04.01.2020
The operation to remove the nerve of a tooth is familiar to almost everyone who treated teeth in Soviet times or in the 90s. Not surprisingly, most people associate this procedure with arsenic being placed inside the tooth, followed by pain for several days. The memories are terrifying... But is it worth it to be afraid of this procedure now, when the modern industry has made a significant leap forward and modern dental services have appeared in all cities.
The first thing worth saying is that arsenic is a thing of the past. In addition, dentists use modern equipment and innovative materials, including for removing the nerve of a tooth. As a result, the process takes much less time, and the procedure itself is absolutely painless.
Removing the nerve allows you to protect other teeth and maxillofacial tissue from further development of the inflammatory process and the appearance of infectious diseases of the oral cavity.
First, we suggest you figure out what the nerve of a tooth is and when can a dentist decide to remove it?
What is a nerve and how many are there in a tooth?
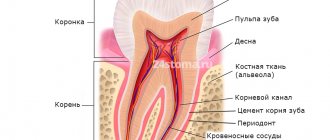
A tooth consists of several parts. Enamel is the top, most durable layer. It protects the underlying tissue - fairly dense but porous dentin. The infection slowly destroys it and spreads beyond the crown of the tooth, into the root canals. The first thing on the way is pulp. This is a neurovascular bundle consisting of a different number (from 1 to 3) of nerve endings and blood vessels. They are the ones who nourish the tooth, maintain its strong structure and vital functions. In addition, the pulp protects the connective tissues of the periodontium from infection and immediately reports it through pain and temperature sensitivity. When the nerve is removed, the tooth is left without nutrition and protection, and therefore becomes more fragile and susceptible to chipping. It is considered dead, although it retains its functionality.
Surgical method
The dentist’s task is to completely clean out the affected nerve from the canals when treating pulpitis.
In this case, treatment of pulpitis involves excision or complete removal of the affected pulp. Removing only the crown part will not work for teeth with one root due to the structure of the nerve. In addition, there are certain restrictions on the age of patients and the presence of allergic reactions.
If the pulp was partially removed, the doctor will also use medications to preserve the remaining part of the nerve.
With complete removal - under anesthesia or using a devitalizing paste - the nerve is completely removed from the tooth, including the root canals.
- Treatment of pulpitis in stages means that it is important for the doctor to remove the tissue completely to avoid recurrence of the infection.
- Afterwards, the canals and the tooth cavity are filled and everything is closed with a permanent filling.
After filling the canals, an x-ray must be taken to check the absence of voids; the cavities are etched and dried to ensure high-quality adhesion of the material to the tooth tissues and to prevent the filling from falling behind after hardening.
How to remove a nerve from a tooth
A couple of decades ago, the only way to remove a nerve from a tooth was with arsenic.
After treating the caries, it was applied to the exposed area of the pulp and a temporary filling was placed. You had to walk with arsenic paste on your tooth for several days for the nerve to die. The danger was that arsenic is a poison that affects the health of the entire body. And with prolonged contact with the tooth, it could be completely destroyed. Modern methods of treating pulpitis and removing the nerve are harmless.
The doctor makes an accurate diagnosis and determines the area of inflammation in the tooth. Then he injects an anesthetic to make the procedure painless. The specialist thoroughly cleans the root canals and removes affected tissue to prevent re-inflammation. If necessary, he applies arsenic-free medicine under a temporary filling, and then replaces it with a permanent one and takes a control photograph. Most often, tooth nerve removal takes place in one session, with a permanent filling immediately installed. It is impossible to carry out treatment without complete removal of the pulp (in adults), since its damage is an irreversible process.
Biological method using antibiotics
This requires high professionalism of the doctor to adequately assess the condition of the pulp. If the pathological process is at an initial stage and has not progressed to tissue destruction, then the doctor can use antibiotics to stop the inflammatory process.
- The tooth is prepared and the pulp chamber is opened;
- the doctor lays down the medicine;
- a microbandage with calcium hydroxide is installed;
- The tooth is filled with a temporary filling.
After the established period, the patient comes for a follow-up appointment. If the condition of the pulp has returned to normal, the filling is replaced with a permanent one.
Tooth hurts after nerve removal
After treatment and the end of anesthesia, the pulpless tooth may hurt. The reason may be temporary, since removal of the nerve is a serious intervention in the structure of the tooth. Usually, after a few days, all unpleasant symptoms disappear. If after two weeks the tooth continues to ache, and the pain even intensifies, consult your doctor immediately. Perhaps it’s all about the neighboring tooth, the pain from which radiates to the recently cured one.
Will my tooth hurt after pulpitis treatment?
The effect of the anesthetic drug wears off approximately 3 to 4 hours after the injection. The tooth sometimes begins to ache monotonously, and this pain can continue for some time. My tooth made itself felt for about two days. I stopped chewing on the left side of my jaw for several days to avoid getting hard food particles on the filled tooth, because at such moments the pain worsened significantly. These days I measured my body temperature, monitored my well-being, and was wary of complications.
My condition completely stabilized on the fourth day. I got used to the new filling, and the cured tooth stopped hurting. Now all I had to do was carefully monitor the health of my teeth and do everything to prevent deep inflammatory processes that lead to the removal of the nerve.
Surgery to remove a nerve frightens patients more with the unknown than it actually causes pain and discomfort. Toothache tends to be insidious and appear unnoticed, so I recommend everyone not to start inflammatory processes in the oral cavity, consult a dentist in time and not let the matter go to the point of removing the nerve. If indications for removal still appear, feel free to go to a professional and competent doctor. The doctor will select a good anesthetic for you, treat your aching tooth and relieve the pain forever.
Stages of treatment
Diagnostics. Before removing the nerve, the dentist takes x-rays. The image allows you to assess the condition, number and structure of the root canals, decide on the need to remove the nerve, and plan the procedure.
