Metastases in the bones can develop in absolutely any malignant process; for some cancers this is an almost obligatory localization, while for other diseases it is rare. In the metastatic ranking, first place in terms of frequency of occurrence will go to lung metastases, second to liver foci, and third to skeletal metastases.
Metastases in the bones are difficult to treat and promise pain; however, skeletal foci, less than other tumor localizations, shorten life, but can ruin it with a fracture or compression of the spinal cord.
- What types of bone metastases can there be?
- What cancers develop?
- When do skeletal metastases appear?
- Which parts of the skeleton are most often affected?
- Clinical manifestations of bone metastasis
- Why does pain occur?
- How are bone metastases detected?
- Treatment of skeletal lesions
- Why are bisphosphonates needed?
What types of bone metastases can there be?
According to clinical and radiological characteristics, all bone lesions are divided into three groups:
- osteoblastic - with a predominance of compaction beyond the physiological measure, but additionally grown tumor tissue does not impart strength to the bone and can compress the nerves passing nearby;
- osteolytic - destruction of the structure prevails and the likelihood of a fracture increases as the cancer grows;
- mixed - a combination of two types and this situation occurs most often.
It almost never happens that a patient has exclusively osteolytic or only osteoblastic foci; as a rule, a combination with a predominance of either a sparse lytic or an excessive blastic structure is diagnosed.
What cancers develop?
The leader among all malignant processes occurring with metastatic lesions of the skeleton is myeloma - bone destruction begins at the very beginning of the disease and in 100% of clinical cases multiple destruction of bone tissue is noted.
In case of breast and prostate cancer, skeletal metastases are diagnosed in two thirds of patients, and pathological observations reveal the involvement of bones in the malignant process in almost 90% of patients. In breast cancer (BC), mixed and osteolytic variants predominate; in prostate cancer, osteoblastic variants predominate.
A high frequency of bone metastases is observed in lung cancer, but in the small cell variant there are twice as many bone defects, while in the non-small cell variant it occurs in 40% of patients with a tendency towards single or solitary lesions, that is, a single one.
Every fourth person suffering from kidney cancer has skeletal metastases; in bladder carcinoma, bone tumors are much less common.
In case of colon cancer, bone metastasis is detected in every eighth patient, in case of stomach cancer - not often, since the cancer affects the liver and abdominal cavity earlier and more abundantly. Colon cancer tends to be small-focal and multiple secondary formations.
Book a consultation 24 hours a day
+7+7+78
When do skeletal metastases appear?
In malignant processes, the time of appearance of bone metastases varies, while the rate of growth of the lesion depends solely on the individual biological characteristics of the tumor tissue, which change under the influence of treatment and as cancer disseminates.
At the initial treatment, bone lesions in the absence of other manifestations of the cancer process are present in hardly 20% of patients; in the vast majority of cases, tumor lesions of the bones are a sign of cancer dissemination—spread across systems or generalization. This is exactly what happens with breast cancer, non-small cell lung carcinoma and colon cancer.
In prostate cancer, skeletal pathology is often detected simultaneously with a prostate tumor or shortly after the diagnosis of problems in the gonad.
In kidney carcinoma, metastases are often first found in the bones and lung tissue, and then the primary tumor is discovered.
Classification of myeloma
Myeloma is a heterogeneous group of diseases, some of which may remain stable for years, while others progress rapidly.
- Plasmacytoma. The term bone myeloma is most appropriate for her. It is characterized by single foci of osteodestruction, responds well to treatment and can exist in a stable state for many years and even decades. But in most patients, it eventually disseminates throughout the body, transforming into multiple myeloma.
- Smoldering myeloma. With it, bone damage is not detected, but in the bone marrow the number of plasma cells exceeds 10%, and M-protein is detected in the blood in values of more than 30 g / l. This condition may also remain stable for several years.
- Symptomatic myeloma. There is already a detailed clinical picture here; the disease is characterized by rapid progression and an unfavorable prognosis.
Which parts of the skeleton are most often affected?
The localization of bone metastases is determined not by the nosological affiliation of the primary malignant tumor, but by the functional load and the associated development of the blood supply. Multiple foci in the skeleton are more typical for highly aggressive cancer, single and especially one metastasis indicates a favorable prognosis of the disease.
