If you are concerned about facial asymmetry:
- Don't rush to see a surgeon!
Any surgical intervention is a risk. Especially if the operation does not eliminate the cause of the problem.
- Don't rely only on cosmetics!
You can paint and repaint a damaged car as much as you like. But that won’t stop her from being beaten. It's the same with the face...
Treatment at the Orto-Artel clinic without surgery!
We will help you understand the correction of facial asymmetry. And we will decide “wisely”, based on the reason.
Problems of facial aesthetics are of more and more concern to our patients. “How to correct facial asymmetry?”, “How to correct an asymmetrical face?” or “If the face is not symmetrical, what should I do?” We hear such questions very often. But how is this usually solved in other clinics? Cosmetologists, plastic surgeons. And all of them are in demand and promise good results. But is turning to a surgeon always justified? And can a cosmetologist always help? And most importantly, is there an alternative to surgery and all these “Botox”, “golden threads” and other “medicines” for the face? Indeed, very often, in pursuit of aesthetics, wanting to get results here and now, patients forget about the main thing - health.
Treatment in installments
The Orto-Artel clinic offers installments for the entire process of treating any disease. Personal conditions are considered on an individual basis.
Find out more
or call 8 (495) 128-11-74
One of the most common problems is various types of facial deformities. The range of such asymmetries, as well as complaints and tasks that patients set for themselves in order to achieve a harmonious face, is very diverse. Some people don't like the fact that the right and left halves of the face are not the same. Someone is concerned about different eye sizes (see “Deformation of the cranial bones”). Someone has an asymmetrical jaw: the lower jaw moves to the side when opening the mouth, or the center of the upper jaw (the line between the central upper incisors) is shifted to one side (see “Crossbite”). And some people have ears at different levels and protruded differently. Someone’s jaw protrudes (see “Mesial bite”) or, conversely, “sinks” (see “Distal occlusion”). And someone has an asymmetrical chin.
In general, our patients have a great many complaints and complaints. But, despite this variety of expression and manifestations of facial asymmetries, these problems are corrected, as a rule, for some reason very superficially: either cosmetologists “inject”, “pump” or “rub” something, or surgeons do plastic surgery, something cutting or enlarging.
But it should, however, be understood that an asymmetrical face is not a diagnosis. This is just a symptom of a problem. A symptom, in medical terms. But treating symptoms is a thankless task. It is much more important to find the cause of the problem and eliminate it.
Diagnostics is the first and key step in the treatment of facial asymmetry. Do you want to know why it’s impossible to do without diagnostics?
Face distorted: reasons
Basically, various neurological diseases are hidden behind changes in the facial muscles. Below are the main reasons:
- facial paralysis;
- blepharospasm;
- acute cerebrovascular accident - stroke.
The most dangerous condition listed above is stroke. It requires immediate medical attention and hospitalization, as prompt initiation of treatment increases the chances of successful rehabilitation.
Above is a photo with the distorted face of a woman who suffered from a stroke.
How to correct facial distortion after a stroke
The process of facial restoration after a stroke is a complex and labor-intensive process, which consists of long-term drug therapy and rehabilitation measures. If you follow all the recommendations and perform special exercises, even in the most difficult cases, you can correct the distortion, as well as return your face to normal expression and facial ability.
Drug therapy must give a certain result:
- restore blood circulation;
- normalize intracranial pressure;
- relieve the inflammatory process;
- reduce swelling;
- eliminate paralysis of the facial muscles.
In parallel with drug treatment, various procedures are prescribed that help restore motor and swallowing reflexes. These include:
- massage;
- physiotherapy;
- a set of facial gymnastics exercises.
Facial exercises immediately after a stroke require some effort and patience from the patient. They are difficult to perform, but constant practice helps restore mobility.
Facial nerve paralysis: causes
Being one of the conditions that can cause the face to become skewed, it requires proper treatment to restore the previous shape of the face. Paralysis is the inability to move any part of the body, in this case, the facial muscles. A number of pathological conditions can lead to this:
- infectious diseases (chicken pox, herpes, rubella) that lead to inflammation of the facial nerve - neuritis;
- inflammation of the middle ear - otitis media;
- traumatic brain injuries;
- inflammation of the meninges - meningitis;
- brain tumors.
