Paroxysmal attacks “paralyze” and knock you out of the usual rhythm of life. They can be short-term, lasting no more than a few minutes, and the pain in this case is often shooting in nature. The second option is a constant burning, drilling or cutting pain that exhausts a person for 2-3 days.
Any manipulation on the face can provoke a paroxysm of neuralgic pain. Women, who for some unknown reason suffer much more often from this disease, often provoke a paroxysmal attack by applying decorative cosmetics, and men by shaving. The trigger factor for an attack of trigeminal pain can be even a normal conversation, washing with cool water, or hygiene procedures for caring for the oral cavity or facial skin.
Triggers are actions that provoke the return of paroxysmal pain. They are, as a rule, preceded by some events that happened shortly before that affected the general condition of the body. The true cause of exacerbation of inflammation of the trigeminal nerve can be hypothermia, exacerbation of herpes, colds, nervous fatigue and stress, even eating certain foods (fatty, spicy foods, chocolate, garlic).
The localization of pain depends on which branch is affected by the pathological process. With compression and inflammation of the orbital branch, pain in the upper third of the face dominates in the clinic; with damage to the middle root - in the upper jaw, upper teeth, and cheekbones. When the lower branch is compressed, the epicenter of pain is often localized in the teeth of the lower jaw. In addition, inflammation of the third branch is characterized by motor disturbances - spasm or paralysis of the masticatory muscles on the affected side.
Since the trigeminal nerve innervates one half of the face, pain, paresthesia and motor disorders are always unilateral. The patient complains of pain only on the right or only on the left. Because of this, slight or pronounced facial asymmetry often develops. With neuralgia of the lower branch, there may be a weakening of the bite on the affected side.
The trigeminal nerve contains sensory fibers that are part of the adductor arc of some reflexes. In this regard, with this disease, a decrease or loss of superciliary, corneal or mandibular reflexes is often observed. This symptom is detected during an examination of the patient by a neurologist.
Diagnostics
A preliminary diagnosis of inflammation of the trigeminal nerve is made by a neurologist based on the clinical picture, which includes:
- attacks of acute pain of a burning or shooting nature;
- unilateral localization of pain;
- numbness of the skin, tingling sensation or “pins and needles” on the affected side;
- weakening of reflexes;
- motor disorders with damage to the 3rd branch of the trigeminal nerve;
- vasomotor and secretory disorders (lacrimation, increased salivation).
To confirm the diagnosis, identify the cause of the disease, accurately determine the location of compression and differential diagnosis with other neurological diseases, instrumental examinations are prescribed:
- Computed tomography or MRI of the brain.
- X-ray of the facial skeleton.
- Angiography.
- Electromyography.
- Other.
Inflammation of the trigeminal nerve: treatment methods
The main objectives in the treatment of the trigeminal nerve are pain relief and complete cessation of paroxysms of neuralgic pain. To solve the problems, therapeutic and surgical approaches are used, as well as massage and physiotherapy. Treatment with folk remedies can be used as an additional, but not the main method.
Drug therapy
Drug treatment is carried out using strong painkillers, as well as anti-epileptic drugs. Carbamazepine, an anticonvulsant, helps relieve pain. Muscle relaxants and anti-neurotic drugs may be included in treatment regimens. In severe cases, narcotic analgesics are prescribed.
Painkillers from the NSAID group are ineffective for trigeminal neuralgia. Only the attending physician can prescribe strong analgesics and other drugs, and therefore the patient should contact a qualified specialist as soon as possible.
To reduce swelling and inflammation, hormones from the group of corticosteroids (Diprospan, Hydrocortisone) are included in the treatment protocols for the trigeminal nerve. Corticosteroids have a strong anti-exudative (anti-edematous) and anti-inflammatory effect, due to which rapid positive dynamics are achieved. Antihistamines can be used as an additional antiexudative and anti-inflammatory agent.
Neuroprotectors are also used in treatment to improve the nutrition of nerve cells and promote their recovery. If there are foci of chronic infection, antibiotics are prescribed. When exacerbation of labial herpes occurs, antiviral drugs are prescribed. Treatment regimens often include vitamin injections, vascular medications, antidepressants, tranquilizers and sedatives.
Rehabilitation of foci of chronic infection is mandatory. It is necessary to undergo diagnostics at the dentist, treat existing diseases of the teeth (caries, pulpitis), gums and periodontal tissues. If the diagnosis of neuralgia reveals chronic sinusitis, you need to undergo treatment from an otolaryngologist.