- Most often, secondary cancer screenings occur in the spongy bones, the vertebrae, which are abundantly fed with blood, and mainly in the lumbar and thoracic spine, which are under high load.
- Next in frequency are metastases in the pelvic bones - almost half of all cases, typical locations are the ilium and pubic bones.
- Metastasis is half as common in the bones of the skull and lower extremity, where damage to the femur predominates.
- The chest, mainly the ribs and sternum, are involved in the malignant process in almost 30% of cases.
Psychological support
Cancer is always a serious stressful situation associated with a strong negative emotional shock. A person who is faced with this disease should be surrounded by his family and friends and provide him with full support. In addition, professional psychological assistance is also important, which can be obtained in special groups and from specialists in the form of counseling. The main thing is that a person should not be left alone with his illness. Anadolu doctors are well aware of the importance of psychological support, so the patient can always count on a caring and attentive attitude.
The material was prepared in agreement with Anadolu physician and medical oncologist Yeshim Yildirim.
Clinical manifestations of bone metastasis
Contrary to popular myths, skeletal metastasis often occurs without significant pain and even without symptoms at all. Osteoblastic lesions are less often accompanied by pain than osteolytic lesions.
Dangerous manifestations of metastatic bone lesions:
- hypercalcemia - a significant increase in calcium concentration due to the destruction of the bone matrix leads to a severe condition that requires correction of metabolism, essentially resuscitation measures;
- fracture - destruction of half the diameter of a bone or vertebra is sufficient to cause it; every eleventh patient with a pathological fracture requires urgent surgical care;
- syndrome of compression or compression of the spinal cord by fragments of a broken thoracic or lumbar vertebra, complicated by severe neurological disorders below the damage zone;
- impairment of motor activity up to paralysis is possible when the spinal cord is compressed in the cervical region by an osteoblastic lesion or damaged by fragments during lytic destruction.
Complications of bone metastasis have a fatal impact on the patient’s condition and actively interfere with adequate treatment, which can shorten life expectancy with an absolute lack of quality.
Stages of multiple myeloma
Stage 1 - characterized by mild anemia, calcium remains within normal values, M-protein is low, the number of bone lesions is no more than 5.
Stage 2. Moderate anemia (hemoglobin within 85-100 g/l), there is an increase in calcium (up to 3 mmol/l) and M-protein. There is also an increase in the number of osteolysis foci. For the second stage, their number should not exceed 20.
Stage 3 multiple myeloma is diagnosed when at least 1 of the following symptoms is detected:
- Hemoglobin is below 85 g/l, which corresponds to severe anemia.
- Exceeding the calcium value by more than 3 mmol/l.
- M-protein level is more than 70 g/l.
- The number of bone lesions is more than 30.
Why does pain occur?
Pain is caused by three reasons:
- destruction of the richly innervated periosteum by a cancerous conglomerate;
- irritation of pain receptors in the periosteum by biologically active waste products of cancer cells;
- involvement of muscle nerve endings in the metastatic node.
Unbearable pain is not always associated with skeletal metastasis; as a rule, this is a consequence of the high aggressiveness of tumor cells in the terminal stage of the process, when the concentration of biologically active substances in the blood is enormous - cytokines, which literally “burn” the nerve endings of even tissues not affected by the tumor. With a high degree of malignancy of the primary tumor, pain is observed more often and more intensely. The most obvious example is widespread and persistent pain in completely intact bones due to lung adenocarcinoma; surgery to remove the affected lung completely cures the pain.
How are bone metastases detected?
Diagnosis of skeletal injuries is not complicated, but high-tech, they begin with an isotope examination - osteoscintigraphy, which reveals minimal cancerous tumors. The “hot spots” illuminated by the isotope are then subjected to radiography or, better yet, computed tomography (CT). PET is the “queen” of evidence; unfortunately, it is an expensive study, so it is not very suitable for monitoring the effectiveness of therapy.
Bone resorption markers are not suitable for identifying foci in the skeleton; they have not been actively used in practical oncology.
Blood tests allow one to suspect a tumor lesion in the bone marrow, which often accompanies metastasis to the sternum.
Diagnosis of bone metastases
Various imaging methods are used to detect metastases:
- magnetic resonance, computer or positron emission tomography;
- radiography;
- radionuclide scintigraphy.