Fortunately, all of the serious causes listed above (brain injuries, tumors, meningitis) are rare. But in most cases, the cause of the paralysis cannot be determined, and then doctors make a diagnosis of “idiopathic Bell's palsy.” This condition is the most common cause when a child's face is distorted.
Risk factors
There may be a hereditary predisposition. Acute neuritis associated with a complicated family history is found in 4% of cases. The disorder may be associated with autosomal dominant gene transmission. The presence of other neurological diseases in close relatives, such as trigeminal neuralgia and multiple sclerosis, increases the patient's risk of developing the disease. Doctors also consider the influence of other conditions and symptoms, including lifestyle factors.
Known risk factors:
- Age. Neuritis is most often diagnosed in patients aged 15 to 60 years. In children, secondary facial paralysis is usually detected.
- Diabetes. Elevated blood glucose levels lead to damage to small vessels that supply nerve fibers.
- Traumatic brain injury. With TBI, damage to the brain matter and deformation of the skull bones with subsequent compression of the facial nerve are possible.
- Pregnancy. Facial paralysis occurs especially often during the last trimester or a week after childbirth.
- Chronic infections of the upper respiratory tract. From the respiratory tract, viruses can spread to neighboring tissues.
- Pre-existing neurological diseases, including multiple sclerosis, ophthalmoplegia and essential tremor.
- Congenital or acquired decreased immunity. Usually we are talking about HIV infection and its complications, which increase the risk of developing a herpetic or cytomegalovirus form of the disease.
Preventive measures aimed at eliminating risk factors are effective for secondary neuralgia.
Facial nerve paralysis: symptoms
Damage to the facial nerve is characterized by the fact that the face is skewed on only one side, and asymmetry of the entire face is observed. This means that the patient has both the lower part of the face affected (the corner of the mouth is drooping, he cannot bare his teeth, the tongue deviates to one side) and the upper part of the face (one eye is closed or the eyelid is drooping).
When diagnosing this pathology, the doctor may resort to the following additional examination methods:
- electromyography - the study of facial muscles by recording the signals that come from them;
- magnetic resonance imaging - visualization of the brain using a tomograph, which will help exclude brain damage (tumor, injury, stroke).
Why does facial asymmetry occur?
Physiological conditions
Slight static (visible at rest) facial asymmetry is a physiological norm and occurs in almost all people.
A difference in proportions within 3-5 degrees or 2-3 mm is considered normal. Sometimes visually noticeable differences between the halves of the face are aggravated by facial features. This asymmetry (noticeable during tension of the facial muscles) is called dynamic. The differences tend to worsen with age as a person repeatedly tenses the same muscles asymmetrically. This affects the condition of soft tissues and the formation of wrinkles.
Damage to cerebral structures and meninges
Facial asymmetry is provoked by traumatic injuries and diseases of the central nervous system of various origins. The list of pathologies includes:
- Compression of the brain.
Acutely develops as a result of severe head injury, cerebral edema. Gradually progresses with hydrocephalus, tumors, cystic formations located in the cranial cavity. - Stroke.
Occurs acutely against the background of arterial hypertension, atherosclerosis, angina pectoris. May be ischemic or hemorrhagic. The outcome of both variants of pathology is focal brain damage, causing disturbances in nervous regulation and facial asymmetry. - Encephalitis.
Focal disorders are a consequence not only of circulatory disorders, but also of inflammatory processes in the brain. Facial asymmetry is sometimes observed in patients who have had primary (tick-borne, Japanese mosquito) or secondary (influenza, measles, post-vaccination) forms of encephalitis. - Meningitis.
The cause of symmetry disorder can be the involvement of cranial nerves, the spread of infection to brain structures with the development of meningoencephalitis. The symptom is more often detected with purulent meningitis, basilar tuberculous meningitis. - Neuroleukemia.
Formed as a complication of leukemia. Facial asymmetry can be caused by dysfunction of the cranial nerves, the occurrence of leukemic meningoencephalitis, and compression of brain structures in patients with the pseudotumor form of the disease. - Progressive hemiatrophy of the face.
The gradual reduction of half the face is due to atrophy of bones and soft tissues, presumably caused by an effect on the autonomic centers. Changes appear in a limited area and eventually spread to the entire half of the face. - Oromandibular dystonia.