Surgery
In cases where the cause of paroxysmal attacks is compression of the root by a tumor or pathologically altered vessel, surgical treatment is performed. Its goal is to decompress nerve fibers, which is achieved by removing a tumor or moving a blood vessel. For decompression purposes, the nerve root can be isolated from surrounding tissues using a special protective sleeve.
If decompression is impossible or ineffective, surgical treatment has a different goal - complete cessation of impulse transmission along the fibers of the affected nerve. For this, a radiosurgery method can be used, which involves destruction of the sensory nerve, radiofrequency rhizotomy (destruction of the root using electromagnetic influence) or balloon compression.
Additional treatments
Additional methods of therapy include massage, physiotherapy and folk remedies. Massage improves blood circulation and helps reduce swelling, which increases nerve compression during inflammation. Physiotherapeutic procedures include electro- and phonophoresis, ultrasound, pulsed currents, and electromagnetic pulses. Reflexology can have a good effect.
At home, you can use the following traditional medicine recipes:
- Rinse your mouth with a decoction or infusion of chamomile. Rinsing has a minor effect in case of infectious etiology, but does not have an analgesic effect.
- Rubbing fir oil into the area of most severe pain. Can be repeated several times throughout the day to slightly reduce pain. It will not be possible to completely relieve the pain syndrome.
- Rubbing the skin of the affected area of the face with black radish juice. Has a weak analgesic effect.
- Healing clay: apply medicinal clay diluted in vinegar to the affected area. Used as an anti-inflammatory agent.
- Apply marshmallow infusion compresses to the painful area of the face for 30 minutes 1-2 times a day.
The trigeminal nerve is located deep, and traditional medicine cannot have a direct effect on inflamed and swollen tissues. The measures listed above are mainly distracting and auxiliary in nature; they cannot significantly alleviate the patient's condition. Therefore, if trigeminal neuralgia worsens, you should seek qualified help as soon as possible.
You can learn more about the methods of treating neuralgia and inflammation of the trigeminal nerve at the Galaktika clinic (Moscow).
Facial nerve: symptoms, lesion syndromes
When the trunk of the facial nerve, the root of the facial nerve or the nucleus of the facial nerve is damaged, paresis of the facial muscles (muscle paresis) of the same half of the face develops - prosoplegia. Facial asymmetry occurs, which is pronounced even at rest. The entire affected side is motionless and mask-like. The forehead folds and nasolabial folds are smoothed. The palpebral fissure is widened. The corner of the mouth is downturned. Due to loss of function of the circular muscle of the eye (musculus orbicularis oculi), the eye does not close. This is lagophthalmos , or hare's eye. When you try to close your eyes, the eyeball on the affected side turns upward, the iris goes under the upper eyelid - Bell's symptom. With mild paresis of the orbicularis oculi muscle, the palpebral fissure closes, but less tightly than on the healthy side, the eyelashes remain visible (eyelash symptom). When the normal function of the lacrimal gland is preserved, lagophthalmos is usually accompanied by lacrimation, which is caused by difficulty in moving tears to the lacrimal canal due to insufficient adherence of the lower eyelid to the eyeball and impaired absorption due to displacement of the opening of the canal. Also, lacrimation is facilitated by the strengthening of the tear reflex due to the constantly open eye. Inflammatory phenomena, conjunctivitis, and keratitis often develop due to irritation of the eye membranes by air flow and dust.
The asymmetry of the face increases sharply when teeth are shown. The corner of the mouth is pulled back and it is skewed towards the healthy side - this is the phenomenon of the exclamation point, it is associated with paralysis of the musculus risorius. Due to the weakness of the orbicularis oris muscle, whistling and stretching of the lips into a tube are impossible. The patient often has difficulty speaking and eating. Liquid food on the affected side spills out of the mouth, thick food gets stuck between the cheek and teeth. When frowning and wrinkling the forehead, folds do not form on the side of paralysis, it is impossible to puff out the cheeks, and there is no tension on the musculus platysma of the neck. The brow reflex, nasopalpebral reflex, corneal reflex, and conjunctival reflex are lost or weakened. If damage to the facial nerve occurs in a child of the first year of life, then the sucking reflex, proboscis reflex, and search reflex are reduced. As with any peripheral paralysis, atrophy of the facial muscles is possible. When studying electrical excitability and myography, a degeneration reaction is noted.
Peripheral paralysis of the facial muscles is sometimes accompanied by pain in the face, ear, and mastoid process. The pain is associated with the phenomenon of repercussion. Repercussion is the irradiation of excitation from the motor branches of the facial nerve to the sensory branches of the trigeminal nerve.
