Dear friends, today’s topic of conversation, in fact, should be a prologue to all our publications devoted to bone tissue augmentation before implantation. We have already written about sinus lifting, guided bone regeneration, bone blocks and osteotomy, we talked about when and why this should be done, but we left out of the scope of publications perhaps the most interesting question:
Why does bone atrophy occur in the first place?
What is atrophy? What are its reasons? Why does it develop rapidly in some people, literally in a month or two:
and someone walks without teeth for years - and there is no loss of bone tissue?
Is it possible to predict the degree of bone tissue atrophy even before tooth extraction and is there a way to prevent it?
The answers to these questions are important, if only because without understanding the biological mechanisms of atrophy, it is impossible to determine the need for the same preventive augmentation of the socket of an extracted tooth, it is impossible to CORRECTLY choose the method of bone tissue augmentation for a specific clinical case and, most importantly, it is impossible to give a clear and long-term prognosis as a result of osteoplasty.
I will say even more - in many ways, almost all unsuccessful outcomes of bone tissue augmentation are explained, among other things, by a lack of understanding of the processes occurring in the jawbone after tooth extraction. That's why this knowledge is important.
So,
How to understand that tissue atrophy is occurring?
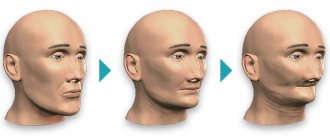
- the patient’s face “sinks,” the skin in the jaw area sags, nasolabial wrinkles become more pronounced;
- the gum contour recedes;
- displacement of dental units occurs;
- neighboring crowns become more mobile.
In dental practice, there are four main types of bone atrophy: minor, moderate, pronounced, and severe atrophy of bone tissue. So, with minor atrophy, implantologists can still introduce a titanium root into the jaw without restoring the bone, but with a rough form, they cannot do without restoring the volume.
What in practice?
Knowledge of the principles and patterns of the atrophic process, on the one hand, breaks the pattern and our understanding of osteoplasty, but on the other hand, it provides a very reliable prognostic tool. Using it, you can not only predict the dynamics of changes in bone tissue volumes after removal and implantation, but also clearly explain how different methods of bone tissue augmentation work in different clinical conditions.
What do we know about the patient?
The biotype of bone tissue is something that we can determine from a computed tomogram even before tooth extraction.
How to use it?
Knowing the relationship between the biotype and atrophy, it is possible to more or less reliably determine the indications, for example, for preventive preservation of the socket, including immediate implantation.
And, in theory, such a clear analysis and prognosis of atrophy in relation to a specific clinical case should replace the well-established principle in modern implantology “Everyone does it!” or “That’s how we were taught!”
In addition, we can predict the degree of atrophy and determine whether bone augmentation will be required during delayed implantation even before the teeth are extracted.
and, if necessary, what is the best method to do this?
Or, for example, can we explain why in some cases the transplanted bone block goes away, but in others it does not?
The main causes of bone tissue atrophy in a patient
- missing one or more teeth;
- wearing prosthetic systems that apply pressure;
- jaw deformation;
- cystic formations on the roots - pathological cyst cells grow and gradually replace tissue;
- anatomical feature of the jaw structure;
- elderly age;
- diseases (diabetes mellitus, osteoporosis, gum disease, inflammatory processes in the oral cavity);
- incorrect prosthetics or implantation.
When chewing food, pressure is applied to the bone, and it, one way or another, dissolves. If the pressure itself cannot be excluded, then there is always the possibility of returning the lost bone with the subsequent installation of a dental prosthesis or bridge.
How to protect bone from atrophy: treatment of periodontitis and periodontal disease
Over decades of dental research and practice, many methods have been found to treat gums, dental ligaments and jaw bones with periodontitis and periodontal disease. In recent years, developments in microbiology and advances in the field of periodontics and biomaterials have brought the latest effective developments and drugs. Some time ago, periodontitis was considered an irreversible disease, and even at the initial stage it was necessary to take into account the fact that with all methods of treatment and prevention, a temporary result was achieved, albeit for a long time - for several years. Today, the first two stages of the disease can be successfully treated in adults and children, as well as restoration of bone and gum levels thanks to advanced methods and drugs.