From laboratory tests, a blood test is important. There may be an increase in the concentration of calcium and alkaline phosphatase. Finally, a needle biopsy is used. The material taken is sent for histological examination, which establishes the final diagnosis.
Treatment of skeletal lesions
Is it possible to cure bone metastases? Definitely, treatment can prolong life if you feel well. On the one hand, skeletal lesions are a manifestation of the spread of cancer throughout the body, on the other hand, they are a sign of a relatively favorable prognosis of the disease in the absence of tumors in other tissues and visceral (internal) organs, which gives years of life when the process stabilizes.
At the stage of bone metastasis, the question of radical treatment is no longer raised, but surgery is not excluded if the histological structure is favorable and the lesion is solitary - the only bone lesion. So, in case of lung or kidney cancer with metastasis to the humerus or thigh, a one-stage intervention can be performed with removal of the diseased organ and bone resection with prosthetics, but after several months of chemotherapy.
Chemotherapy is the main method of treating bone lesions, the drug regimen is determined by the primary tumor. For breast and prostate cancer, hormonal therapy shows good results.
Supplementing chemotherapy with local radiation can improve the overall outcome of therapy, relieve pain and reduce the likelihood of fracture. So, if the cervical vertebrae are affected, radiation therapy is mandatory already at the first stage.
The operation is necessary if there is a threat of compression (compression) of the spinal cord by a broken vertebra; as a rule, the affected part of the vertebra is removed - laminectomy. With long-term stabilization (more than six months) as a result of chemotherapy, the question of removing the affected bone of the limb and replacing it with a prosthesis can be raised, if there are no other manifestations of cancer.
Why are bisphosphonates needed?
The use of bisphosphonates for skeletal metastases has become the standard of adequate therapy.
Human bones are constantly renewed: osteoclasts destroy, and osteoblasts build up tissue; normally, the processes are balanced; in the presence of a malignant tumor, osteoclasts become overactive. Bisphosphonates are similar in structure to the bone matrix, therefore, after introduction into the body, they are sent to the bones, where they have a detrimental effect on osteoclasts activated by cancer products, while simultaneously relieving pain and protecting against fractures.
Bisphosphonates can be treated for about two years; if sensitivity to them is lost, the monoclonal body denosumab plays a similar role. Demosumab and bisphosphonates are classified as osteomodifying agents (OMAs).
To prescribe OMA, it is not enough to identify “hot” lesions during osteoscintigraphy; they are used in cases of tumor lesions proven by radiological methods.
Chemotherapy and OMA are the main treatments for skeletal lesions, but they are not the only ones. Treatment of bone metastases should be comprehensive; only a combination of radiation and drugs, with the correction of metabolism and the addition of palliative surgery, can relieve pain and return the patient to an active life.
When and what is needed and possible in each specific clinical case of cancer, the specialists of our clinic know. Find out more, call:
Book a consultation 24 hours a day
+7+7+78
| More information about treatment at Euroonco: | |
| Oncologist consultation | from 5,100 rub. |
| Emergency oncology care | from 12,100 rub. |
| Chemotherapy appointment | RUB 6,900 |
| Palliative care in Moscow | from 44,300 rubles per day |
Bibliography:
- Aliev M.D., Teplyakov V.V., Kallistov V.E., Valiev A.K., Trapeznikov N.N. / Modern approaches to surgical treatment of metastases of malignant tumors in the bones // Practical Oncology, No. 1(5) (March), 2001
- Belozerova M. S., Kochetova T. Yu., Krylov V. V. Practical recommendations for radionuclide therapy for bone metastases // Malignant tumors, No. 4, 2016, Special issue 2.
- Kondratyev V.B., Martynyuk V.V., Lee L.A. / Bone metastases: complicated forms, hypercalcemia, spinal cord compression syndrome, drug treatment // Practical Oncology, No. 2 (June), 2000
- Manzyuk L.V., Bagrova S.G., Kopp M.V., Kutukova S.I., Semiglazova T.Yu./ The use of osteomodifying agents for the prevention and treatment of bone tissue pathology in malignant neoplasms // Malignant tumors: Practical recommendations RUSSCO #3s2, 2022 (vol. 7)
- Snegova A. V., Bagrova S. G., Bolotina L. V., Vladimirova L. Yu., Gorbunova V. A., Kogonia L. M./ Prevention and treatment of bone tissue pathology with osteomodifying agents (OMA) in malignant neoplasms // Malignant tumors, No. 4, 2016, Special issue 2.