Prolonged peripheral paralysis can lead to the development of contracture of the affected muscles, which is manifested by a narrowing of the palpebral fissure on the affected side and a pulling of the mouth when baring teeth towards the affected affected side. Symptoms of incipient contracture are often pathological synkenesis of the facial muscles - ocular synkenesis. They are characterized by the following symptoms. The closing of the eyes is accompanied by movement of the corner of the mouth or baring of the teeth. Baring your teeth causes the eye on the affected side to close.
In pathological processes that cause irritation of the nucleus or fibers of the facial nerve, facial hemispasm is observed - this is squinting the eye and pulling the mouth and tip of the nose to the affected side with simultaneous contraction of the chin muscles and tension of the subcutaneous muscle of the neck. Signs of irritation of the facial nerve are also tics of facial muscles and Chvostek's sign.
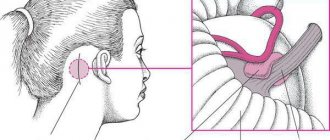
The main nerves of the face and types of damage when injecting fillers
The main nerves that can be damaged during facial injection surgery are the facial and trigeminal nerves. The trigeminal nerve branches into:
- ophthalmic branch;
- maxillary branch;
- mandibular branch.
The trigeminal nerve passes through the openings of the skull and divides into independent sensory components.
Subscribe to our channel on Telegram !
The facial nerve , in contrast, has a single trunk, which passes through the stylomastoid foramen and, at the parotid gland, divides into two branches:
- cervicofacial;
- temporofacial.
The cervical and temporofacial branches are in turn divided into:
- temporal;
- zygomatic;
- buccal;
- marginal branch of the mandible;
- cervical
Nerve damage caused by dermal filler injections can be temporary, reversible, or permanent.
Damage can occur when drugs are administered using either a needle or a cannula. In addition to puncture or partial rupture of the nerve with a needle, it can be damaged as a result of :
- injection of filler directly into the nerve;
- tissue compression after filler injection;
- Too much massage after filler injections.
Nerve damage almost always results in neuropraxia , a loss of sensory and/or motor function.
Diagnosis of the level of damage to the facial nerve
Isolated lesions of the nucleus of the facial nerve are observed quite rarely. It is manifested by total paresis of the facial muscles and occurs in the pontine form of polio.
More often, pathological foci localized in the pons are more common and lead to the involvement of the nucleus of the facial nerve, radicular fibers, and pyramidal tract in the process, which is manifested by alternating Millard-Hübler syndrome. Simultaneous damage to the nucleus of the abducens nerve is manifested by alternating Foville syndrome.
When the pathological process is localized in the cerebellopontine angle, the symptoms of damage to the facial nerve are combined with damage to its companions (the intermediate nerve and the greater petrosal nerve) and the vestibulocochlear nerve. Paralysis of facial muscles in these cases is accompanied by dry eyes - xerophthalmia, impaired taste in the anterior 2/3 of the tongue on the affected side. Xerostomia may be felt - dry mouth, but more often it does not occur due to the functioning of other salivary glands (parotid, sublingual, submandibular on the healthy side). Hyperacusis does not occur due to concomitant damage to the cochlear nerve. Hearing loss or deafness is more common. There may be signs of dysfunction of the trigeminal nerve and abducens nerve located in the immediate vicinity, as well as cerebellar disorders.
When the facial nerve is damaged in the facial canal above the origin of the greater petrosal nerve, dry eyes, taste disorders and hyperacusis develop simultaneously with paralysis of the facial muscles.
The lesion after the departure of the greater petrosal nerve is accompanied by increased lacrimation, taste disturbance, and hyperacusis.
When the facial nerve is damaged below the origin of the stapedius nerve, but above the origin of the chorda tympani, paralysis, lacrimation, and taste disturbance are observed.
Damage to the nerve in the bony canal below the origin of the chorda tympani or after exiting the stylomastoid foramen causes only paralysis with lacrimation.
When the process is localized in the area of the outer knee of the facial nerve with involvement of the knee node, Hunt's syndrome can be detected - this is paresis of the facial muscles (facial muscles), severe pain and herpetic rashes in the area of the auricle (ear).
Sometimes there are cases of bilateral damage to the facial nerve. Bilateral damage to the facial nerves is called diplegia facialis. The patient's face is mask-like, his eyes are half-open, it is impossible to form his lips into a tube or close his mouth.
