Causes of inflammatory damage to the trigeminal nerve
Factors contributing to inflammation of the trigeminal nerve are:
- surgical interventions on the jaw bones;
- fractures of the base of the skull, lower and upper jaws;
- tumors;
- complex tooth extraction;
- hypothermia;
- surgery on the maxillary sinus;
- improperly administered anesthesia;
- incorrectly performed dental prosthetics;
- metabolic disorders;
- the presence of foreign bodies that irritate the nerve trunk or injure nerve endings;
- bacterial or viral infection;
- various types of intoxication of the body;
- hypovitaminosis;
- weakening of the immune system.
Causes of inflammation
Primary neuritis of the facial nerve occurs due to:
- hypothermia of the face, cold, wind, drafts;
- insufficient blood supply (ischemia) to the nerve.
Secondary neuritis of the facial nerve is caused by the following reasons:
- inflammatory diseases of the ear: otitis media, eustachitis, mastoiditis;
- infections: mumps virus, measles, herpes;
- traumatic brain injuries;
- vascular disorders - for example, atherosclerosis of the vertebral arteries;
- brain tumors;
- anesthesia of the inferior alveolar nerve by the dentist.
Other factors that provoke inflammation include:
- traveling on a bus or minibus next to an open window;
- long work under air conditioning;
- metabolic disorders in the body;
- endocrine diseases - for example, diabetes;
- hypertension, intoxication of the body;
- nervous stress, emotional instability.
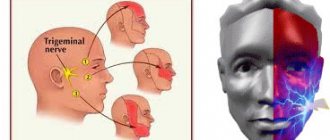
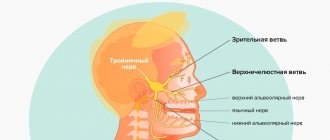
Symptoms of trigeminal neuritis
The maxillary trigeminal nerve consists of three types of nerve fibers:
- vegetative;
- motor;
- sensitive.
The symptomatic picture of neuritis may vary depending on which fibers were affected by the inflammatory process.
Damage to sensory fibers
In particular, with inflammation of the sensory fibers, the patient may complain of a tingling sensation, numbness, and weakened sensitivity in the area innervated by the trigeminal nerve.
Damage to motor fibers
When motor fibers are damaged, there is a partial or complete decrease in strength in the innervated muscles, their atrophy and deterioration of tendon reflexes.
Damage to vegetative fibers
When the vegetative fibers are inflamed, the patient experiences cyanosis and swelling of the skin, dryness and thinning of the skin, and the potential risk of developing a trophic ulcer increases.
How does neuritis of the facial nerve appear?
Neuritis of the facial nerve can begin with mild pain in the ear area. Simultaneously with the onset of pain or after a couple of days, the facial muscles partially or completely lose mobility. The patient's face becomes distorted, the affected part freezes in the mask.
With timely treatment, the patient has a great chance of recovery - in 75% of cases the disease goes away completely. If facial paralysis does not resolve within three months, the patient's chances of making a full recovery are greatly reduced.
In order for facial neuritis to pass without consequences, you need to consult a doctor in the first hours after the onset of symptoms.
Pain due to inflammation
In addition, a disease such as inflammation or neuritis of the facial trigeminal nerve makes itself felt with attacks of pain of a very diverse nature:
- cutting,
- burning,
- pricking,
- tearing
- shooting, etc.
In this case, the area of pain does not always correspond to the area of innervation and can spread to the lower jaw, cheeks and chin.
Pain may be accompanied by:
- muscle spasms (facial, chewing),
- the appearance of nasal discharge,
- development of hypersalivation,
- increased lacrimation.
Lack of sensation in the tongue, lips and chin
With inflammatory damage to the trigeminal nerve, not only the entire nerve can be damaged, but also its individual branches. This is why numbness and pain can occur in various areas of the face. For example, when the lingual branch of the nerve is inflamed, patients complain of pain and sensitivity disturbances in the anterior part of the tongue, and when the mental branch is damaged, in the area of the lips and chin.
Pain when laughing, chewing, brushing teeth and shaving
Pain due to neuritis of the maxillary trigeminal nerve can intensify with touching, chewing, laughing and with changes in temperature. That is why patients, trying to prevent the recurrence of painful attacks, avoid excessive mobility and prolonged conversations, and refuse brushing their teeth and shaving.
