When the gums become inflamed, swollen and bleed, even if the symptoms are very mild, we can talk about a disease such as gingivitis.
Unfortunately, there is nothing special about such a diagnosis, since healthy periodontal tissue is found in only three percent of our fellow citizens. We are accustomed to ignoring minor manifestations of this disease, but it can lead to damage to deeper tissues, after which the process becomes irreversible. When gingivitis develops into periodontitis, doctors can only stop the disease for a while, but one day there comes a time when a person loses teeth. Therefore, it is very important to regularly check your gums for inflammation, and if gingivitis is detected, actively engage in treatment.
Patients often underestimate the seriousness of the situation and try to recover on their own. This is not the best move, because in the fight against gingivitis, reliable diagnosis and a properly designed course of treatment are important. And in order to be able to effectively fight the disease, you need to have a certain understanding of it.
Negative or iodine-negative Schiller test
Often, only with the help of a test with Lugol's solution, it is possible to identify areas of pathologically altered epithelium, when upon examination they are visually practically indistinguishable from healthy ones in color and relief, since they do not rise above the surface of the surrounding tissues.
With a negative or iodine-negative Schiller test, the altered epithelium will be stained with Lugol's solution in different shades. The changed areas during the Schiller test have a lighter color, with clear edges - the so-called silent iodine-negative area (usually keratinized epithelium).
Pathologically changed cells are stained with Lugol's solution with different shades, depending on the type of damage and the degree of keratinization (keratinization) of the tissue. In this case, the iodine solution stains only the changed integument (epithelium) with varying intensities of canary yellow color.
Symptoms of gingivitis
Despite the fact that there are many causes and types of gingivitis, dentists most often encounter catarrhal, usually chronic, gingivitis. Its very first symptoms are slightly swollen gums with redness, as well as discomfort on the teeth from hot and cold water.
The next manifestation is bleeding gums during hygiene procedures; this is already an average form of the disease. It is very important to start treating it immediately when a symptom is detected. And finally, if your gums bleed at night, then you have a severe form of gingivitis. It requires urgent professional intervention.
Less common symptoms are:
- yellow or red sores,
- gum overgrowth
- atrophy, pain.
Schiller test value
Of great importance in the differential diagnosis of normal and atypical patterns is the color shade and the clarity of the zone boundaries.
The presence of clear boundaries indicates an unfavorable situation. Benign lesions usually have less sharp, blurred contours.
Thus, the test expands diagnostic capabilities and allows:
- preliminary assess the degree of damage, size, depth and number of pathologically changed areas;
- determine patient management tactics;
- evaluate the effectiveness of treatment measures,
- to clarify the features of changes in stratified squamous epithelium under various physiological conditions (pregnancy, menopause, contraception).
Causes
Gingivitis in most cases has several causes.
Firstly, rarely do any patients satisfactorily monitor oral hygiene, so first plaque and then tartar form on the teeth. Tartar hides a lot of pathogenic bacteria.
Secondly, many of us have gastrointestinal diseases, which also provoke gingivitis.
Thirdly, often in the oral cavity, or in general in the human body, immune defense is reduced. The reason for this is an unhealthy lifestyle, vitamin deficiency, bad habits, and chronic conditions such as stress.
More rare causes include burns of the mucous membrane, teething, heart disease, diabetes and others.
In addition, incorrectly installed veneers and braces, poorly made, old and decaying fillings can lead to increased gingivitis.
Benefits of the procedure
Diagnostic colposcopy with the Schiller test allows you to give an objective assessment of the condition of the vulva, vagina and mucous membrane of the cervix, identify pathologies of the epithelial zones, and establish the nature of the detected neoplasms. The procedure is a highly accurate diagnostic method. It is short-lasting, does not cause pain and has no side effects.
Indications
- Colposcopy of the vagina is prescribed if the presence of:
- cervical polyps;
- papillomas and conilomas;
- cercivita;
- cervical cancer;
- precancerous changes in the tissues of internal organs.
