Purpose of the dental system
The biological mechanics of the dental system and its understanding lead to timely recognition of pathologies of teeth and soft tissues of the oral cavity. The normal functioning of the temporomandibular joint largely depends on the structure and normal functioning of the periodontium - the soft tissues surrounding the tooth cavity.
The anatomy and physiology of the structure of the periodontium determines the biomechanics of the structure and the characteristics of the periodontium. In addition, periodontal biomechanics helps in the functioning of other organs.
Knowledge of the laws of biological mechanics of the jaw and joints helps to design and use features, as fundamental knowledge on the topic of prosthetics and dental implants. Knowledge of the anatomical features of the jaw is necessary in the manufacture of structures and dental materials.
Devices have been developed that almost completely repeat the movements of the jaw and make it possible to reproduce anatomically similar structures to the human jaw. Popular devices include the occluder, facebow, and articulator. The latter design plays an important role in the fitting and creation of individual prostheses.
If disorders of the lower jaw occur, disruptions in articulation, speech, nutrition and swallowing occur. Today, a system of articulation of movements has been developed, led by such authors as Ganau, Gisi, Monson. These authors most accurately described the biomechanics of mandibular movements.
The authors claim that dysfunction of the lower jaw, as well as sore neck muscles, necessarily lead to breathing problems. Different angles of inclination of the lower jaw determine human health.
Occlusion is a condition characterized by full contact of both jaws, which ensures complete chewing of food. Therefore, the contact of teeth is a determining factor for the characteristics of chewing mechanisms.
The work and action of the lower dentition during chewing is due to the synchronous work of all muscles and joints. The work occurs under the influence of the central nervous system. In this case, displacements that occur spontaneously occur under the influence of the neuromuscular structure.
Conscious movements of the dentition include the moment food enters the mouth and swallowing food. The remaining movements that occur after eating food are the result of unconscious motor functions of the body.
The lower part of the human masticatory apparatus is the only moving bone in the human body. However, the connecting and muscle tissue, which sets the mechanism in motion, is of great importance in the structure of the masticatory row and in the normal functioning of the muscles.
In the structure of the lower dentition, there are several muscle groups that are responsible for various movements of the jaw.
Fundamentals of occlusion and biomechanics of the jaws: a new look at old concepts
A deep understanding of the basics of occlusion and biomechanics of the jaws is one of the most important and necessary components for providing comprehensive patient rehabilitation in dental practice. Knowledge of the principles of differential diagnosis of pain, planning of future iatrogenic intervention, as well as algorithms for the treatment of prosthetic disorders provides the doctor with all the necessary tools for further normalization of the patient’s dental status.
An orthopedic doctor simply cannot do without understanding how significant the concept of occlusion is not only in pathology, but also in a state of stable and adequate function. The formation of appropriate occlusal schemes is based on the redistribution of acting forces, because, in fact, it is precisely because of the excess of such indicators that diseases, pathologies and dysfunctions of the elements of the dentofacial apparatus arise.
Occlusal disorders can manifest themselves in the form of various structural damage to the dental status, such as pathological abrasion, fractures, and premature wear of restorative structures. In addition to the latter, functional pathologies are characterized by tooth mobility, loss of volume of soft and hard tissues, muscle pain, as well as pain and noise in the joints (the so-called clattering), limitation and impairment of movements of the lower jaw, remodeling changes in bone tissue in the structure of the temporomandibular joint . In such cases, patients form so-called parafunctional habits, the presence of which he himself does not know. Clinically, signs of such are manifested by excessive wear of one’s own teeth and various types of restorative structures present in the oral cavity.