Facial nerve: treatment in children
Damage to the facial nerve in children is more common than damage to other cranial nerves, which is due to its anatomical features. The facial nerve is supplied with blood from the external carotid artery system, therefore, when the head is hypothermic, spasm of the external carotid artery leads to nerve ischemia, swelling and compression of the facial nerve. Compression of the facial nerve develops especially easily when the process is localized in the narrow canal of the temporal bone pyramid. The facial nerve canal is connected to the tympanic cavity and the pneumatic cells of the mastoid process. The outflow of lymph from the trunk of the facial nerve occurs in the cervical lymph nodes. In childhood, damage to the cervical lymph nodes is often observed.
Facial nerve: causes of damage, causes of neuritis, neuralgia, neuropathy, paresis, paralysis
The main causes of damage to the facial nerve a are inflammatory diseases (diseases) leading to primary damage to the facial nerve and its involvement in the process secondary to pathological changes in adjacent formations. Meningitis, arachnoiditis of the cerebellopontine angle, inflammatory processes in the area of the eustachian tube (eustacheitis) and mastoid process (mastoiditis), inflammation of the ear (otitis), jaw arthritis, lymphadenitis, mumps can cause the development of neuritis, paresis, paralysis, inflammation of the facial nerve. Also the cause of damage to the facial nerve are primary and secondary polyradiculoneuritis. Traumatic damage to the facial nerve occurs during traumatic brain injury with a fracture of the base of the skull in the area of the temporal bone, during surgical operations on the ear. The cause of paralysis and paresis of the facial nerve in children can be birth trauma, the application of obstetric forceps, or facial presentation. The facial nerve suffers from various tumors of the cerebellopontine ganglion region. Neuroma of the facial nerve, Recklinghausen's neurofibromatosis, tumor of the parotid salivary gland, infiltration due to leukemia are also causes of damage to the facial nerve.
In rare cases, congenital aplasia of the facial nerve nucleus and congenital narrowness of the facial nerve canal occur.
Central palsy - facial nerve
Central paralysis of the facial muscles (facial muscles) is observed as a result of damage to the corticonuclear fibers going to the nucleus of the facial nerve. Central paralysis is characterized by dysfunction of the muscles of the lower half of the face, which have unilateral cortical innervation. The main symptom of central paralysis is the smoothness of the nasolabial fold on the side opposite to the lesion. In some patients with central paralysis of the facial muscles, mild deficiency of the orbicularis oculi muscle can be detected. Central paresis of the facial muscles is usually observed in combination with central hemiparesis, or hemiplegia. In contrast to peripheral paralysis, with central paralysis of the facial muscles, the conjunctival reflex, brow reflex, and corneal reflex are preserved, and there is no degeneration reaction.
Symptoms
Symptoms of facial neuropathy make it possible to immediately suspect the disease. Signs arise from the affected nerve. Patients note:
- acute pain: it usually begins in the ear area and gradually spreads throughout the face and begins to radiate to the occipital region;
- intense lacrimation, less often dry mucous membranes of the eyes;
- discomfort or ringing in the ear due to sharp sounds;
- disturbance of the sense of taste in the anterior parts of the tongue.
As the disease progresses, signs of damage to the motor fibers of the nerve appear:
- smoothness of skin folds, especially nasolabial folds;
- swelling of the cheek when exhaling or trying to pronounce a consonant sound;
- lack of complete closure of the eyelids, rotation of the eyeball upward and outward (lagophthalmos);
- leakage of fluid from the corner of the mouth;
- food getting stuck between the gum and cheek when eating;
- limitation of facial expressions: the patient cannot frown or smile.
If the cause of neuropathy is an infectious process, the characteristic signs are accompanied by symptoms of general intoxication:
- high body temperature;
- headache;
- nausea and vomiting;
- weakness.
Primary neuritis of the facial nerve
Primary facial paralysis is caused by herpes viruses, mumps, enteroviruses, and adenoviruses. Bell's palsy can develop with general or local hypothermia of the face. Bell's palsy is characterized by acute development within 3 to 24 hours. The leading role in the development of Bell's palsy belongs to ischemia, which develops due to vasospasm, or vasodilation with the development of swelling of the facial nerve and compression of the nerve.
Often, neuritis of the facial nerve occurs for no apparent reason against the background of absolute complete health. Sarklinik observed many cases where the first symptoms of facial neuritis appeared after a person slept, at the moment of awakening. This may be due to the activation of chronic infection with weakened immunity, the development of various allergic reactions.