The basis for the procedure is also any deviation that was detected during the examination or when taking a smear. Colposcopy is indicated for all women of reproductive age and should be performed at least once a year. It is necessary to do a Schiller test twice a year for representatives of the fair sex who are at risk: patients during menopause, after a miscarriage and a sexually transmitted disease, surgical abortion, with a family history of various gynecological pathologies.
Reasons for visiting the clinic are also menstrual irregularities, vaginal discharge (unpleasant odor, pus, blood), pain and discharge during sexual intercourse, itching in the genital area.
Contraindications
Colposcopic examination has no contraindications.
Preparation
The reliability of the results of colposcopy with the Schiller test depends on preparation. Gynecologists recommend adhering to the following rules:
- Refrain from sexual intercourse 2-3 days before the procedure;
- Before visiting a gynecologist, do not use intimate gels, deodorants and other cosmetics, as they can affect the composition of the microflora;
- A few days before the analysis, avoid starchy and sweet foods, as well as foods that cause the formation of gases, alcohol and nicotine;
- A week before the procedure, stop taking hormonal medications and antibiotics.
Seasonality
The examination can be carried out at any time of the year.
Process
- Visual examination of the genitals;
- Insertion of a gynecological speculum into the vagina;
- Installation of a colposcope;
- Treatment of the area under study with 3% acetic acid;
- Performing the Schiller test.
Rehabilitation
During the procedure, the patient does not experience pain; after it, natural reactions sometimes appear (burning, tingling), which go away on their own after a few hours. After diagnosis, you can return to your normal lifestyle.
Process
The test is carried out using a solution consisting of iodine, potassium iodide and distilled water.
During the test, the doctor opens the woman's cervix using a speculum. Next, using a tampon, the cervix is cleared of any secretions and mucus present. Having finished this, Lugol's solution is administered.
This solution should be in such quantity that the cervix is completely immersed in it. In a number of situations, the area under study is lubricated with a swab, which is pre-wetted in a composition consisting of glycerin and Lugol's solution. Next, the solution is removed, and the treated area is dried using a cotton swab. The technique of the procedure ends with another examination of the condition of the cervix.
The result will be in just 5 minutes, the procedure itself is painless, so no anesthesia is used. But having the solution in the vagina can cause some discomfort.
There is no point in conducting a test at every visit to the gynecologist. It is enough to perform the Schiller test once a year. If a woman is diagnosed with some kind of disease, then it is considered necessary to carry out the procedure 2-3 times a year until the test is negative.
Determination of the diagnostic method - Schiller-Pisarev test in dentistry
The high prevalence of periodontal pathologies and the need for their objective diagnosis in dentistry have led to the emergence of a whole set of indices. These indices are aimed at monitoring the dynamics of the disease over a certain time period, assessing the depth and extent of the pathological process, allowing one to compare the effectiveness of the therapeutic methods used, and processing the results mathematically.
There are several types of periodontal indices - complex, irreversible, reversible.
Reversible indices assess the dynamics of the pathological process and the effectiveness of the used
therapeutic techniques. They are calculated taking into account indicators of bleeding gums and bad breath, pocket depth, and tooth mobility. Irreversible characterizes the degree of bone tissue resorption and gum atrophy. Complex ones allow for a comprehensive assessment of the condition of periodontal tissues.
The Schiller-Pisarev test involves intravital staining of gum glycogen - the content of this component increases significantly during periodontal inflammation. That is, intense staining of the gums indicates that it is inflamed. The test can also be used after completion of a course of treatment and to draw up a further course of action.
Preparing for the study
In order to prepare yourself for the Schiller test and get accurate results, you must follow a number of certain rules. First of all, two days before the study, sexual intercourse is not advisable, in addition, there is no need to douche. The day before the test, doctors do not recommend using suppositories or tampons, various gels and ointments. While taking a shower, it is prohibited to use intimate hygiene products.
By following the simple instructions from the list, you can get reliable results. It is worth noting that the doctor will tell you about them directly when prescribing the procedure.
Gynecologists
- Levshina Natalya Vasilievna
Experience: 20 yearsObstetrician-gynecologist of the highest qualification category
Rating: 0/5 — 0 votes
Make an appointment
- Mikhailidi Irina Arkhimedovna
Experience: 11 years
Head of the gynecological department/obstetrician-gynecologist, ultrasound diagnostics doctor, Ph.D.