There are different opinions regarding the relationship between the state of occlusion and disorders of the temporomandibular composition. According to the most extensive literature reviews, such associations are rather weakly expressed, as evidenced by the fact that when correcting occlusal relationships, it is not always possible to prevent the development and progression of joint pathologies. Based on the available data, the following conclusions can be drawn: only the absence of traumatic occlusal injuries, which are manifested by the action of excessively high parafunctional forces exceeding the adaptive capabilities of the body, ensures complete prevention of the occurrence of pathologies and dysfunctions, or the presence of such in the acceptable adaptation range. This conclusion is evidence-based, regardless of how ideal or non-ideal the occlusal schemes of each individual patient are. On the other hand, with prolonged exposure to excessive occlusal forces, the development of corresponding dysfunctions and diseases occurs regardless of the characteristics of a particular occlusal scheme. The corresponding pathological types of occlusion only further aggravate the course of related prosthetic diseases.
From the above it follows that if the doctor is fully familiar with the specifics of occlusal movements in a particular patient, and also understands their impact on the condition of soft and hard tissues, muscles and joints, then he can ensure the formation of such occlusal patterns that would be the most stable and least traumatic for each specific patient. In other words, understanding the basics of occlusion helps doctors not only plan future interventions, but also predict the functional rehabilitation of prosthetically compromised patients. The main connecting link between the pathology of the temporomandibular joint, the state of occlusion and the functional disorder of the dentofacial apparatus is the repeated action of excessive occlusal load, which goes beyond the adaptive range of the body. Based on this, the author considers it wrong to separate the dynamics of the application of force on human tissue from disorders and diseases developing in the same tissues - after all, in fact, these processes are of an indirect cause-and-effect nature.
The question is different: what is the true connection between the existing parafunction, the state of occlusion and functional deviations of the dentofacial apparatus. In order to understand how the jaw functions and where occlusion begins, you need to repeat in detail the anatomy of the masticatory muscles, the temporomandibular joint, and, of course, the teeth, taking into account the functional parameters of each of the above-mentioned components. After analyzing the anatomy, you should focus on how the relationship between the upper and lower jaws is generally formed, taking into account the occurrence of static and dynamic contacts between the surfaces of antagonist teeth. After this, the data obtained during the analysis can be implemented into a plan for future iatrogenic intervention aimed at eliminating structural disorders of the dentition and aesthetic problems, while ensuring not only the functional comfort of the dentofacial apparatus, but also the stability of the achieved results of complex rehabilitation.
In the course of analyzing the features of anatomy and intermaxillary relationships, doctors should look for key parameters of each of these components, on the basis of which they will subsequently make a decision regarding one or another possible treatment plan.
In this article, the author will refer to the concept of dental treatment planning, which takes into account changes in the facial profile during iatrogenic interventions, developed by Frank Spear. With significant destruction of the tooth structure, the main occlusal landmarks are simply lost, and the pathology goes beyond the boundaries of possible dental-alveolar compensation. Consequently, the clinician’s task is also to restore the supporting occlusal points of the intermaxillary relationship, and then, based on their stability, carry out further prosthetic rehabilitation. When implementing an approach to treatment taking into account changes in the facial profile, it is possible to ensure successful prosthetic reconstruction of the bite, based precisely on the position of the supporting occlusal landmarks.
Pankey rules and the concept of optimal occlusion
Dr. LD Pankey, being a pioneer and developer of comprehensive approaches to dentition restoration, proposed a specific concept that helps critically evaluate occlusion both during systemic dental rehabilitation and during everyday dental care:
- When the condyle of the jaw is completely in the glenoid fossa, all the posterior teeth exhibit equal and uniform contact, while the anterior teeth only lightly touch the opposing teeth.
- When the jaws are clenched, neither the teeth nor the lower jaw move.
- When the mandible moves in any direction, none of the back teeth contact faster or more strongly than the teeth in the anterior region.
Having analyzed these features, we can take a fresh look at the specifics of the anatomy of the dentofacial apparatus.