Complications of the disease
Neuritis of the facial nerve can lead to contracture of the facial muscles. It appears 4-6 weeks after the onset of the disease due to incomplete restoration of the motor functions of the facial muscles. Contracture is a contraction of the muscles of the affected half of the face. At the same time, it seems that it is not the diseased part of the face that is paralyzed, but the healthy one.
To avoid complications of inflammation of the facial nerve, you need to consult a doctor in time. For prevention, we recommend doing facial exercises. You will find examples of exercises at the end of the article.
Treatment of neuritis of the maxillary trigeminal nerve
Therapy
The treatment program for trigeminal neuritis is drawn up taking into account the causes of the disease and its clinical signs. The main goals of treatment are:
- achieving a sensitizing effect;
- fight against bacterial and viral infection;
- increasing the body's immune forces;
- elimination of swelling of the nerve trunk;
- restoration of natural adaptive and compensatory reactions;
- normalization of the patency of nerve impulses.
Healing procedures
The set of procedures aimed at blocking the inflammatory process and eliminating all manifestations of neuritis includes:
- antibacterial therapy;
- antiviral therapy;
- elimination of factors contributing to the occurrence of intoxication;
- removal of tumor-like neoplasms or dissection of adhesions compressing the nerve;
- prescribing vitamin and mineral complexes to the patient;
- stimulation of nerves and muscles;
- acupuncture;
- physiotherapy (electrophoresis, phonophoresis, UHF, ultrasound, paraffin therapy).
People suffering from trigeminal neuritis are advised to regularly visit dental clinics and have their oral cavity sanitized.
Surgery
Surgical treatment of facial nerve neuritis is usually carried out to restore its integrity, damaged by injury (rupture of nerve fibers). For this purpose, the nerve is sutured.
In addition, surgery may be performed if the cause of nerve inflammation is compression by a tumor, aneurysm, scar tissue, or other neoplasm. The cause of the compression is removed (an example of such an operation is neurolysis - removal of connective tissue proliferation).
Another type of surgical treatment is replacing the damaged portion of the facial nerve with a graft. Such operations are usually performed for injuries. The section of nerve to be transplanted is taken from the leg. The volume of plastic surgery is determined by the surgical plan. In particular, the transplant can be sutured to the facial nerve on the healthy half of the face. In this case, the signal from the brain will arrive to the facial muscles simultaneously on the right and left sides.
Surgical treatment is indicated in cases where conservative therapy does not bring results. It can be carried out within 12 months from the onset of symptoms of neuritis. Carrying out the operation later does not make sense, since by this time the facial muscles have time to atrophy.
Prevention
There is no specific prevention against neuralgia. Doctors only recommend eliminating as much as possible exposure to the body of those risk factors that can lead to nerve inflammation. To avoid this, it is necessary to prevent hypothermia of the face, especially in the summer when using fans and air conditioners. It is important to harden yourself and worry less in order to reduce the impact of stress. It is also imperative to treat underlying diseases that are risk factors for neuralgia.
Symptoms
The first attack of pain can be triggered by elementary things that no person can do without: laughter, smiling, articulation, brushing teeth, eating, frostbite on the face. Pain appears in one half of the face. At first, the painful attacks are short-lived. They end, just as they begin, abruptly. Over time, pain occurs more frequently and lasts longer. Often the pain begins to originate in the jaw and can be confused with toothache. Then the painful sensations move to the area of the cheek, ear, and forehead. There is lacrimation, paresis of the facial muscle, and the face becomes asymmetrical. After the attack, a period of remission occurs, which lasts several minutes. During remission there is no pain.
Home remedies
Before treating trigeminal neuralgia at home, you should consult a doctor, since many remedies can only worsen the situation. If the specialist allows it, it is also possible to use various home recipes.
According to recommendations for trigeminal neuralgia, it is worth consuming orally or lubricating the affected side with birch sap. You need to drink 4-5 glasses per day. Heated buckwheat folded in cotton cloth will help relieve pain. The compress is made 2 times a day, keeping it at the site of inflammation until it cools down. At home, it is useful to massage the sore area: rub, stroke and lightly knead the area of inflammation.