To achieve results in restoring oral health, an integrated approach is essential. To treat this disease, you cannot choose just one effective and proven method, since you need to influence the problem from all sides: it is important to eliminate the cause, stop the inflammatory process and subsequently restore the periodontium and ligamentous apparatus.
However, at the third chronic stage of the disease, considerable treatment efforts are, as a rule, insufficient to completely eliminate the disease, and the only solution remains to remove the remaining affected teeth as the source of inflammation and the focus of the disease.
Periodontal disease has a different clinical picture, and the treatment of this disease is based on other methods. Let's look at them in more detail later in the article.
What happens if bone tissue atrophy is not stopped?
The quality of life, appearance, and feelings of a person are more influenced not by the resorption itself, but by the causes of the problem. For example, if the bone in the jaw dissolves due to the absence of one or more teeth, the process of chewing food is disrupted, an imperfect food bolus is formed, resulting in problems in the functioning of the gastrointestinal tract. Diction is also impaired, facial asymmetry occurs, and psychological discomfort develops due to the lack of teeth. The teeth begin to shift in the direction where one or a group of teeth is missing.
It is important!
The longer the jaw is missing teeth, the more volume of jawbone is lost, and the more of it will need to be built up in the future during implantation. Timely replacement of a lost tooth with an implant that serves as a support for the prosthesis will prevent atrophy and will also help save your budget (you will not need to perform an expensive operation to restore the bone).
What is the diagnosis of diseases based on?
Accurate determination of the disease and its stage will allow timely and appropriate treatment to begin. But, unfortunately, many clinics limit themselves to x-rays and visual assessment of the oral cavity, which does not always allow a detailed understanding of the problem. But, in addition to the symptoms, for successful treatment it is necessary to determine the cause of the disease and evaluate what was the impetus for its development. To do this, a differential diagnosis is carried out, consisting of several successive stages:
- the doctor examines the oral cavity, noting signs of disease. Using instruments, measurements are made of the depth of periodontal pockets, the amount of deposits,
- an anamnesis is collected about the time of the disease, its manifestations, the patient’s feelings, as well as the quality of oral hygiene,
- to assess the condition of the bone and get details of the problem, a computed tomography (CT) scan is performed,
- Bacterial plaque and stone from periodontal pockets are taken for examination to determine the composition of the microflora and its resistance or sensitivity to drugs,
- The diagnosis is completed with blood tests (general and sugar); additional blood tests for hormones may be needed.
Diagnosis of periodontal disease at the initial stage of the disease is difficult due to the non-obviousness of the symptoms and is also not limited to one visual examination. However, even at the first stage, radiography can detect bone atrophy. The diagnosis is made on the basis of an orthopantomogram and visual and instrumental examinations. For greater accuracy, microscopic examination of the gums is used to assess the degree of disruption of microcirculation in them.
How to solve the problem of bone tissue atrophy?
- Perform a sinus lift - a procedure for increasing bone in the upper jaw. In this case, the maxillary sinus may rise or shift to free up jaw space for new bone.
- Bone grafting is an operation in which the lack of bone is filled with artificial synthetic materials. The operation is often associated with the risk of rejection of the artificial material.
- Bone grafting is a technique of transplanting your own bone blocks from one area of the jaw to another. As a rule, bone material is taken from the area of the “eights” (wisdom teeth) and placed in place of the bone deficiency. Due to the natural nature of the material, the risk of rejection is low.
To prevent jawbone atrophy, it is important to provide comprehensive prevention. So, if a tooth falls out or is removed, replace it in a timely manner with a new titanium root, which serves as a support for the crown.
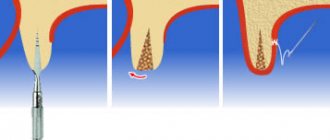
Also, for a patient whose tooth has been extracted, a special membrane is placed in place of the gap to prevent atrophy. If necessary, a small amount of tissue is added to the internal compartment to replenish the lost volume and ensure the stability of the implant being introduced.
Atrophy is...
According to medical textbooks, atrophy means a lifetime decrease in the volume of cells, tissues and organs , accompanied by a decrease or cessation of their functions. In relation to dentistry and implantology, we can define atrophy as a change in the linear dimensions and volume of the alveolar ridge after the removal of a tooth or teeth.
Atrophy can be reversible or irreversible.