It is manifested by violent movements: clenching, lateral movements of the jaws, opening and closing the mouth, which are accompanied by curvature of the lips, violation of symmetry at the level of the cheeks. The occurrence of pathology is provoked by damage to the basal ganglia.
Facial asymmetry
Pathologies of cranial nerves
The most common cranial nerve disorder causing asymmetry is facial neuritis. The cause of violation of symmetry is paresis or paralysis of facial muscles. The typical clinical picture includes smoothness of the nasolabial fold, drooping of the corner of the mouth, inability to close the eyelid, and skewing of the face in the healthy direction. A type of facial paralysis is Ramsay-Hunt syndrome. Along with weakness of facial muscles, patients experience ear pain, dizziness, and hearing loss.
In patients with Bogorad syndrome, branches of the facial or abducens nerve grow into the salivary and lacrimal glands. The disease develops at an early age, less often becomes a consequence of injuries in adults, and is accompanied by lacrimation and increased salivation on the affected side. Damage to the facial nerve is manifested by paresis of the facial muscles, the abducens nerve - hearing impairment, deformation of the auricle. In children, facial asymmetry progresses as they grow.
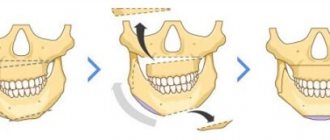
Jaw lesions
A fairly common dental cause of facial asymmetry are diseases, consequences of injuries, congenital anomalies of the jaws and TMJ:
- Arthrosis of the TMJ.
The symptom appears during the process of opening the mouth and is caused by a displacement of the lower jaw to the affected side. The disease develops gradually, accompanied by crunching, clicking, morning stiffness, and dull pain. - Ankylosis of the TMJ.
Facial asymmetry persists at rest and gets worse when trying to open the mouth. The midline of the face is shifted to the affected side. The lower jaw is retracted downwards by no more than 1 cm, horizontal movements are impossible. - Contracture of the lower jaw.
There are restrictions when opening the mouth, a decrease in the amplitude of movements of the lower jaw. The midline also shifts towards the affected side. The pathology can be unstable (inflammatory) or persistent (scarring). - Ameloblastoma.
An odontogenic benign tumor that destroys jaw tissue can reach significant sizes and cause significant facial deformation. The tumor grows slowly, and asymmetry in the jaw area becomes the first symptom of the disease. - Other benign tumors of the jaws
. The symptom is often found in osteomas, osteoid osteomas, and osteoblastoclastomas. - Cancer of the upper jaw.
Deformation occurs when the size of the neoplasia is sufficiently large and is caused by the growth of the tumor itself, the destruction of nearby anatomical structures, and inflammatory edema. - Cancer of the lower jaw.
Facial asymmetry is noted in the case of tumor growth into nearby soft tissues and deformation of the alveolar process.
Another reason for asymmetry is jaw defects, which can be congenital or acquired: resulting from injuries, osteomyelitis, tuberculosis, syphilis, and operations for cancer. In case of a defect of the upper jaw, the symptom appears due to the recession of the cheek, and may be accompanied by the formation of oronasal and oroantal anastomosis.
A defect of the lower jaw is characterized by a violation of the oval of the face. Due to the displacement of the jaw towards the midline, the asymmetry is aggravated during mouth opening. Violation of symmetry is also often manifested by micrognathia - a reduction in the jaw due to underdevelopment or previous damage. With upper micrognathia, the lower teeth overlap the upper ones (reverse overlap); with the lower variant of the pathology, a slanted chin is observed.
Diseases of the salivary glands
Inflammatory processes and space-occupying formations of the salivary gland cause deformation of the lower outer part of the face and cause asymmetry.
- Purulent parotitis.
A rapidly increasing painful swelling appears in the projection of the parotid salivary gland. An increase in temperature and symptoms of intoxication are detected. - Mucocele.
Causes facial asymmetry as a result of damage to the salivary glands located in the parotid and submandibular regions. The swelling is painless, the condition is satisfactory, there are no signs of inflammation. - Cyst.
As in the previous case, the symptom is observed when the parotid and submandibular glands are involved; pain and inflammatory manifestations are not observed. Due to infection, low-grade fever and local soreness are possible. - Adenoma.
Benign tumor with slow growth. As the size increases, along with asymmetry, discomfort and decreased salivation are noted. - Tumors.