Features of diagnosis and treatment of diseases accompanied by resorption of bone structures
Peculiarities of diagnostics and treatment of diseases, accompanied by resorption of bone structures
I. K. Lutskaya , MD, Professor, Head of the Department of Therapeutic Dentistry of BelMAPO
A. O. Korzhev , dental surgeon, 8th City Clinical Dental Clinic, Minsk
A. A. Esman Chief Physician of the 8th City Clinical Dental Clinic in Minsk
The main volume of work of a dental surgeon during outpatient visits is performed by tooth extraction operations. The next most common procedure is periodontal surgery and cystotomy. Currently, the indications for the installation of intraosseous implants with subsequent prosthetics are expanding. At the same time, one of the serious problems faced by specialists is bone tissue resorption due to the inflammatory process, complications of previously performed dental treatment or after surgery [3, 7]. As an example, we can consider the primary formation of a cystic cavity in the root area or secondary resorption of the alveolar bone after tooth extraction.
One of the most common methods for diagnosing most diseases of the human teeth and jaws is an x-ray examination of the patient. Achievements in dentistry in the last decade were marked not only by the emergence of new methods of treatment and prevention, but also by the development of X-ray technology and the development of new radiography techniques [6]. This naturally caused an increase in the frequency of use and expansion of the range of radiological studies of the dental system.
In case of complicated caries, X-ray examinations are necessary to determine the nature and extent of damage to the periapical tissues, and an accurate diagnosis of periodontal tissue diseases is carried out. In case of traumatic injuries, tumors, tumor-like diseases, cysts, deformations and systemic lesions of the skull bones, X-ray examination is the leading method of primary diagnosis and assessment of the effectiveness of treatment measures, and timely detection of complications [3, 4].
On radiographs, the bones of the facial skeleton and jaws have a characteristic structure, the so-called bone pattern, which reflects the features of function and anatomical structure. Pathological processes lead to changes in the bone pattern, which allows the dentist to diagnose various diseases.
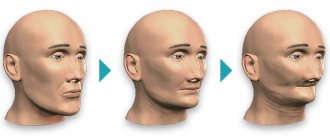
Thus, osteoporosis is a dystrophic process, which is based on the reduction and replacement of bone tissue with osteoid substance, adipose tissue, and blood. With osteoporosis, the number of bone beams per unit volume of bone decreases, they become thinner, and the medullary spaces expand.
Based on the nature of the shadows on the radiograph, osteoporosis is divided into focal and diffuse. The first is represented by individual, 1 to 5 mm in size, foci of rarefaction of bone tissue with clear or unclear contours and precedes sequestration in bone osteomyelitis. Diffuse osteoporosis is characterized by a uniform loss of bone tissue, the cortical layer of the bone is thinned, sometimes disintegrated, and the medullary spaces are expanded. This type of osteoporosis occurs after tooth loss.
Destruction is the destruction of bone and its replacement with pathological tissue (pus, granulations, etc.). On an x-ray, the focus of destruction has a lower density compared to nearby unchanged areas.
Destructive changes in bone substance are most often observed with inflammatory and tumor lesions of bones. Destruction occurs, on the one hand, through the resorption of bone beams and trabeculae as a result of the direct impact of the pathological process (purulent inflammation, decay, necrosis, germination with tumor tissue, etc.), and on the other hand, through a reflex neurohumoral pathway. In this case, the bone marrow spaces merge and increase in volume.
Resorption is the resorption of bone structures or dentin, including the tips of the roots, which can be physiological in nature (roots of temporary teeth) or be a consequence of a pathological process. If a radiograph reveals a destructive focus with better or worse defined contours in the area of the root apex, this may be due to various stages of granulating, granulomatous and fibrous periodontitis. The X-ray image of a cyst in the process of formation may initially not differ from other stages of development of chronic periodontitis. Further formation of the cyst leads to an increase in size. An X-ray examination reveals a spherical area of clearing in the area of the apex of the tooth root. The boundaries of this cavity are smooth and clearly defined. Often a thin sclerotic rim forms around the cavity.
In severe periodontitis, radiographs reveal significant areas of clearing, characterizing a loss of bone tissue of more than 1/2 the length of the root in many teeth, sometimes complete resorption of the interdental septum and pronounced changes in the area of root furcation. Vertical resorption leads to the formation of deep bone pockets along the dentition [3, 6].