Rating: 0/5 — 0 votes
Make an appointment
- Paneva Svetlana Alexandrovna
Experience: 40 years
Obstetrician-gynecologist of the highest qualification category, Honored Doctor of Russia
Rating: 0/5 — 0 votes
Make an appointment
Effective treatment begins with accurate and timely diagnosis. One of the most informative methods in the field of gynecology for examining the mucous membrane of the vagina and cervix is extended colposcopy with the Schiller test.
Indications
In gynecology, colposcopy together with the Schiller test is considered mandatory in the case of preventive medical examinations.
In addition, this technique is prescribed in the following situations:
- spotting after sexual intercourse;
- together with a biopsy to study the condition of the genital organs;
- in case of presence of papillomavirus;
- when checking for malignant formations and precancerous conditions;
- in the presence of various inflammatory processes;
- as a control for various therapeutic procedures related to the cervix;
- before planning a pregnancy.
This test is also performed if itching, unusual discharge or chronic infectious diseases occur.
Thanks to the Schiller test, a gynecologist can detect many diseases of the cervix, which in the initial stages occur without pronounced symptoms.
The test performed so well that many do not even think about the fact that the results obtained may not always be accurate. But the procedure has disadvantages, this is explained by the following factors:
- the epithelium does not in all cases react with iodine present in Lugol's solution;
- after menopause, the upper female layers of the uterus become thinner and stop coloring;
- due to improperly placed speculum, there is a possibility of injury to the epithelial layers.
But these factors arise quite rarely, and when choosing a quality clinic, their likelihood is reduced to zero.
Result: index calculation, assessment of gum condition
For objectification purposes, the Schiller-Pisarev test is expressed in numbers (scores). The color of the papillae is rated at 2 points, the gingival margins at 4, and the gingival alveoli at 8 points. The total amount obtained is then divided by the number of teeth in the study area. That is, the calculation formula looks like this:
Iodine number = Sum of assessments for each tooth / Number of teeth examined.
The result is an iodine number in points. Evaluation of results by points:
- mild inflammation – up to 2.3 points;
- moderate inflammation – 2.67-5.0 points;
- severe inflammation – 5.33-8.0 points.
The peripheral circulation index (abbreviated as IPC) is also determined separately, taking into account the ratio of the time of resorption of hematomas that appeared under vacuum and the resistance of gingival capillaries. Test indicators are assessed in points, their ratio is expressed as a percentage. The index is calculated using the following formula:
- resistance of gum capillaries (scores);
- period of hematoma resorption (scores).
Based on index indicators, the functional state of the peripheral circulatory system is assessed. An IPC from 0.8 to 1.0 is considered normal, 0.6-0.7 is a good condition, 0.075-0.5 is a satisfactory condition, and from 0.01 to 0.074 is a decompensated state. You may be interested in learning how to strengthen teeth with periodontal disease.
Point system used to calculate the IPC (points are points)
| Resistance of gum capillaries | Period of resorption of vacuum hematomas |
| 1-10 seconds, 1 b. | 2.5 days, 10 b. |
| 11-20 seconds, 2 b. | 3 days, 20 b. |
| 21-30 seconds, 4 b. | 3.5 days, 40 b. |
| 31-40 seconds, 6 b. | 4 days, 60 b. |
| 41-50 seconds, 8 b. | 4.5 days, 80 b. |
| from 50 seconds, 10 b. | 5 days, 100 b. |
Gingivitis: different causes - one outcome
In our age of the Internet, when a person notices symptoms of gingivitis, periodontitis or another problem that worries him, the first thing he does is not go to the doctor, but to a professional dental forum. But postponing a visit to the periodontist when bleeding and inflammation of the gums appears is not the wisest decision. You should not engage in self-diagnosis: entrust the health of your teeth and gums to professionals.
Gingivitis: my gums hurt
The process, which is characterized by gum inflammation, swelling, redness and bleeding, is called gingivitis and is one of the most common periodontal diseases in both children and adults. Only 3% of people can boast of absolutely healthy gums. How to get into such a small percentage of lucky ones? The answer is simple - follow the necessary measures to prevent gum inflammation, regularly visit the doctor and not let even seemingly harmless signs of an incipient disease take their course.