Benign lipomas, neuromas, and angiomas form in the area of the salivary glands. Clinical manifestations of the neoplasm resemble an adenoma. The list of malignant neoplasias includes sarcomas and carcinomas, which are characterized by rapid growth and destruction of soft tissue. Pathologies are often accompanied by paresis of the facial nerve.
Other dental diseases
Other inflammatory dental pathologies that can cause facial asymmetry include:
- Periostitis of the jaw (flux).
Only the periosteum suffers, the jaw itself remains intact. Flux is often caused by dental diseases. The cause of asymmetry is local edema, the formation of an abscess under the periosteum. - Periapical abscess.
An abscess forms in the tissues around the root of the tooth, provoked by acute periodontitis. It manifests itself as severe throbbing pain in the area of the affected tooth. Facial deformity is caused by the spread of edema to the surrounding soft tissues. - Perimaxillary abscess.
Develops with dental lesions and inflammatory processes in surrounding tissues. Accompanied by a violation of the general condition, toothache, dense swelling, in the center of which a fluctuation area subsequently forms.
Non-inflammatory causes of asymmetry include crossbite, a condition in which the dentition intersects when the jaws close. May be congenital or acquired. It is characterized by a shift of the chin to the side, recession of the lip on one side, and flattening of the lower parts of the face on the other.
Facial injuries
Temporary asymmetry of the face, caused by swelling of the soft tissues, is observed with soft tissue bruises and facial hematomas. It occurs after a blow or fall, increases rapidly within a few hours, and gradually disappears over 1-2 weeks. At the recovery stage, there is a consistent change in skin color in areas of hemorrhage. In fractures, asymmetry is caused not only by swelling, but also by displacement of the hard structures of the facial skull. The cause of the symptom is:
- Fracture of the lower jaw.
The loss of symmetry is more noticeable along the outer or lower edge of the cheek. A step (discontinuity of the dentition) in the area of the fracture is detected in the oral cavity. - Fracture of the upper jaw.
The face becomes asymmetrical due to swelling in the upper part of the cheek. Hemorrhages in the periorbital area and neurological disorders are possible. - Fracture of the zygomatic bone.
Initially, the swelling is localized in the cheekbone area, and subsequently quickly spreads upward and downward along the outer surface of the face. Periorbital hemorrhages and double vision may be observed.
ENT diseases
Silent sinus syndrome occurs as a result of atelectasis of the maxillary sinus. It manifests itself as a decrease in the volume of the accessory sinus, unilateral deformation of the face: drooping of the lower edge of the orbit, displacement of the eyeball into the orbit, and recession of the cheek. The pathology develops over many years, gradually progresses, and in the final stages is accompanied by ophthalmological disorders.
In patients with cysts of the paranasal sinuses, in contrast to the previous case, asymmetry develops due to excess, and not due to lack of tissue. The symptom is detected only with large cysts and is manifested by unilateral deformation of the forehead or cheek. Pain in the sinus area, dull headaches, and recurrent sinusitis are observed.
Congenital and childhood pathologies
Facial asymmetry is diagnosed in the following congenital diseases and pathologies of childhood:
- Sturge-Weber syndrome.
A congenital disease in which angiomas form on the skin and meninges. With hydrocephalus and hemiparesis, facial asymmetry develops on the side opposite to the location of the angiomas. - Torticollis.
The congenital form is caused by underdevelopment of the sternocleidomastoid or trapezius muscle, while the acquired form is caused by various diseases and injuries. The child's ear, eyebrow and eye on the affected side are lower than on the healthy side. The palpebral fissure is somewhat narrowed. - Lhermitte-Duclos disease.
A genetically determined pathology, the main manifestation of which is a neoplasm of the cerebellum. Even before the tumor begins to grow, the disease can be suspected by asymmetry of the facial skeleton, gum hyperplasia, congenital anomalies of the hands, and some other signs. - Acute intermittent porphyria.
A hereditary disease manifested by attacks caused by disorders of porphyrin metabolism. Facial asymmetry is observed in severe cases, occurs approximately a week after the onset of gastrointestinal symptoms, and is combined with other neurological disorders. - Cleft lip.
A developmental anomaly in which one or two clefts of the upper lip are detected, located on either side of the midline. With an accompanying cleft palate, the deformity is aggravated by a “dip” in the middle part of the face and a violation of the shape of the nose. - Stigmas of embryogenesis.