Among surgical treatment methods, a special place is occupied by reconstructive surgery using osteoreplacement materials, which promote the restoration of bone tissue and activate the processes of tissue regeneration in a living organism [1, 2, 5].
Reparative regeneration of bone tissue as a biological process is genetically predisposed; the process cannot be accelerated [5]. However, there are regeneration factors that can have an optimizing effect, so the role of agents that have a positive effect on osteogenesis is increasing. The term “directed bone regeneration”, proposed by D. Buser, defines the principle of creating favorable conditions for the development of bone cells between the bone defect and the surrounding soft tissues to prevent epithelium from penetrating into the area of osteoreparation. According to the literature, when ensuring the most favorable conditions, means that promote the formation of bone tissue and its calcification deserve special attention. For this purpose, barrier membranes are used in combination with osteoplastic material, which should ensure the implementation of the abilities that bone tissue initially possesses [5, 7].
Calcium phosphate compounds (hydroxyapatite) are of great interest as a material that is closest in composition to bone tissue, the mineral component and hard tissues of the tooth.
Currently, the production of drugs based on hydroxyapatite has been mastered by many, “Kolapol”, “Hydroxyapol” and “Kollapan”), in the Republic of Belarus (“KAFAM”, hydroxyapatite gel). The materials are used with various types of antibiotics and antiseptics, do not require special tools and equipment, and are manufactured in various forms (blocks, plates, granules, powders, suspensions). All types of hydroxyapatite are used in the surgical treatment of various dental diseases.
A product based on nanocrystalline hydroxyapatite (calcium phosphate) is intended for implantation into bone tissue in order to activate osteoreparative processes; it has an increased ability to transform in biological media into calcium and phosphate ions, which ensures better absorption of these ions directly in the “zone of interest” - the bone wound ( zone between fragments in fractures, bone defect, sequestral cavity, etc.).
Calcium reduces the permeability of cell membranes and the vascular wall, preventing the development of inflammatory reactions. Calcium ions are involved in the transmission of nerve impulses, blood clotting and other physiological processes.
Hydroxyapatite helps optimize the healing of bone wounds, the formation of functionally and structurally complete osteoregenerate according to the type of primary healing of a bone wound. The use of the drug can reduce the duration of the pain period in patients after surgery and promotes the rapid elimination of soft tissue swelling in this area. Hydroxyapatite is characterized by low solubility in biological media and a slow entry of calcium ions into the interstitial environment and blood.
Application in dentistry:
- in case of an open (complicated) fracture of the jaw bone - directly into the bone wound in a volume adequate to the interfragmental space;
- in case of formation of bone defects of the jaw bones after removal of benign neoplasms - directly into the bone wound in a volume adequate to the bone defect;
- in case of formation of vertical bone defects in the area of the alveolus of the jaw bone during radical operations on periodontal tissues - after removing pathological tissues from the bone pocket, treating the bone pocket before suturing the surgical wound;
- in case of chronic post-traumatic osteomyelitis of the jaws after removal of sequestra under conditions of immobilization - directly into the sequestral cavity (defect cavity) in a volume adequate to the bone defect.
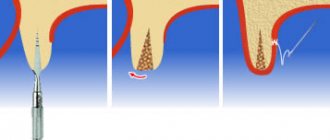
- filling bone defects after surgery for tooth extraction, cystectomy, resection of the root apex (Fig. 1, 2).
Rice. 1. Radicular cyst of the upper jaw. CBCT examination.
Rice. 2. X-ray of a molar after resection of the root apex.
An example of drugs based on hydroxyapatite is “Kollapan”, a drug used to restore bone tissue, prevent and treat purulent complications. Consists of hydroxyapatite and collagen. It is completely replaced by bone tissue and retains antimicrobial activity in the wound for up to 20 days, during which the antibiotic is uniformly released in the bone cavity [2].
Available in the form of granules, gel, plates: different types of material are due to the convenience of filling bone defects of various shapes and locations.
The choice of the type of drug depends on the causative agent of the disease. The presence of antimicrobial agents of various spectrums of action in the material allows you to purposefully select the type of “Kollapan” that corresponds to the causative agent of the disease, which significantly increases the effectiveness of treatment.