Diagnosis of neuralgia
Diagnosis of neuralgia in the CELT Clinic does not cause difficulties, since it has a number of pronounced signs. When talking about the clinical manifestations of the disease, patients try not to touch the affected side of the face and remain in a tense state because they expect a new attack.
Studies are carried out on the functions of the facial and trigeminal nerves, which begin with assessing the symmetry of the patient’s face. In addition, a number of tests are carried out to check taste and sensitivity.
For the most accurate diagnosis of pathological processes in the nerves of the face, an ultrasound scan of the nerves is performed.
Hemifacial spasm (facial hemispasm) - symptoms and treatment
The main goal of treatment for hemifacial spasm is to achieve stable remission without losing the patient’s ability to work and social activity [25].
medications are used to treat hemifacial spasm : clonazepam, levetirace, carbamazepine, baclofen, gabapentin [7]. They belong to anticonvulsants and muscle relaxants, affecting muscle tone and the ability to conduct nerve impulses. However, their effectiveness has not been reliably proven. In addition, patients are forced to take drugs for a long time in fairly high doses, which inevitably leads to side effects such as lethargy, drowsiness, lethargy, dizziness, muscle weakness, dyspeptic disorders, fluctuations in blood pressure, rhythm disturbances and cardiac conduction, and many others. which affects the quality of life.
For primary hemifacial spasm, neurosurgical intervention (microvascular decompression of the facial nerve) is possible, which has shown its effectiveness in 86-93% of cases of surgical treatment. It was developed and first performed in February 1966 by the American neurosurgeon Peter Jannetta [7]. First, the doctor makes an incision in the area behind the ear on the affected side, then cuts out a small area of bone. Having displaced the cerebellar hemisphere, the doctor determines the compression zone and eliminates it: delicately separates the vessel from the nerve and places a special biologically inert material - Teflon wool - between them. The bone defect is replaced with a bone fragment or a special plate, which is firmly fixed.
For secondary hemifacial spasms, it will be effective to eliminate the cause (removal of the tumor, exclusion of the aneurysm from the bloodstream, treatment of the underlying disease, etc.).
In the presence of contraindications to surgical treatment, in case of secondary hemifacial spasm, when surgical treatment is not indicated (stroke, multiple sclerosis, etc.), refusal of surgery, and in elderly people, injections of botulinum toxin type A (BTA) [1 ][7]. According to the recommendation of the European Federation of Neurological Societies (EFNS, 2011), BTA drugs are recommended as the first line of treatment for hemifacial spasm (recommendation class C) [28].
BTA is a highly effective treatment method for hemifacial spasm with minimal risk of adverse events and can be considered as an alternative to surgical treatment. It has been verified by controlled studies and 35 years of clinical practice [26]. Moreover, it is known that in 20% of cases of surgical treatment of hemifacial spasm, a relapse develops; side effects are frequent (impaired functions of the cranial nerves, infections, liquorrhea, hemorrhages), which are more difficult for patients to tolerate than BTA [7].
Californian ophthalmologist Alan Scott first used BTA in 1977 to treat strabismus. In 1985, he was the first to use local injections of BTA in humans for the treatment of blepharospasm and hemifacial spasm [29]. In 1985, neurologist Mitchell Breen published results of successful treatment of blepharospasm and hemifacial spasm using BTA [30]. Since then, BTA has been used not only in ophthalmology, but also in the treatment of diseases of the nervous system. The use of BTA was officially approved by the FDA (Food and Drug Administration - USA) in 1989. One of the first indications for the use of BTA was hemifacial spasm [31].
Botulinum toxin is produced by the gram-positive bacterium Clostridium botulinum. It is a neurotoxin that blocks the release of acetylcholine (a neurotransmitter that mediates the transmission of signals between neurons) from the presynaptic nerve ending. Thus, peripheral cholinergic (excited by acetylcholine) transmission at the neuromuscular synapse is disrupted. This reduces muscle contraction and leads to a dose-dependent, reversible decrease in muscle strength [25][26].