Violation of symmetry can be determined by a number of small anomalies: changes in the shape of the skull, deformations of the nose, eyes, and dental system.
Other reasons
Other possible causes of facial asymmetry include:
- Hydrogen peroxide poisoning.
The symptom is detected when there is a violation of cerebral circulation, complemented by disturbances in speech, hearing, and coordination of movements. - Actinomycosis.
Asymmetry is observed in maxillofacial actinomycosis and is caused by the formation of an infiltrate in the area of the masticatory muscles and the development of trismus. - Kallmann syndrome.
With this form of hypogonadism, the symptom is caused by developmental defects and minor anomalies of the face, and is combined with eunuchoidism, cardiovascular disorders, and gynecomastia. - Botulism.
Accompanied by facial asymmetry in neurological disorders that cause paresis or paralysis of facial muscles.
Facial nerve paralysis: treatment
What to do if your face is distorted due to facial paralysis? There are a number of drug and non-drug treatment methods that will help restore the previous appearance and function of the facial muscles:
- corticosteroids - relieve inflammation of the facial nerve;
- antiviral or antibacterial agents, if the presence of an infectious process is confirmed;
- surgical intervention for a diagnosed brain tumor;
- massage;
- a set of exercises for the facial muscles;
- physiotherapy;
- moisturizing eye drops on the affected side, antibiotic ointments to prevent infection.
Gymnastic exercises
Gymnastics for the facial muscles is performed daily 5–7 times, starting with performing each exercise once, gradually increasing the number to 3 approaches.
Facial muscle movement is stimulated using the following group of exercises:
- Smile as widely as possible with your lips closed. Hold the achieved position for 5 seconds.
- Fold your lips into a “bow” and stretch them out as far as possible for 5 seconds.
- Open your mouth as wide as possible for 5 seconds. Close your lips as hard as possible for 5 seconds. Relax your muscles.
- Pronounce the vowel sounds “a”, “u”, “o”, “i”, “e”, “s” in front of the mirror as long as possible. The exercise stimulates the work of not only the facial muscles, but also the speech apparatus.
- To begin with, wink several times with one and the other eye, then alternate winks with different eyes.
- Raise your eyebrows slowly to maximum height, and lower them just as slowly.
- Move the protruding tongue up and down and left and right to the maximum amplitude.
- Move the lower jaw to the right, fix for 5 seconds. Move to the left, hold for 5 seconds. Return to original position.
- Take as much air into your mouth as possible until your facial cheeks are rounded. Keeping it from exiting through the mouth and nose, alternately press on the cheeks with your fingers on both sides.
The harmonica is an effective home exercise device for rehabilitation after a stroke. Daily exercises of 3-5 minutes stimulate the facial muscles, saturate the body with oxygen, improve blood circulation, and train memory.
Massage
Massaging the facial muscles stimulates blood circulation, improves metabolism, reduces muscle tone, and removes puffiness.
The course of treatment (type of massage, number of procedures) is determined by a neurologist during the rehabilitation period, 2 weeks after the stroke.
Blepharospasm: causes and symptoms
Another condition that can cause the face to become distorted is blepharospasm, an involuntary contraction of the orbicularis oculi muscle surrounding it.
Main reasons:
- Facial paraspasm is a disease characteristic mainly of older people. Its exact cause is unclear, but it is believed that paraspasm occurs due to an imbalance of parts of the nervous system.
- Parkinson's disease.
- Meningitis.
- Multiple sclerosis.
- Inflammation of the eyes (keratitis, conjunctivitis).
- Sinusitis is inflammation of the paranasal sinuses.
With blepharospasm, only the upper part of the face is characterized by asymmetry: the palpebral fissure gradually narrows, and sometimes the eye may suddenly close its eyes. This brings a lot of inconvenience to the patient.
Blepharospasm: treatment
If your face is distorted due to blepharospasm, you should turn to the following therapeutic methods:
- treatment of the underlying disease that caused spasm of the orbicularis oculi muscle;
- physiotherapy;
- nootropics - drugs that increase oxygen delivery to the brain and improve its functioning;
- If symptoms are severe and other treatment methods are ineffective, botulinum therapy may be prescribed, which effectively relieves muscle spasm.