“Kollapan” does not cause rejection, suppuration, or allergic reactions. A contraindication for use is individual intolerance to the antibiotic included in the drug.
Depending on the shape of the defect being filled, both isolated and combined use of granules, plates, and gel is possible. The plates are easily cut with scissors or a scalpel. The gel is introduced if it is necessary to create more complete contact of granules and plates with bone tissue. Used for periodontitis, tooth extraction, root apex resection, dental implantation, peri-implantitis, soft sinus lifting, chronic periodontitis, perforation of the bifurcation zone, alveolitis.
Clinical case No. 1
A tooth extraction operation with preliminary excision of the epithelial edge of the gum.
Using an ophthalmic scalpel, incisions were made along the marginal gum from the vestibular and oral surfaces so that, from the side of the bone pockets, the incision passed below the marginal part of the gum by 1-2 mm; From the side of the preserved alveolar bone, the incision was made as close as possible to the gum edge.
Deep into the tissue, the incision was made at an angle from the edge of the gum to the level of the bottom of the periodontal pocket and extended all the way to the cementum of the root, which made it possible to excise the epithelium along the edge of the gum, pathological granulations in the pocket and subgingival dental plaque.
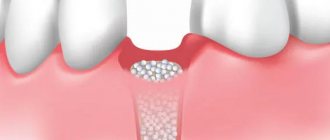
Hemostasis was carried out, and the removal of mobile teeth was immediately performed. When applying forceps, tissues excised from the oral and lingual sides of the tooth were grasped (Fig. 3, 4). The bone defect was filled with a preparation containing an osteoplastic base and meeting the basic requirements: chemically stable in the physiological environment of the body, resistant to oxidation, does not allow the accumulation of harmful interaction products, and does not cause galvanoelectric phenomena. These requirements are largely satisfied by preparations containing hydroxyapatite [Ca10(PO4)6(OH)2] with a Ca/P ratio of 1.67, which is an analogue of the inorganic component of the bone and dental tissues of the body.
Rice. 3. The socket of the extracted tooth is filled with osteoplastic material.
Rice. 4. Wound surface after removal of a group of teeth.
The wound was sutured in such a way that a more mobile flap covered the tooth socket. After regeneration was completed, implants were installed in the jawbone (Fig. 5, 6).
Rice. 5. Intraosseous implants.
Rice. 6. Normal bone structure in the implant area. X-ray.
Clinical case No. 2
Organ-saving surgery with cementotomy for localized periodontitis.
The corresponding area of the jaw was anesthetized, and an incision was made in the interdental space parallel to the base of the papilla between the proximal sides of the teeth. The dissection of the interdental soft tissues was carried out in a section of the dentition that exceeded the area of the intended intervention by 1-2 teeth on each side, and was supplemented with an incision that made it possible to deepen the vestibule of the oral cavity. Then, alternately on each side, the flaps were peeled off on both sides of the alveolar process and retracted to a distance allowing free manipulation in the surgical field.
Removal of granulations and vegetation of the epithelium with a scalpel began from the apical parts of the surface of the flaps. Next, we began to remove granulations adjacent to the tooth and alveolar bone using instruments for removing tartar and small curettage spoons. Sharp bony protrusions on the alveolar process were ground off with a diamond head.
Treatment of the roots of non-pulp teeth was carried out by scraping with sharp instruments (excavator, sharp hooks of various shapes) surface deposits of tartar along with granulations and necrotic tissues on the surface of the cement. The roots of pulpless teeth were subjected to cementotomy with an elongated bur with a blunted and polished end part, holding it at different angles relative to the surface of the tooth root.
The wound was thoroughly washed with antiseptic solutions. The bone pockets were filled with a preparation of hydroxyapatite with collagen. The sutures were made from catgut with an extended resorption period. Recommendations for wound care are given. Postoperative monitoring is carried out.
Clinical case No. 3
Patient Sh., 34 years old. Diagnosis: radicular cyst of the upper jaw on the left in the area of teeth 22 and 23 (Fig. 7). Teeth extraction with cystectomy was performed under local anesthesia (Fig. 8). The cavity walls were carefully processed and hemostasis was performed (Fig. 9). The cyst cavity is loosely filled with a preparation based on hydroxyapatite. The wound was sutured with catgut, and instructions were made to perform it at home. The postoperative period proceeds without complications.