Anatomy of the temporomandibular joint
In Photo 1 you can see that the condyle of the mandible is in very close contact with the biconcave disc of the joint. These elements of the joint are located inside the capsule, which is protected behind by retrodiscal ligaments, and below, by means of capsular ligaments, is attached to the neck of the condylar process. Anteriorly, the superior portion of the lateral pterygoid muscle attaches to both the disc and the neck of the condylar process, while the inferior portion of the muscle attaches only to the neck of the condyle. Behind the joint is the external auditory canal. Anterior and superior to the condyle is the eminence, and directly above it is the glenoid fossa. The articular surfaces are covered by fibrocartilage, which is a smooth structure, and is supported by synovial fluid. The latter lubricates the surfaces of the joint, providing them with nutrients and oxygen, as well as ensuring the removal of possible debris. In the structure of the capsule, the number of blood tissues is very limited, or they may be completely absent.
Photo 1. Classic diagram of the anatomy of the temporomandibular joint.
When analyzing a joint, it is necessary to note the most important relationships of its individual components. First, there is the close condyle/disc/fossa connection. Essentially, they are in as much contact as possible, allowing the joint to withstand the necessary loads. On the other hand, this form of connection of the elements ensures the anatomical and functional integrity of this organ during dynamic movements of the lower jaw. In certain articular pathologies, this relationship is disrupted, which leads to permanent functional changes. It is obvious that the variation in the size, volume and shape of the temporomandibular joint is quite significant, and these differ greatly from person to person. Historically, we have assumed that the dimensions of the condylar process are relatively stable. However, recent research has established that the size of this anatomical structure can change and adapt over time and depending on the prevailing circumstances. A striking example is the increase in condyle size when using night guards. Due to the protrusion of the mandible to maintain patency of the upper airway, the condyle also remodels, increasing in size. Thus, it is obvious that this bone structure can not only adapt to functional conditions, but also change its shape, increasing in its geometric parameters. Consequently, the previously determined dimensional stability is very, very relative. As the first occlusal guideline, the doctor can use the position of the condyle during the registration of the centric relation, which is the most desirable. Firstly, the central ratio is a parameter that, with adequate execution technique, can be quite accurately and easily recorded. In addition, this position of the structures is repeatable, and it can be restored even if the position of the teeth changes or the contact between them is disrupted. A stable joint in this position has the ability to withstand significant loads, and the lateral pterygoid muscle can remain in a passive state even with strong clenching of the jaws (photo 2, 3).
Photo 2. Muscles that lift the mandible on the right side.
Photo 3. Muscles that lift the mandible on the left side.
Anatomy of the masticatory muscles
The function of raising the lower jaw is provided by three masticatory muscles. With parafunctional habits, such as bruxism, these masticatory muscles can develop significant force acting on all structures of the dentofacial apparatus. The masticatory muscle starts from the zygomatic arch and is attached to the lower edge of the lower jaw. The force vector of this muscle is directed upward and forward. The cross-sectional thickness of the masticatory muscles justifies the fact why they can develop the most significant strength indicators, located anterior to the temporomandibular joint. The temporalis muscle begins in the area of the temporal fossa and the deep part of the temporalis fascia. It is directed medial to the zygomatic bone and forms a tendon that is attached to the coronoid process of the mandible, and also passes into the region of the retromolar fossa distal to the last molar of the mandible. Since the muscle splits along its course, the action vectors of its force also diverge: the anterior component is directed upward and slightly anteriorly, while the posterior component is directed upward and posteriorly. This feature should be taken into account when diagnosing pain symptoms arising in the area of this particular muscle.
The medial pterygoid muscle consists of two heads: the main part of the muscle begins directly above the medial surface of the lateral pterygoid plate, while the superficial head begins from the maxillary tubercle and the pyramidal process of the palatine bone. The fibers of this muscle are directed downward laterally and posteriorly, and through the tendon are woven into the lower and posterior parts of the medial surface of the angle and ramus of the mandible. Insertable fibers connect this muscle with the masseter, forming common tendon slings, which allows both muscles to jointly perform the function of raising the mandible.
