Necrosis is a serious pathology accompanied by the death of gum tissue. It is quite rare in dental practice. The danger of this process lies in its irreversibility, asymptomatic course in the early stages of development and serious complications that it can lead to if the necessary measures are not taken in time. Find out what can trigger necrosis of gingival tissue, what the dead areas look like, what symptoms should alert you and where to go if they are identified.
Gum necrosis
Causes of necrosis
Types of gum necrosis and treatment
Symptoms of the disease
Diagnosis of the disease
Prevention of the development of gum necrosis
Gum necrosis (from the Greek nekros - dead) is the death of tissue that occurs due to cessation of blood circulation. This disease is difficult to detect at an early stage, as its symptoms are barely noticeable. Another danger is that this process is irreversible. Therefore, if the doctor has diagnosed gum necrosis, it is important to take appropriate measures as soon as possible to prevent the development of pathology. In this article we will look at the causes of necrosis, its types, and also tell you how to avoid it.
How dangerous is this pathological phenomenon?
If you start the process, it will inevitably lead to irreversible consequences. The affected tissues do not have a chance to recover, and the further the necrosis goes, the higher the likelihood of losing teeth and losing chewing function. The addition of infections can provoke the development of osteomyelitis of the jaw - purulent-necrotic destruction of bone tissue structures. Less commonly, the pathological condition is complicated by general blood infection - sepsis.
You need to understand that necrotic areas in the oral cavity become a suitable environment for the proliferation of harmful microorganisms. The problem is that the initial stages of the pathology are quite difficult to diagnose. If the problem has already become pronounced, it will be much more difficult to treat.
Necrotic areas in the oral cavity become a suitable environment for the proliferation of harmful microorganisms
Causes of necrosis
Table 1. Causes of gum structure destruction
| Causes of necrosis | How it manifests itself |
| Insufficient oral hygiene | Plaque forms, which leads to the development of gingivitis, periodontitis, and periodontal disease. |
| Injury to the gums due to malocclusion or ill-fitting dentures | This disrupts blood flow and blood circulation stops in certain segments. |
| Hormonal disbalance | During pregnancy, adolescence, with diseases of the endocrine system and blood. |
Sometimes the disease can occur due to prolonged exposure to cold, high temperatures or arsenic, which is part of the dental pastes used in root canal treatment. For example, if a temporary filling does not close the dental canal tightly, the paste can come out, causing tissue necrosis.
Classification
The course of the disease caused by infection can be acute, chronic or subacute.
According to location they are distinguished:
- osteonecrosis of the lower jaw;
- necrosis of the upper jaw.
By type of infection:
- endogenous - infection occurs as a result of dental diseases;
- hematogenous - pathogens enter the jaw through the bloodstream.
Also distinguished:
- medicinal (bisphosphonate);
- traumatic.
The American Dental Association defines the following stages of disease development:
Stage 0
– toothache that radiates to the temporomandibular joint or sinus. Mobility of teeth, with intact periodontium. The appearance of fistulas, cysts, fluxes.
Stage 1
– exposure of a section of bone without severe pain
Stage 2
– exposure of a section of bone, accompanied by pain and inflammation
Stage 3
- exposure of a section of bone that extends beyond the alveolar (the one in which the tooth is located) bone. With necrosis of the lower jaw, the jaw is affected down to the lower edge. Bone tissue atrophy occurs. This is the stage of pathological fractures. With necrosis of the upper jaw, the zygomatic arch and maxillary sinus are affected. Numerous fistulas are formed.
Types of gum necrosis and treatment
The treatment plan is developed individually for the patient and depends on the type of necrosis.
Table 2. Treatment plan depending on the type of anesthesia
| Type of gum necrosis | How to determine | Treatment |
| Dry | Dead areas dry out and decrease in volume. There are no signs of inflammation or intoxication. | The affected areas are removed, the surrounding tissues are treated with antiseptics. After the procedure, the doctor prescribes drug therapy. |
| Wet | It is considered the most dangerous form. Accompanied by swelling and increased hyperemia. | They open purulent foci, cut out dead tissue, dry the gums, and carry out antiseptic treatment of the oral cavity. After – drug therapy |
Once the necrotic process has stopped, bone grafting may be required to improve aesthetics.
Signs of normal wound healing
After a tooth is removed, a hole is formed in the empty area in which a natural blood clot accumulates. It is very important to monitor it closely. This substance must not be removed, scrubbed, washed or dissolved. A blood clot is the most reliable protection of a wound from infection and inflammation.
Gum restoration begins 3-4 days after tooth extraction. If the operation was traumatic, the healing process lasts 5-7 days. After removal of wisdom teeth (“eights”), the healing process can exceed 10 days. The back teeth are the most “complex”, as they have many canals, so after their removal the risk of gum inflammation is especially high.