Reversible atrophy is usually caused by the cessation of functioning of an organ or tissue. So, if you do not use your hand for a long time (for example, after a fracture), the muscles of the hand will atrophy.
However, once the function returns, they quickly return to normal.
Irreversible atrophy has a number of causes, of which dysfunction is just one of them. Thus, atrophy of the heart muscle is accompanied by its sclerosis, the replacement of the muscle fibers themselves with connective tissue. The result is chronic heart failure, for which only symptomatic treatment exists so far.
The reversibility of brain atrophy in some people remains controversial.
, atrophy of the alveolar ridge after tooth extraction is classified as dysfunctional, i.e., associated with cessation of function. It would seem a very simple mechanism - “no teeth, no load on bone tissue - presto, atrophy!”
But, in reality, not everything is so simple.
First, dysfunctional atrophy is usually reversible (see muscle example).
Secondly, and this is the question that concerns me first, why do different people have different rates and levels of bone loss?
Why do some patients develop atrophic pesdets within a few weeks after tooth extraction, while others live without teeth for many years, maintaining almost the original volume of bone tissue? Where does this injustice come from?
And so, in order to understand this issue, we need to remember what bone tissue is in general.
Why doesn’t prosthetics solve the problem of bone tissue atrophy?
Installing a removable denture or “bridge” does not solve the issue of missing bone, since the load in this case is on the gum tissue and on the remaining healthy teeth. Consequently, the resorption process is not stopped, the gums begin to “sag” along with the bone, the fixation of the prosthesis is disrupted, and a gap is formed under it. Food debris accumulates in this gap, which can lead to inflammation. Unlike conventional prosthetics, dental implantation allows you to compensate for the deficiency of bone tissue, and most importantly, restores the integrity of the dentition.
Why does the jawbone shrink?
When a person has all the teeth in the mouth, the chewing load is evenly distributed throughout the entire alveolar ridge (that is, pressure is received by the gums, ligamentous apparatus and directly the bone in which the tooth roots are located). This is a natural process through which bone cells receive nutrition and metabolic processes occur in them. And thus the bone maintains its volume.
In cases where a tooth is removed, the bone tissue no longer receives load. When chewing, all the pressure is redistributed between the remaining teeth. Therefore, the nutrition of tissue cells is disrupted, which leads to its resorption. And gradually atrophy of the jaw bone tissue occurs.
Bone loss is also affected by other dental problems, such as inflammatory processes (cysts, granulomas, periodontitis and periodontitis). In these cases, tissue resorption occurs as bone cells are replaced by others.
There are other reasons that lead to bone thinning:
- individual structural features of the maxillofacial apparatus,
- genetic predisposition,
- getting jaw injuries,
- age-related changes in humans and natural aging of all organs,
- prosthetics that rely only on the gums (removable) or on living teeth (bridge), due to which the bone again does not receive the necessary load,
- inflammation of the mucous membranes, periodontal tissue diseases.
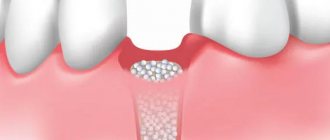
Does all the bone atrophy?
Our jawbone consists of several sections: the central one is the spongy layer. It contains tooth roots. This section is the most porous, since it is in it that a large number of capillaries are concentrated, which means that it is the spongy section that undergoes atrophy first. Below it is the basal layer - it is already stronger, since it consists of bone partitions and there are several times fewer capillaries in it. Both layers are covered by a shell or cortical plate - it, like the basal layer, is very dense and does not undergo atrophy.
Further, already behind the basal section, on the upper jaw there is a zygomatic bone, as well as buttresses - these are lines of force that evenly distribute pressure on the jaw between all the bone tissues of the skull.
On the upper jaw, the sinuses are located close to the jawbone. They have a rather thin shell, which can be easily damaged if implants are too long1. There are no sinuses on the lower jaw - the chin and jaw bone go under the alveolar process. They are very durable, so tissue atrophy below is less common, and implantation is easier.
Implantation options for bone atrophy
- Dental implantation with delayed loading is a technique in which bone material is first restored, and only then an artificial implant is introduced - a support for the subsequent prosthetic structure.
- Dental implantation with immediate loading is a procedure in which the implant is screwed into the basal (deep) parts of the jawbone, and not into the alveolar zone, as with classic implantation with build-up. In this case, the bone is instantly “loaded”, all living cell processes are preserved in it, and healing is accelerated.