All of the above anatomical factors determine the direction vector of forces when activating the above-mentioned muscles. First, the directions of force of all three muscles shape the position of the condyle in the glenoid fossa: anteriorly and superiorly opposite the eminence and slightly medially, so that the medial pole of the condyle is the most load-bearing side of the joint. In other words, if we exclude the action of interdental contacts, then it is these muscles that determine the most superior position of the condyle, thereby ensuring close contact between the condyle, disc and glenoid fossa. The digastric muscle is one of the main muscles that lowers the lower jaw and opens the mouth. It begins in the area of the mastoid notch, forms a tendon along its path, and ends at the lower border of the mandible near the symphysis on the side of the digastric fossa. Since this muscle lowers the jaw, pain in this area is a rather unusual symptom. The lateral pterygoid muscle moves the lower jaw laterally and also forward. The upper head of this muscle starts from the infratemporal wing of the sphenoid bone, and the lower head starts from the lateral pterygoid plate. The muscle is woven in two bundles into the neck of the condylar process and the articular disc. Part of its function is to coordinate the position of the disc relative to the condyle to maintain the desired functional relationship, but in addition it provides support for the mandible in an eccentric position during intense clenching or bruxing when appropriate jaw movement is required to achieve maximum intercuspidation at existing tooth contacts . The three main levator muscles produce much more force than the lateral pterygoid muscle, therefore it must provide sufficient contraction to counteract the aforementioned elevator muscles. If these parameters do not correspond, painful sensations and even spasms may occur, which indicate a violation of muscle function.
Posterior teeth relationship
Pankey's first rule states that by positioning both condyles in centric relation, the posterior teeth form simultaneous and uniform contact, while the anterior teeth contact either slightly less or to a similar degree (Plates 4, 5).
Photo 4. Teeth contacts on the upper jaw.
Photo 5. Teeth contacts on the lower jaw.
Essentially, every type of occlusal design, regardless of condylar position, involves achieving multiple tooth contacts. With this ratio, the bite force is distributed more evenly over a larger number of tooth surfaces. In addition, maximal contact does not require activation of the lateral pterygoid muscles to maintain the mandible in the desired eccentric position. On the other hand, by ensuring simultaneous contact of the tooth cusps with flat bite pads, it is possible to guarantee the direction of the acting force down the long axis of the teeth, excluding the influence of deflecting lateral components (photo 6).
Photo 6. Areas of contact between the cusps.
It is the latter that provoke various structural damage to teeth, restorations, soft tissues and bone crest. And finally, with adequate contact of the posterior teeth, optimal distribution of the functional forces of the muscles that lift the mandible is ensured on both temporomandibular joints. When contact is ensured only in the area of the incisors, 60% of the total force generated by the muscles that lift the mandible is transferred to both joints, while with contact of the second molars this figure decreases to 5%. Posterior tooth contact is especially critical for painful and unstable joints.
Functional system assessment
Assessment of the functional system is a stage of diagnosing all conditions of the functioning of the dentofacial apparatus in each individual patient. The beginning of this stage is an analysis of how the patient talks to the doctor, and the idea of this approach was first proposed by Bob Barkley and later improved by Pankey. Barkley came to the conclusion that it is best when any disorders in a patient are diagnosed not only by the treating team of doctors, but also by the patient himself during diagnostic procedures. Therefore, a history review is a key initial aspect of treatment. A thorough and comprehensive patient examination algorithm was precisely described by William Lockard in his book “The Exceptional Dental Practice”.
Assessment of the functional state of the dental system includes diagnostics:
- temporomandibular joints
- masticatory muscles
- range and pattern of movements of the lower jaw
- analysis of static and dynamic tooth contacts.