Within 5-7 days after tooth extraction, a white film appears at the bottom of the empty socket. This film is an absolutely normal reaction of the body, as protective fibrin covers the wound from “attacks” of pathogenic organisms. Just like a blood clot, the film should never be processed.
The speed of healing of the hole depends on a number of factors:
- depth of the operation performed;
- localization of the focus of the operation;
- associated dental problems;
- the state of immunity and other characteristics of the patient’s body.
If the gums are swollen and begin to bleed within half an hour to an hour after tooth extraction, this is normal. However, if the inflammation does not subside within a few hours, be sure to contact your surgeon.
Symptoms of the disease
Signs of the disease differ depending on the stage.
Early.
The tissues are slightly affected, darkening of the enamel and pale gums may be observed.
Average
. Swelling of the interdental papillae, a gray coating forms on the mucous membrane, and bad breath appears.
Heavy.
Swelling of the gum tissue - it turns black and ulcers appear on it. Appetite disappears, body temperature rises to 39 C°.
Last
. The epithelium dies, severe pain is felt in the gums, the necks of the teeth are exposed, and the dental units become loose.
Diagnosis of gum necrosis
Often the problem is identified during an examination by a dentist, without any complaints from the patient. In some cases, symptoms are present: pain, bleeding, flushing, bad breath.
Other signs of the disease may include:
- swelling of the mucous membrane;
- digestive problems;
- problems with swallowing;
- deterioration of health.
During diagnosis, the doctor does an X-ray examination and conducts an instrumental examination. The image allows not only to identify the necrotic process, but also to determine the stage, possible complications, etc.
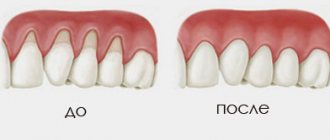
Treatment for gum recession
If the gums on a tooth have receded, the dentist decides how to treat and restore the atrophied tissue after examination and diagnosis.
The method of treating recession depends on the form of the pathology, the number of affected teeth and other factors.
In the initial stages of the disease, therapeutic measures can be used:
- professional cleaning, removal of tartar and plaque;
- cleaning periodontal pockets using closed curettage;
- laser therapy, electrophoresis, current therapy, UV irradiation;
- therapeutic injections based on biogels;
- taking medications - antibiotics, vitamins;
- hygienic rinses with lotions and herbal decoctions.
In the mild stage, it is important to stop the inflammatory process and restore blood circulation in the tissues, as well as eliminate the cause of the pathology.
In advanced cases, surgery cannot be avoided. It is carried out in several ways.
Flap reconstruction or plastic surgery. The gum tissue is cut and the root canals are cleaned. The missing tissue is transplanted using tissue from a nearby unaffected area or from the patient's palate. The technique is traumatic, but allows you to quickly and completely restore the gums.
Regeneration or regrowth of damaged tissue. At the first stage, the cause of the recession is eliminated, after which a membrane is applied to the gum, which stimulates the growth of bone and soft tissue. Subsequently, the membrane is removed or resorbed using resorbable membranes.
If there is atrophy of the gingival contour on the upper jaw or if the gums on the lower teeth have receded, what to do and what treatment to resort to depends on the clinical picture.
And timely diagnosis and regular examination by a specialist will help avoid the development of pathology and unnecessary problems.
Prevention of the development of gum necrosis
Interventions are often based on maintaining oral health and preventing dental diseases.
- Regular teeth cleaning and professional hygiene.
- Quitting bad habits (smoking, alcohol).
- Timely correction of the bite to prevent trauma to the mucous membrane and accumulation of dental plaque.
- Balanced diet, taking vitamins if necessary.
- Timely treatment of diseases of teeth and gums, gastrointestinal tract, endocrine diseases, etc.
After treating necrosis, it is important to prevent its reappearance. Proper oral care and mandatory visits to the dentist once every six months will help with this.
Causes of jaw bone destruction
The disease develops due to a combination of several factors. Under other identical conditions, patients are at risk:
- with poor oral hygiene;
- with periodontitis;
- after dental surgery, including tooth extraction;
- taking large doses of bisphosphonates for a long time;
- during chemotherapy and corticosteroid therapy;
- undergoing treatment with anticancer drugs;
- with diabetes;
- with poorly fitting, chafing dentures.
Infections of any etiology significantly increase the likelihood of getting sick. Untreated, carious teeth open the way for pathogens not only into the oral cavity. In advanced cases, when purulent discharge begins, the infection enters the general bloodstream and spreads throughout the body. On the other hand, sinusitis, otitis, and sore throats are a huge number of pathogens that provoke serious dental diseases. Complications in both cases can lead to osteomyelitis, and this can lead to necrosis of the jaw.