Treatment at the Energy of Health clinic
Facial nerve neuropathy requires the fastest and most accurate diagnosis and comprehensive, comprehensive treatment. Only in this case can a rapid restoration of impaired functions be achieved. Neurologists at the Energy of Health clinic use the most effective techniques:
- modern drug regimens that affect the cause of the disease and relieve symptoms;
- physiotherapy courses for tissue restoration;
- massotherapy;
- training in facial gymnastics techniques;
- taping the affected areas;
- observation throughout therapy, adjustment of dosages and medications if necessary;
- a full range of measures for quick and complete rehabilitation;
- organization of sanatorium-resort treatment for the most complete recovery.
Neuritis of the facial nerve secondary
Secondary neuritis of the facial nerve is most often of otogenic origin, observed after or during otitis, mastoiditis, eustacheitis. In these cases, reactive inflammation of the nerve trunk develops. Also, the inflammatory process can penetrate directly into the facial nerve itself due to the penetration of infectious agents into it. This is often observed with purulent epidemic partitis, lymphadenitis of the stylomastoid area. Secondary neuritis of the facial nerve can occur with infectious mononucleosis, toxoplasmosis, typhus, tuberculous meningitis, acute leukemia, cranial polyneuritis, polyradiculoneuritis.
Neuritis of the facial nerve occurs with fractures and cracks of the base of the skull passing through the pyramid of the temporal bone (post-traumatic neuritis of the facial nerve). Hereditary factors and congenital developmental anomalies play a major role in the occurrence of paresis of the facial muscles. There are aplasia of the facial nerve trunk and aplasia of the nucleus of the facial nerve. In this case, there may be unilateral and bilateral violations.
The occurrence of neuritis of the facial nerve is facilitated by a narrowing of the fallopian canal and an increase in the size of the styloid process.
Damage to the facial nerve can be one of the signs of such syndromes as Melkersson-Rosenthal syndrome, Mobius syndrome.
Neuritis of the facial nerve diagnosis
Diagnosis of facial nerve neuritis is based on an analysis of the symptoms preceding and accompanying diseases of the nerve damage. Neurologists, neuropathologists, and reflexologists distinguish such forms of damage as neuritis of the facial nerve and neuropathy of the facial nerve. According to pathogenesis, neuritis is divided into primary and secondary.
Neuritis of the facial nerve must be differentiated from isolated damage to the motor nucleus of the nerve, a variety of common pathological processes in the area of the cerebellopontine angle. Damage to the nucleus of the facial nerve is accompanied by isolated paresis of the facial muscles of the same half of the face without autonomic and sensory disorders, which occurs mainly in the pontine form of poliomyelitis or poliomyelitis-like diseases, tick-borne encephalitis.
When the lower parts of the bridge are damaged, which occurs with tumors, encephalitis, vascular diseases, along with the nucleus of the facial nerve, the pyramidal tract is involved in the pathological process. In such cases, peripheral paresis of the facial muscles is combined with central hemiparesis of the opposite side (Millard-Hübler syndrome). If the nucleus of the abducens nerve is affected, then paresis of the external rectus muscle of the eye (Fauville syndrome) is added to the above symptoms.
Isolated neuritis of the facial nerve is differentiated from processes in the area of the cerebellopontine angle, which develop, for example, with arachnoiditis, tumors of the vestibulocochlear nerve, which is manifested by decreased hearing, deafness, paresis of the facial muscles, sometimes dysfunction of the trigeminal nerve, contralateral spastic hemiparesis.
Polyneuritis and polyradiculoneuritis often involve lesions of the facial nerve. Usually the lesion in these cases is bilateral, often asymmetrical, accompanied by limited or diffuse damage to other parts of the human peripheral nervous system.
Anatomy of the nerves in the cheek area
The location of the infraorbital foramen in the cheek area is critical to prevent neuropraxia. Damage may occur due to an infraorbital nerve . Fortunately, most fillers include lidocaine, which reduces the need for n. infaorbitalis in this zone. However, such anesthesia may be necessary for upper lip augmentation. Injecting an anesthetic into the eye socket, as well as too strong massage after injection of filler, can lead to:
- diplopia;
- dysesthesia;
- paresthesia.
There are known cases of Bell's palsy after injections of dermal fillers. In most patients, improvement occurs spontaneously (71%), but in a fairly large percentage of victims, residual weakness of one half of the face persists for life.
You may also be interested in: First aid for central retinal artery occlusion after filler injections
Emergency treatment for Bell's palsy is a short course of oral steroids. Surgical decompression and other treatments such as electrography, physical therapy and acupuncture are not supported by sufficient evidence.