Gingivitis is the last of all diseases in periodontology in which the inflammatory process can still be stopped. Next comes periodontitis, a disease in which inflammation spreads to other periodontal tissues. From this point on, treatment is based only on bringing the disease into remission and attempts to relieve symptoms as much as possible at the time of relapses, as well as in the future when it is necessary to resort to tooth extraction. Therefore, gingivitis in children and adults requires increased attention in order to avoid serious periodontal problems.
What can gingivitis be like: classification
Gingivitis differs in the nature of its course:
- Acute gingivitis is a disease whose symptoms appear suddenly and progress quite quickly.
- Chronic gingivitis is a sluggish process, the symptoms of which increase gradually.
- Aggravated gingivitis (recurrent stage of a chronic process) is an increase in the symptoms of a chronic disease.
- Gingivitis in remission is the moment of complete relief of all symptoms.
The form is:
- catarrhal gingivitis, which is manifested by swelling and redness;
- ulcerative (ulcerative-necrotic) gingivitis, with necrotic (dead) areas of the gums;
- hypertrophic gingivitis, in which there is a significant increase in the volume of gum tissue and its bleeding;
- atrophic gingivitis, on the contrary, is characterized by a decrease in the volume of gingival tissue;
- desquamative (geographic) gingivitis, which is manifested by intense redness and abundant desquamation of the epithelium of the mucous membrane.
According to its distribution in the oral cavity, gingivitis can also be local (affects some areas of the teeth) and generalized (the process affects the gums of the entire jaw or both jaws). And according to severity - mild, moderate and severe gingivitis.
Etiology and pathogenesis of gingivitis: why, what and how
Most often, gingivitis develops as an independent disease, but sometimes the causes of its occurrence are acute and chronic diseases of the gastrointestinal tract, cardiovascular system, hematopoietic organs, infectious diseases, and changes in hormonal levels. In this case, gingivitis is one of the symptoms of the underlying pathology. The causes of gingivitis can be internal or external.
Internal include:
- tooth growth that injures the gums - the eruption of wisdom teeth;
- vitamin deficiency, hypovitaminosis (most often lack of vitamin C and zinc);
- weakened immune system;
- metabolic disease;
- allergic diseases;
- diabetes;
- stress, mental illness;
- anomalies and various deformations of the gums;
- diseases of the gastrointestinal tract.
External reasons are a number of factors:
- physical (injuries, burns);
- chemical (the influence of aggressive substances);
- medical (incorrectly applied fillings, incorrectly installed veneers, traumatic wearing of braces);
- bad habits (smoking, mouth breathing);
- biological (infectious process);
- hygienic (insufficiently thorough hygienic procedures).
Toxins from microorganisms that enter the oral cavity with food and water, as well as those that live there permanently, form dental plaque (plaques) due to insufficient hygiene measures. They are the most common cause of the inflammatory process.
Inflammation can develop differently depending on the cause. Chronic catarrhal gingivitis occurs most often due to unsatisfactory hygiene measures or as a result of gum injury or burns. Hypertrophic gingivitis is caused by crowded teeth, incorrectly installed fillings or dental crowns, as well as changes in hormonal levels, for example, during pregnancy (pregnant gingivitis) or puberty (adolescent or juvenile gingivitis). Necrotizing ulcerative gingivitis (Vincent gingivitis) is usually caused by an infectious process. It occurs due to the activation of two microorganisms (Vincent spirochete and spindle bacillus) against a background of weakened immunity, hypothermia, stress or malnutrition.
Forms of gingivitis: their symptoms and diagnostic methods
Signs of gingivitis directly depend on the nature of the disease and its form. Let's look at each form of gingivitis separately. So, complaints and visual inspection.
Catarrhal gingivitis
This form of the disease usually occurs without obvious pain. Its immediate symptom is bleeding gums when brushing teeth, eating solid foods and other mechanical effects on the dental system.