In Russia, the following BTA preparations are approved for use: conditionally 100-unit - "Botox", "Lantox", "Xeomin", "Relatox", "Botulax" (some drugs are available in bottles of 50 and 200 units) and " Dysport" (in bottles of 300 and 500 units). The drugs have similar effectiveness; they differ in storage and dilution features. Only in the instructions for the drug "Relatox" (Russia) hemifacial spasm is not included in the indications for use. The dosage of the drug is calculated individually for each patient and in accordance with the instructions for medical use. The conversion factor for units of action between Dysport and 100-unit drugs has been scientifically calculated; it is 3:1 or less for neurological indications and 2.5:1 for aesthetic indications [32]. The final dose calculation remains with the doctor. In Wolfgang Jost's atlas of botulinum therapy, doses are already indicated taking into account this recalculation per point of administration [33]. When treating hemifacial spasm, the average dose for Dysport can be 120-170 units. [14], for Xeomin - 30-50 units. depending on the muscles involved. The dose of administration at one point for Xeomin is 1.25-5 units. [33][34].
BTA is able to eliminate hyperkinesis during hemifacial spasm while preserving muscle function; it must be prescribed as soon as the diagnosis is made. Before carrying out botulinum therapy, the doctor must obtain voluntary informed consent for BTA injections. Injection sessions are recommended every 3-4 months in the target muscles. It is permissible to carry out injections “at the patient’s request,” that is, earlier or later than the recommended dates. This depends on the resumption of hemifacial spasm symptoms. After injections, it is recommended to actively contract the injected muscles for 20 minutes, and the patient should be under medical supervision for 1 hour to monitor for immediate allergic reactions [26]. To reduce the risk of developing intradermal hematomas on the face, it is recommended to cool the injection sites for 10-20 minutes.
A decrease in hyperkinesis after the administration of botulinum toxin is usually observed quite quickly - already on days 2-5, sometimes reaching the maximum effect by the end of the week (less often by days 10-14). The effect lasts up to 3-6 months. With regular repeated administrations of BTA, in most cases the positive effect is consolidated. The severity of hyperkinesis when they resume is less than before botulinum therapy and tends to decrease [14]. For facial symmetry in the muscles contralateral (on the opposite side) to the hemifacial spasm, it is necessary to perform BTA injections at 50% of the dose administered into the ipsilateral (on the side of the disease) muscles. It is advisable to do this after 2-3 weeks to evaluate the effect of the injected BTA and identify the muscles requiring aesthetic correction [35]. There is usually no decrease in sensitivity to BTA. Against the background of the effect of therapy, there is the possibility of gradual withdrawal of previously received medications [14][34].
More often, injections are performed in the following muscles: the circular muscle of the eye (orbicularis oculi); zygomaticus minor (zygomaticus major et minor); circular muscle of the mouth (orbicularis oris); subcutaneous muscle of the neck (platysma); frontal muscle (frontalis); muscle that wrinkles the eyebrow (corrugator supercilii); muscle that lowers the nose (procerus); nasal muscle (nasalis); muscle that lifts the upper lip and wing of the nose (levator labii superioris alaeque nasi); muscle that lifts the upper lip (levator labii superioris); laughter muscle (risorius); muscle that lifts the angle of the mouth (levator anguli oris). The drug should not be injected into the middle zone of the upper eyelid - in the projection of the muscle that lifts the upper eyelid, as this can lead to drooping of the eyelid [26][28].
Treatment with the drug should be carried out by specialists (neurologists, neurosurgeons) who have experience in the diagnosis and treatment of such conditions and have been trained in the treatment.
Contraindications to the use of BTA include pregnancy, hypersensitivity to one of the components of the drug, and acute diseases [26]. In the treatment of hemifacial spasm, according to various authors, temporary adverse reactions . They are distributed according to frequency as follows: very often - ptosis (drooping); often - weakness of the facial muscles, diplopia (double vision), dry eyes, swelling of the eyelids, lacrimation; infrequently - paresis (weakening) of facial muscles; rarely - ophthalmoplegia (paralysis of the eye muscles), entropion of the eyelid [26]. They do not require additional interventions and regress on their own within a few weeks [14][26][34]. To reduce the risk of side effects, it is important to maintain the dose of BTA and begin treatment with the minimum effective doses. Drugs that affect neuromuscular transmission, such as aminoglycoside antibiotics, should be used with caution during the period of BTA action [26].