Face massage
Facial massage after a stroke is included in therapeutic measures to restore facial muscles. Even if the massage is performed at home, it should only be done by a specialist. If the procedure is performed at a professional level, the result will give a stable remission.
It is not recommended to massage yourself; incorrect exposure to certain facial points can cause a relapse or worsen the patient’s condition. A correctly performed procedure normalizes blood circulation, restores the motor ability of the facial muscles and the swallowing reflex.
Stroke: causes
One of the most dangerous causes of facial asymmetry and impaired facial expressions is a circulatory disorder in the brain, which often results in a stroke. Depending on the cause that caused it, it can be ischemic (when a cerebral vessel is blocked by a thrombus or embolus), as well as hemorrhagic (when a thinned wall of a cerebral vessel ruptures).
Underlying conditions that increase the risk of stroke:
- cerebral atherosclerosis is one of the main causes of ischemic stroke;
- arterial hypertension - increases the risk of hemorrhagic stroke;
- cerebral aneurysm - sac-like protrusion and thinning of the wall of a cerebral vessel, as a common consequence of prolonged arterial hypertension;
- chronic cerebrovascular accidents;
- obesity and low physical activity.
Diagnostics
Determining the cause of facial asymmetry is most often carried out by dentists or neurologists. If appropriate symptoms are detected, the patient is referred to otolaryngologists, oncologists, endocrinologists, and other specialists. The examination plan may include the following diagnostic procedures:
- Questioning, physical examination
. The doctor establishes the time and circumstances of the onset of the symptom and asks the patient about other manifestations of the disease. Evaluates the severity of asymmetry at rest, during facial and chewing movements. Detects other changes: swelling, redness, blanching, increased local temperature, tumor formations. - Dental examination.
Includes studying the condition of teeth, gums, hard and soft palates, mucous membranes of other areas, and bones of the facial skeleton. Allows you to confirm the presence of diseased teeth, inflammation, injury, suppuration, tumors. - Neurological examination.
The specialist studies the innervation of the facial muscles, asking the patient to perform certain movements: wrinkle his forehead, raise and lower his eyebrows, puff out his cheeks, show his tongue, bare his teeth, follow the movements of the neurological hammer with his eyes. The neurologist then palpates the available nerve exit points. - Otorhinolaryngological examination.
Provides for special research. If pathology of the paranasal sinuses is suspected, echosinusoscopy or diagnostic puncture can be performed. In case of complaints of hearing impairment, audiometry, tuning fork examination, etc. are performed. For vestibular disorders, vestibulometry and rotational tests are recommended. - Radiography
. Taking into account the identified pathological changes, the patient is prescribed an X-ray of the tooth, an X-ray examination of the jaw or paranasal sinuses. In some cases, radiographs of the skull and cervical spine are necessary. - Ultrasonography
. During the examination, sonography of the salivary glands, paranasal sinuses, and soft tissues may be performed. If signs of brain compression are detected, echoencephalography is indicated. - Other visualization techniques
. Most often, CT or MRI are used to clarify the diagnosis and to study in detail the nature of the changes, the volume and location of the pathological focus. For neurological pathology, PET-CT and SPECT of the brain may be prescribed. - Lab tests
. A general blood test determines the presence and severity of inflammation; the results of a microbiological study determine the pathogen and its sensitivity to antibiotics. In case of space-occupying formations, histological and cytological examination of smears, punctures, and biopsy specimens is carried out.
Elimination of facial asymmetry
Stroke: symptoms
If your face becomes distorted during a stroke, you should immediately consult a doctor, since time plays a very important role here. Therefore, you need to know the following signs that will help you suspect the development of a stroke:
- In the vast majority of cases, only the lower half of the face is characterized by asymmetry, which is manifested by a drooping corner of the mouth, smoothness of the nasolabial fold, deviation of the tongue to one side, and the inability to show teeth or stick out the tongue completely.
- Paralysis (complete immobilization) or paresis (weakness) of a limb, typically involving unilateral damage to the arm and/or leg. It is difficult for the patient to raise his arm or he cannot stand up; with leg paresis, walking is possible, but difficult.
- Speech impairment, and the patient may have damage to both the speech understanding center, located in the frontal lobe of the brain, and the pronunciation center, located in the temporal lobe. In the first case, the patient pronounces words and sentences absolutely normally, but does not completely understand the meaning of what is being said to him. In the second case, he understands everything, but is either completely unable to say anything, or speaks separate incoherent words.