The overall goal of a functional examination is to collect as much data as possible in order to determine whether the patient’s dental condition is stable or not. If the system is unstable, the doctor needs to determine where the structural damage occurred, what pathology could provoke it, and what type of dysfunction arose as a result. It is extremely important to consider all possible influencing factors before making a final diagnosis. Sometimes it happens that certain violations of functional parameters can be identified only at the end of the diagnostic process, or even between patient visits, based on his own complaints and comments that arose during a comprehensive examination. The order of diagnostic manipulations is determined by the attending physician himself, therefore the author developed the algorithm presented in the article himself, based on existing clinical experience. The first stage of diagnosis remains the assessment of joint function.
This step involves obtaining answers to the following questions:
- Do you feel pain when palpating your joints? If so, what is the nature of these sensations and how strong are they?
- Do you feel noises when moving your joints? If so, at what point in the movement and what is the nature of the sound? Is it painful?
- Is the movement of the lower jaw free and unrestricted? Are there any deviations? If so, how significant are they and in what direction are they observed?
- Can the joints withstand the forces or loads placed on them?
Positioning at the 12 o'clock position allows the doctor to examine the patient along the long axis of the head and at the same time analyze the existing deviations in movements and symmetrical relationships. In adult patients, full mouth opening exceeds 40 mm, and in some patients this parameter even goes beyond 50 mm. The lateral movement of the lower jaw is normally about 10 mm. In this case, the doctor must determine whether pain occurs during lateral movements? Do the ranges of lateral motion differ in any particular direction? The nature of the movements of the lower jaw is determined simultaneously by the state of the condylar process, disc, articular fossa and tubercle, as well as the stability of the lateral pterygoid muscles and the muscles that provide mouth opening. It is logical that movements in a damaged or unstable joint will be more limited than movements in a healthy state of the dental system. Therefore, assessment of the initial parameters of movements in the joint is a mandatory stage of a complex diagnostic algorithm. In addition, it is very important to record the position of the joint in the centric relation position. The author uses the bimanual centric relation technique developed by Dawson, as well as a leaf calibrator, a luchiu jig, and various types of frontal stoppers. The lack of contact in the area of the posterior teeth allows the muscles that elevate the mandible to position the condylar head more highly before the disc-fossa complex of the joint limits its position. The use of front stoppers is a fairly reliable method for recording centric relation. The patient is asked to stick the lower jaw forward and repeat this several times in the position of the frontal stopper - in this way it is possible to achieve activation of the muscles that understand the lower jaw. Initial attempts to determine the centric relation may be unsuccessful due to disc impairment, or fluid swelling within the joint capsule, not to mention possible spasms of the lateral pterygoid muscles. In such cases, the doctor will be able to determine only a preliminary central ratio. As the joints and muscles stabilize, more accurate centric relation parameters can be determined. Using the same three recording methods above, the doctor can also test the ability of the joints to tolerate force applied to them. In other words, the physician can determine whether the present condyle/disc/fossa condition is stable and healthy enough to withstand the forces of normal functional loading or even parafunctional conditions? In most cases, joint instability is caused by disorders such as inflammation, disc lesions, disturbances between the constituent surfaces, and pain in the area of attachment of the lateral pterygoid muscle to the condyle and disc. By repeated protrusive and retrusive movements of the patient using a sheet calibrator and a Lucia Jig, the condition of the joint and the lateral pterygoid muscle can be diagnosed. Adaptation to stress is tested using a bimanual technique, increasing the upward pressure force. After diagnosing the joint, they begin to evaluate muscle function. This part of the inspection is to determine the following:
- condition of the three muscles that lift the mandible. Is there any discomfort during palpation? What is the approximate cross-sectional thickness of the muscle? What level of tension is present when they are active? How does the patient react to palpation performed by the doctor?
- condition of the lateral pterygoid muscles. Does pain occur with palpation or the action of any other factor?
- condition of the muscles of the floor of the mouth.
- condition of the muscles in the neck and shoulders.