To assess the effectiveness of treatment, scientists have developed a special system using five- and six-point scales. For example, according to Vincent Marneffe (neurosurgeon) [36], the result is considered “excellent” with the complete disappearance of hyperkinesis, “good” - if the disappearance is more than 80%, “satisfactory” - if the disappearance is from 20 to 80%, “unsatisfactory” - if hyperkinesis disappeared by less than 20%. Tetsuo Iwakuma et al [37], Peter Giannetta [21], Robert Auger et al [38] suggested “excellent,” “good,” “satisfactory,” “unsatisfactory,” “poor,” and “recurrent” results for the treatment of hemifacial spasm. One should strive to achieve “excellent” and “good” treatment results [7].
Drug therapy for hemifacial spasm is a thing of the past. Only in the presence of comorbid disorders (depression) can a doctor prescribe antidepressants in addition to the main treatment [25][26].
Thus, the use of BTA requires visiting a doctor 3-4 times a year without the need to constantly take other medications and undergo other procedures. It is also necessary to conduct cognitive behavioral therapy with patients for better social adaptation [25][26].
Facial hemispasm. Paraspasm. Blepharospasm
These are diseases similar to diseases of the facial nerve. Even doctors often confuse them. We will definitely understand the causes of the disease and provide the necessary treatment.
Facial hemispasm is attacks of involuntary contraction or twitching of the facial muscles on one side, similar to a nervous tic of the eye (read more about the causes and treatment of neural tics (including the eyes) here). It may look like squinting, closing your eyes, retracting the corner of your mouth or tip of your nose, or lowering your chin. More information about nervous tics (including the eyes and its causes)
Facial paraspasm is an attack of involuntary contraction of facial muscles on both sides. It occurs much less frequently than hemispasm and more often has common causes with it. More details
Blepharospasm is a disease that begins with rapid blinking, which subsequently develops into intense uncontrolled squinting of the eye or both eyes. More details
We will be happy to help you find the cause and treatment of facial hemispasm (nervous tic of the eye), facial paraspasm, blepharospasm.
Treatment of the facial nerve at the Echinacea clinic
The treatment will be structured like this:
- Find and eliminate the factor that damaged the nerve (viruses, for example);
- Stimulate nerve regeneration.
If you neglect the first point, the chances of restoring the nerve are reduced, and the risk of facial contracture increases. The average duration of treatment is 2 months; you can complete most of the course at home on your own.
The planned result is restoration of the functioning of the facial muscles. Possible difficulties are advanced disease, significant narrowing of the facial nerve canal, damage to the myelin sheath of the nerve, leading to the appearance of a nervous tic of the eye, which to some extent complicates the treatment process. Read more about the causes and treatment of nervous tics.
Treatment of neuralgia
Treatment of neuralgia is a long and difficult process, but doctors at the CELT Pain Clinic know how to carry it out with maximum positive effect. For this purpose it is used for the treatment method.
Conservative method
Conservative treatment involves taking medications:
- antispasmodics;
- anticonvulsants
Radiofrequency rhizotomy
- Cost: 35,000 rub.
- Duration: 15-30 minutes
- Hospitalization: 2 hours in hospital
More details
It is very important to correctly calculate the dosage of medications and take them regularly, since this is the only way to achieve the desired effect. It is equally important to regularly attend physiotherapeutic procedures:
- Bernard currents;
- acupuncture;
- paraffin applications.
If this treatment method does not bring the desired effect, the attending physician may decide on surgical treatment.
Examination for facial nerve disease - find and eliminate the cause of the disease
The symptoms of facial nerve pain are almost the same in all cases, but its causes are different and require different treatments. Treatment “blindly” can delay the healing process. Therefore, in our clinic everything starts with searching for the exact cause and location of the nerve damage.
MRI of the brain, temporal bone. MRI scans show the brain centers of the facial nerve and its area of exit (root) to the base of the brain, blood vessels, and temporal bone. Circulatory disorders, cysts and tumors are easily recognized.
Blood tests to check for infections, biochemical changes that damage the facial nerve. The trigeminal nerve is a favorite area of attack by the herpes virus group. The suspicion of the presence of the virus and its activity can be easily verified using a blood test.
Electromyography, Blink reflex - measurement of electrical potentials of facial muscles. Helps assess the function of impulse transmission along the facial nerve, the degree of its impairment, judge the effectiveness of treatment, the presence of complications, and help in choosing the correct treatment tactics.
Stimulation electromyography of the facial nerve (electroneuromyography, myography of the facial nerve)