Ulcerative-necrotizing gingivitis
This is one of the most unpleasant forms of gingivitis, which is characterized by a feeling of itching of the gingival papillae, severe pain, copious flow of saliva, fever, inflammation of the lymph nodes and the formation of necrotic areas of the gums.
Hypertrophic gingivitis
Patients suffering from this form of gingivitis complain of severe pain, constant bleeding of the gums and a significant increase in the volume of the gums, which can partially cover the crowns of the teeth from the outside (not from the tongue). At the same time, the patient’s gum remains quite hard and under it, on the teeth, tartar forms, which creates favorable conditions for the proliferation of microorganisms. With hypertrophic gingivitis, teeth may move slightly.
Atrophic gingivitis
The last and most advanced stage of gingivitis, often leading to periodontitis, is atrophic gingivitis. With it, the gum tissue becomes thinner, decreases in size, the necks of the teeth, and sometimes their roots, are exposed. Teeth become more sensitive to temperature changes (cold or hot drinks, frosty air), to sour or sweet foods, to the mechanical impact of a toothbrush.
Desquamative (geographic) gingivitis
The symptoms of this form of gingivitis differ from others by pronounced red spots on the gums, desquamation of the upper layer of the epithelium, the appearance of blisters on the gums and the formation of mouth ulcers and erosions.
Diagnostic tests
Schiller-Pisarev test
This test is based on determining the level of glycogen in the gum. Its amount increases significantly during inflammation, while healthy gums do not contain glycogen. Lubricating the inflamed gums with Schiller-Pisarev solution gives a color change reaction from light brown to brown. This research method is used to make diagnoses of both periodontitis and gingivitis.
Assessment of oral hygiene level
A solution (2 g of potassium iodide, 1 g of crystalline iodine, 40 ml of distilled water) is applied to the outer surface of the six lower front teeth.
The assessment is carried out using a five-point system and each tooth is assessed separately:
- 5 points – complete staining of the entire tooth surface;
- 4 points – staining of ¾ of the tooth surface;
- 3 points – staining of half the tooth surface;
- 2 points - staining of a quarter of the tooth surface;
- 1 point - absence of any staining of the tooth surface.
Then the scores of all examined teeth are summed up and divided by their number (usually the test is carried out on six teeth). This is how the hygiene index is obtained.
As a result, the quality of hygiene is assessed:
- 1.1-1.5 points – good hygiene index;
- 1.6—2.0—satisfactory hygiene index;
- 2.1—2.5—unsatisfactory hygiene index;
- 2.6—3.4—poor hygiene index;
- 3.5-5.0 - very poor hygiene index.
Vacuum test according to Kulazhenko
Using a Kulazhenko vacuum apparatus, it is possible to determine the time of hematoma formation when a vacuum is applied to the gum area. Typically, the test is carried out in the incisor area by placing a tube of the device on the gum. The formation of a hematoma in 60 seconds indicates the normal condition of the gums, while the appearance of a hematoma in 29-30 seconds signals an inflammatory process.
Oxygen tension in gum tissue
The sensor of the device is applied to the gum, and the device records the level of tissue hypoxia. Reduced oxygen tension indicates a prolonged inflammatory process.
Differential diagnosis of gingivitis
It is based on the complaints presented to the patient, a visual examination of the patient, the results of functional tests and laboratory tests. The goal of differential diagnosis is to distinguish gingivitis from other periodontal diseases, such as periodontitis and periodontal disease.
The main feature that distinguishes gingivitis from other periodontal diseases is that the inflammatory process affects only the gum tissue, the remaining structures (muscle ligaments that hold the tooth in the jaw and bone tissue) remain unchanged.
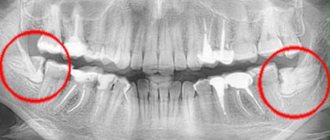
Along with this symptom, gingivitis is not characterized by periodontal pockets, exposure of the necks of teeth, or their mobility. And the x-ray shows no signs of bone resorption.
Identifying gingivitis in a timely manner, determining its form and prescribing the correct treatment is the task of a periodontist. But not to forget about prevention and regularly visit the dental clinic is the maximum program for the patient. This is the only way to avoid a more serious periodontal disease – periodontitis.