Palpation of each of these muscles is slightly different, but the doctor should palpate as many of them as possible. The physician should increase the pressure gently and slowly while observing the patient's response while rating their pain response on a scale of 1-2-3 (mild to moderate to severe). In addition, the clinician should analyze the relative cross-sectional thickness of the masseter and temporalis muscles, as this parameter is a reliable indicator of the patient's ability to generate loads of a certain force during jaw clenching or towing. Based on existing observations, it is known that patients with a shallower mandibular angle tend to have thicker masticatory muscles, which in turn allows them to generate more force during function.
And finally, the doctor needs to determine the nature of tooth contacts at different jaw ratios for a final understanding of the patient’s functional state. First, the first contact at centric relation must be determined, which will be considered the critical cutoff point, even if the patient has not reached the stage of restoration of centric relation. For this manipulation, the author uses a bimanual technique and a sheet calibrator. In addition, for the same purpose, you can use the “luchiu jig”, deprogramming the patient’s masticatory muscles, and then proceed to the bimanual technique with a progressive increase in the thickness of the calibrator sheets: this is how it is possible to evaluate the upper movement of the condyle deep into the articular fossa, and as a result, the area of occurrence of the most early contact in the dental area. This manipulation helps the clinician form an idea of the need to correct the corresponding vertical and horizontal components in order to achieve maximum contact between the antagonist teeth. To perform such a correction, it may be necessary to use various treatment methods, while at the same time it is necessary to evaluate whether such an intervention will be so effective as to compensate for all the changes in the dentofacial apparatus expected during its implementation, or whether performing it as a whole will be considered inappropriate.
conclusions
Understanding the anatomy of the joints, muscles and dentition, as well as their relationship, helps the doctor to objectively assess the parameters of the bite and the function of the dentofacial apparatus. This knowledge determines the adequacy of the choice of one or another treatment approach, based on the specific clinical conditions of each individual patient. Determining the forces generated during function and parafunctional states is a key step in diagnosing and solving the main clinical problems associated with occlusion and its constituent components. The following article will examine the features of the relationship of the anterior teeth and the dynamics of the movement of the lower jaw in case of malocclusion and various dysfunctions, including pathological abrasion of teeth. In addition, the concepts of treatment planning based on changes in the patient’s appearance remain promising in the structure of algorithms for restoring articulatory patterns, while helping to reduce the destructive influence of excessive forces on the state of the entire functional system.
Source: stomatologclub.ru
Directions of movement of the lower jaw
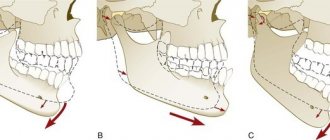
During the movement of the lower jaw, sagittal, vertical and transversal displacement of its heads occurs.
Vertical displacement is necessary to open and close the mouth. In this case, the movement, depending on the force, occurs with varying strength, which determines the degree of movement of the head.
The sagittal axis of displacement is the ability to move the lower jaw back and forth. In this case, the forward movement of the jaw and the biomechanism of the head of the articular part at the moment of movement is called the sagittal path of the joints.
Transverse is the ability of the jaw to move left or right. In this case, certain muscle groups move. For example, the direction of the masticatory apparatus to the right determines the left direction of the lateral muscles, and vice versa.
Without knowledge of how muscles and joints work, the dentist cannot regulate the normal functioning of the masticatory apparatus, which means he will not be able to manufacture and install suitable dentures and implants.
“Biomechanics of the lower jaw” Professor, Doctor of Medical Sciences Zhulev E.N. Lecture 3. – presentation
“Biomechanics of the lower jaw” Professor, Doctor of Medical Sciences Zhulev E.N. Lecture 3
Biomechanics is the science of human and animal movements from the point of view of the laws of mechanics.
Sagittal movements Angle of the sagittal incisive path (40-50 degrees) - - are carried out by bilateral contraction of the external pterygoid muscles. the angle of inclination of the palatal surfaces of the upper incisors to the occlusal plane;
The angle of the sagittal articular path (33-35 degrees) is the angle of inclination of the slope of the articular tubercle to the occlusal plane. the angle of inclination of the slope of the articular tubercle to the occlusal plane.