How to install implants in conditions of bone deficiency
Classic dental implantation in case of insufficient bone tissue is preceded by bone augmentation surgery or sinus lift. Before implantation, a period of engraftment of the grafting material (4-6 months) is waited. During this period, the patient is fixed with a removable prosthesis.
If I and II degrees of loss are diagnosed, implantation and replanting of cells can be organized simultaneously. It is possible to exclude bone grafting if all or almost all teeth in a row are missing - artificial roots are implanted using a one-stage protocol at an angle (into the deep bone layers).
Nesterenko Alexey Pavlovich Implant surgeon, doctor of the highest category
Can implantation stop cell loss?
In addition to solving the problem of aesthetics and restoring the functionality of the dentition, installing implants helps prevent resorption. Due to the implants, the load on the jaw is distributed evenly, internal metabolic processes in the cells are activated, cellular nutrition is established - the atrophy process stops.
How much does surgery to restore bone atrophy cost?
The average price of bone grafting in Moscow is from 20,000 rubles. The cost of a sinus lift ranges from 22 thousand to 80 thousand rubles, respectively.
This amount includes expenses for:
- osteoplastic materials;
- bone membrane;
- anesthesia;
- X-ray images;
- the work of a surgeon, etc.
Dentistry "32 Dent" specializes in performing bone grafting operations to solve the problem of bone tissue resorption in patients and the restoration of living cells. Also, specialists will restore the dentition by performing subsequent prosthetics.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Sources:
- Personal experience as an orthopedic dentist;
- Yamurkova, N. F. Optimization of surgical treatment for severe atrophy of the alveolar process of the upper jaw and the alveolar part of the lower jaw before dental implantation: abstract. dis. ...Dr. medical sciences: 01/14/14 / Yamurkova Nina Fedorovna. — Nizhny Novgorod, 2015;
- Durnovo, E.A. Method of preserving alveolar tissue in the aesthetically significant zone / E.A. Durnovo, A.V. Kazakov, S.E. Sakharova, N.A. Yanova // Russian Bulletin of Dental Implantology. – 2013;
- Amkhadova, M.A. Surgical tactics when using the implantation method in patients with dentition defects and significant jaw atrophy: dis. ...Dr. med. Sciences: 14.00.21 / Amkhadova Malkan Abdrashidovna. – M., 2005;
- Artyushkevich, A.S. Periodontal diseases: a practical guide / A.S. Artyushkevich. – M.: Med. lit., 2006;
- Bedretdinov, R. M. Clinical and morphological assessment of various osteoplastic operations before dental implantation (experimental clinical study): abstract. dis. Ph.D. medical sciences: 01/14/14 / Bedretdinov Rinat Mansurovich. – M., 2016;
- Belchenko, V.A. Craniofacial surgery: a guide for doctors / V.A. Belchenko. – M.: Medical Information Agency., 2006;
- Andersson, L. Oral and Maxillofacial surgery / L. Andersson, K. Kahnberg, M. Pogrel. – WILEY-BLACKWELL Publishing Ltd. – 2010;
- Alfaro, F.H. Bone grafting in Oral Implantology. Techniques and Clinical Applications / FH Alfaro. – Quintessence Publishing Co. Ltd. – 2006.
The appearance of wrinkles, facial aging
Bone tissue atrophy is unpleasant not only because if it occurs, it is sometimes problematic to install implants. It also leads to the fact that our appearance is disrupted - many signs of aging appear very quickly: the lips sink inside the mouth, wrinkles appear around the mouth, on the neck, on the cheeks. In addition, a person begins to lisp, stops eating normally (after all, there is simply nothing to chew food with), smile and communicate. The chin visually becomes smaller, the lips become thinner.
Symptoms and course
Unfortunately, the disease can occur without any symptoms for a long time. The patient does not experience pain, so he consults a doctor only when the infection has penetrated deep into the bone.
Signs of jaw necrosis:
- pain in an infected tooth or in the socket of an extracted one;
- loosening of teeth;
- swelling so severe that it disrupts the symmetry of the face;
- purulent discharge from the gums;
- putrid odor from the mouth;
- pain when swallowing, chewing, talking.
The main symptom of osteonecrosis of the jaw is bone exposure
.