If you notice any of the listed symptoms in yourself or those around you, do not hesitate, call an ambulance immediately!
Disease Information
Facial neuritis is an inflammatory disease of the facial nerve, which is responsible for the contraction of facial muscles. In the medical literature, the pathology is also called Bell's palsy. As a rule, damage to nerve fibers causes unilateral disruption of the facial muscles. Other symptoms include spontaneous contractions of muscle fibers, weakness and decreased sensitivity of the facial skin. Signs of paralysis appear within 24-48 hours after tissue damage. In most cases, doctors are able to cure facial neuritis and restore facial expressions without any complications.
The facial nerve leaves the brain and branches in the facial part of the skull. This anatomical structure transmits electrical impulses from the brain to control facial expressions. The intermediate nerve, which joins the facial nerve fibers, is responsible for carrying sensory information to the brain. With the help of this part of the organ, a person receives sensitive information from the receptors of the skin and subcutaneous tissues of the face. Damage to the nervous system primarily affects the work of the facial muscles, and functions are usually impaired on one side of the face.
Facial neuritis is sometimes called idiopathic facial paralysis, since the exact causes of the disease are unknown. This is a common disease diagnosed in men and women at any age. According to epidemiological data, the pathology occurs at least once in life in 1.5% of the population, and patients with chronic infections aged 15 to 60 years are at risk.
Stroke: treatment
Therapy for circulatory disorders should begin as early as possible, since early initiation increases the likelihood of successful restoration of muscle function, including facial muscles. Therapy directly depends on the type and cause of the stroke.
For cerebral ischemia, drugs are prescribed that resolve the blood clot and restore normal blood circulation (acetylsalicylic acid, thrombolytic therapy).
In case of hemorrhagic stroke, it is necessary to stop bleeding in the brain tissue, which is achieved with the help of antifibrinolytic therapy (alpha-aminocaproic acid).
However, it is not only drug therapy that plays a role. If the patient’s condition is satisfactory, physical therapy and massage should be started as early as possible to restore muscle function.
Treatment options
Symptoms of the disease in most cases go away on their own within a few weeks, but without timely treatment the patient may experience complications. The main task of the doctor is to quickly eliminate the identified cause of neuritis. When selecting therapy, clinical recommendations are taken into account. Thus, in the case of idiopathic facial paralysis, therapy is aimed at restoring the functions of facial muscles and alleviating the patient’s condition. Medicines, physiotherapeutic procedures and, if necessary, surgical methods for correcting the disease are selected. Rehabilitation is underway.
Drug treatment of facial neuritis
- Corticosteroid therapy. These are anti-inflammatory drugs that help eliminate swelling in the area where nerve fibers pass. As a result, the functions of the organ are restored and the transmission of nerve impulses to facial muscles is facilitated. It is best to start using corticosteroids in the first days after symptoms of neuritis appear.
- Use of antiviral drugs. Such therapy is justified only if herpes is detected. The patient is prescribed a course of Valacyclovir or another drug. Preventing further spread of the virus in the body helps prevent the formation of a chronic form of the disease.
- The use of diuretics to combat edema. Patients are prescribed Furosemide, Triamterene or another drug. Diuretics are justified in cases of severe swelling that compresses nerve fibers.
- Use of painkillers. Non-steroidal anti-inflammatory drugs are usually sufficient to relieve pain.
- Therapy with vasodilator drugs. Nicotinic acid preparations, Scopolamine and other medications are prescribed.
During the first week of treatment, constant rest is indicated. Vitamins can be used as a general strengthening therapy.
Surgery
The decision to perform an operation is made after receiving the results of visual diagnostics. Surgery may be required for patients with brain damage, complete rupture of nerve fibers, and congenital defects of the peripheral nervous system. The torn nerve is sutured using microsurgical methods. When connective tissue scars grow in the area of nerve fibers, neurolysis is performed.
Effective surgical treatment is possible only within 12 months after the onset of the first symptoms of facial neuritis. Subsequently, irreversible changes occur. At the same time, modern surgical practice allows autotransplantation to restore the organ. Nerve fibers are removed from the lower limb and sutured to the facial nerve.