Bonneville's three-point contact - formed when the lower jaw moves forward, when the sagittal occlusal curve is well defined - contact of the anterior teeth and the distal cusps of the third molars.
Studying the relationship between the sagittal incisal path and the nature of the compensatory mechanism of dental occlusion, Bonneville derived the following laws: 1-the distance between the center of the articular heads and the medial angles of the mandibular incisors is equal to 10 cm - they form an equilateral triangle. 2-the severity of the cusps of the chewing teeth is directly dependent on the amount of overlap of the anterior teeth. 3-presence of a sagittal occlusal curve. 4-front teeth are located in a circle; and the side ones - in a straight line. 5-when the lower jaw moves, closure is achieved on the working side with like-named tubercles, and on the balancing side - with opposite ones.
Articulatory five of Hanau: - i.e. elements between which there is a natural connection under physiological conditions. 1-overlapping of the front teeth; 2-joint path; 3-height of the mounds; 4-sagittal compensation curve; 5-horizontal occlusal plane.
Transversal movements are provided by unilateral contraction of the external pterygoid muscle, when the head of the lower jaw on one side moves downward, forward and inward, forming an angle with the original direction - Benet's angle (15-17 degrees).
Transversal movements The curves of tooth movement to the right and left intersect, forming obtuse angles; the largest angle is formed when moving the incisors - degrees. (Gothic angle or transversal incisal path angle).
During lateral movements of the lower jaw, two sides are distinguished: - working - the teeth are set by the same tubercles; - balancing - the teeth are set with opposite cusps.
Temporomandibular joint A - upper joint space B - lower articular space C - articular tubercle D - articular capsule E - articular disc E - head of the mandible
Vertical movements The articular disc, attached along the periphery to the articular capsule, divides the joint space into two chambers - upper and lower. In the upper chamber, translational movements of the articular head are carried out due to the sliding of the disc along the slope of the articular tubercle. In the lower chamber there are only rotational movements of the articular head around the horizontal axis.
Gisi movement pattern: a – central occlusion; b – lowering and moving forward with a shift to the side; c – closure with the formation of the working and balancing sides; d – return to central occlusion.
Axis of rotation of the lower jaw
“Occlusal field” is a space within which a certain range or volume of movements of the lower jaw is limited by the need to obtain occlusal contacts.
Three-dimensional image of a complex of functional movements according to U. Posself
Complex of chewing movements according to U. Posself l-lV – phases of the chewing cycle, horizontal and vertical forms of the chewing cycle
Extraoral recording: lateral incisal path angle recording: sagittal articular path recording using facebow: sagittal incisal path recording
Intraoral recording - based on the Christensen phenomenon - a wedge-shaped gap formed between the bite ridges when the lower jaw moves forward.
Articulators 1 - anatomical articulators with an average setting of the inclination of the articular paths, incisal sliding and occlusal curves (Kantorovich, Monson, Bonneville, Gisi-Simplex, Sorokin). 2 - anatomical articulators with individual installation of articular paths (Walker, 1896; Christensen, Schwartz, Snow). 3 - Universal articulators - Ganau, Gizi-Turbayt, SIA - modern articulator Height. Occluders
Using a facebow
Chewing
TMJ functioning problems
| Click to sign up for a FREE consultation |
Disruption of the work and function of the joints and muscles of the lower jaw is called TMJ dysfunction. The pathology is caused by the occurrence of a defect in the teeth, increased wear and tear and an abnormal bite of a person.
The main clinical manifestation of dysfunction is clicking and clattering of teeth when opening the mouth. In more advanced cases, pain occurs in the ears, jaw, and painful sensations begin during chewing and yawning.
The main method for diagnosing TMJ dysfunction is radiography, which reveals dysfunction of the jaw and joint.
Treatment consists of a comprehensive effect on the condition of the jaw, which the dentist carries out based on knowledge of the biomechanics of its work.