Rice. 7. CBCT image. Cyst in the upper jaw area on the left.
Rice. 8. Teeth removed. A cystectomy was performed.
Rice. 9. Hemostasis after cystectomy.
Conclusion
Inflammatory processes in the maxillofacial area are often accompanied by destruction of bone tissue, expressed by the resorption of bone beams and their replacement with products of pathological decay or newly formed granulation tissue. Diagnosis of such changes is carried out (or clarified) on the basis of an x-ray examination of the bones of the facial skull. The x-ray image reveals areas of clearing that correspond to a certain clinical picture. The effectiveness of treatment of diseases manifested by resorption of bone structures increases significantly with the local use of drugs that have an osteotropic effect, primarily based on hydroxyapatite.
- Lutskaya Irina Konstantinovna, Doctor of Medicine, Professor, Head of the Department of Therapeutic Dentistry BelMAPO, Belarus, Minsk Doctor of Medicine, Professor, Head of the Department of Therapeutic Dentistry BelMAPO, Belarus, Minsk
Lutskaya IK, dms, professor, Head of the Department of Therapeutic Dentistry Belarusian Medical Academy of Postgraduate Education, Belarus, Minsk
Korzhev Alexey Olegovich, dental surgeon, 8th City Clinical Dental Clinic, Minsk, Belarus, Minsk
Korzhev AO, 8th city clinical dental clinic, Belarus, Minsk
Esman Andrey Alekseevich, chief physician, 8th City Clinical Dental Clinic, Minsk, Belarus, Minsk
Esman AA, 8th city clinical dental clinic, Belarus, Minsk
UDC 616.716-003.95-07-08
220040, Minsk, st. Surganova, 70—71
Tel. +375 29 631-65-28
e-mail:
Annotation. The article provides information characterizing the x-ray picture of diseases accompanied by destruction of the alveolar bone. Features of the pathological process are manifested by specific changes in the structure, which are reflected on the x-ray and allow you to clarify the clinical diagnosis. Surgical treatment of identified diseases aims to exclude etiotropic factors. The efficiency of regeneration of bone structures can be significantly increased by filling bone defects with an osteotroplastic preparation based on calcium hydroxyapatite.
Annotation. The article provides information characterizing x-ray picture of the diseases accompanied by destruction of the alveolar bone. Features of a pathological process manifested specific changes in the structure, which is reflected in the x-ray and allows us to Refine the clinical diagnosis. Surgical treatment of identified diseases aims to the exclusion of causal factors. The efficiency of regeneration of bone structures can be significantly increased by filling the bone defects osteuropaeischen a drug on the basis of hydroksiapatit calcium.
Key words: X-ray diagnostics; destruction of alveolar bone; osteoplastic material.
Key words: x-ray diagnostics; destruction of the alveolar bone; osteoplastic material.
Literature
1. Bezrukov V. M., Grigoryan A. S. Hydroxysapatite as a substrate for bone grafting: Theoretical and practical aspects of the problem // Dentistry. - 1996. - No. 5. - P. 7-12.
2. Kozlov V. S., Tumanova A. S., Trukhanov E. F. Application of collapan in the surgical treatment of periodontitis // www. medznate. ru/docs/index780. html, 2013.
3. Kulakov A. A. Clinical and laboratory examination in preoperative preparation for intraosseous dental implantation in patients with osteoporosis / A. A. Kulakov, M. S. Sedova, M. V. Gunko // Materials of the XIII International Conference of Maxillofacial Surgeons and dentists “New technologies in dentistry.” - St. Petersburg, 2008. - pp. 125-126.
4. Lutskaya I.K. Implantation of a single tooth in the frontal part of the upper jaw / I.K. Lutskaya, T.L. Shevela // Dental implantology and surgery. - 2014. - No. 3. - P. 63-65.
5. Paraskevich V. L. Dental implantology. Fundamentals of theory and practice / V. L. Paraskevich. - Minsk: Unipress, 2002. - 368 p.
6. Ruzylo-Kalinovska I., Ruzylo T.K. Three-dimensional tomography in dental practice. Translation from Polish - Lvov: GalDent, 2012. - 584 p.
7. Wortche R. An alternative method for sinus floor elevation //EDI Jornal. - 2013. - No. 1. - Vol. 9. - P. 80-85.