Anesthesia. For pain relief, conduction anesthesia is used (injection is performed). In case of severe inflammation and severe pain, local anesthesia at the injection site can be additionally used.
Preparation of the working field. After opening the hard tissues, the tooth must be protected from saliva containing bacteria getting inside. To do this, the working field is isolated with latex strips (cofferdam). During further treatment, this insulation protects the mucous membranes from heating by polymerization lamps.
Processing of hard tissues. Performed after injuries, carious lesions, destruction, etc. The damaged tissue is removed, and the dentist creates an opening in the tooth to access the pulp. During treatment, the tooth is cooled with an air-water mixture to prevent overheating of its tissues. After removing the affected tissue, the walls of the pulp chamber are treated in such a way as to increase the reliability of subsequent filling.
Nerve removal. Performed with a pulp extractor. This is a dental instrument that looks like a needle with small teeth. A pulp extractor is placed in the canal, the nerve is wound around it and removed. This is a disposable tool. In some cases, instruments for cutting pulp tissue can be used instead.
Root canal treatment. Measuring their length, cleaning, treating with an active antiseptic. Needed to remove residual pulp and other particles.
Installation of a temporary filling. Performed as an intermediate stage of treatment. A permanent filling is not placed immediately so that the dentist has the opportunity to check the condition of the root canals during the next visit, before permanent filling or crown installation.
Taking a control shot. It is necessary to make sure that the canals are properly processed and completely sealed.
What is a dental nerve?
The nerve of a tooth is a bundle of nerve endings that is located in the center of the tooth under the hard tissues of dentin and enamel. In medicine it is called pulp, and the process of removing the nerve is called depulpation.
The pulp performs a number of functions that are important for the growth and maintenance of dental health. It nourishes the hard tissues of the tooth, prevents the penetration of infections into the periodontium, and most importantly, is responsible for the sensitivity of the teeth when chewing. If the pulp is removed, the teeth require constant care, since adequate nutrition of the hard tissues is stopped. Therefore, the dentist, as a rule, decides on depulpation only if there are serious indications.
Symptoms of tooth pulpitis -
Pain with pulpitis can be of varying degrees of severity - from minor pain, which is provoked by thermal irritants, to acute paroxysmal spontaneous pain, which makes you want to climb the wall. Given the difference in symptoms, it is customary to distinguish 2 forms of this disease. Below we have described what pulpitis symptoms and treatment will have in each of these cases.
- Acute form of pulpitis – this form is characterized by acute paroxysmal pain that occurs especially at night.
It is typical that the pain increases, while pain-free intervals become shorter and shorter. As a rule, pain occurs spontaneously, i.e. without the participation, for example, of thermal stimuli. However, during the pain-free interval, in some cases it can be provoked by cold or hot water. With pulpitis, it is typical that after the removal of the irritant, the pain persists for about 10-15 minutes (this makes it possible to distinguish pain with pulpitis from pain with deep caries). With the latter, the pain stops immediately after the cessation of exposure to the stimulus. Very often, patients cannot even indicate which tooth exactly hurts, which is due to the irradiation of pain along the nerve trunks. The pain increases due to the gradual transition of inflammation from serous to purulent. With the development of purulent inflammation in the pulp, the pain becomes pulsating, shooting, and pain-free intervals almost completely disappear.
- Chronic form of pulpitis - in this form the inflammation is unexpressed. Patients usually complain of slight aching pain, most often arising from exposure to heat and cold irritants. Sometimes, by the way, with this form of pain there may be no pain at all. Keep in mind that the chronic form of pulpitis can periodically worsen, and during periods of exacerbation of inflammation, the symptoms will be exactly the same as in the acute form.
Why does deep caries develop?
The process of tooth decay under the influence of microorganisms and other factors is caries. Its onset and development is caused by the activity of pathogenic microflora of the oral cavity, in particular the bacteria Streptococcus mutans. They feed on sugars from food, cause fermentation and produce acid. It corrodes tooth tissue, which leads first to demineralization of the enamel, then to deformation of its structure and the formation of carious cavities. Gradually, the process spreads deeper and affects dentin - the bone tissue under the tooth enamel.
Caries most often does not develop at lightning speed and goes through several stages. First, a barely noticeable chalky spot forms on the enamel - an area that is different in color from the rest of the tooth. This is the area of demineralization where the carious process began. Enamel loses the mineral compounds that make up its structure, becomes more fragile and less resistant to harmful influences. This is the initial stage of caries - the spot stage. People often miss it due to the lack of obvious symptoms. Then tooth decay continues, and the disease progresses to the stage of superficial caries. The tooth begins to react to hot/cold, sour/sweet, and a clear defect is noticeable in the enamel.
Without treatment, superficial caries progresses to intermediate caries when dentin begins to deteriorate. Symptoms become more pronounced, pain occurs not only as a reaction to an irritant, but also on its own. According to statistics, most patients seek help from a dentist at the stage of average caries.
But there are also people whom even acute toothache will not force them to go to the dentist. And then the most complex and advanced form can develop - deep caries. At this stage, the carious cavity is in close proximity to the dental pulp; at any moment, inflammation can spread to the dental nerve and lead to pulpitis, and then to periodontitis.
Conservative treatment
The conservative method of treating inflammation is otherwise called biological and involves the preservation of nerve endings. Unfortunately, this option is only suitable for restoring a tooth at an early stage of pathology; in case of extensive tissue damage, more drastic methods will have to be used.
Conservative treatment is indicated for acute pulpitis, in cases where the chamber was opened due to negligence, as well as for the chronic course of a fibrotic disease.
This method also has a number of contraindications. The main ones are considered to be old age and the presence of serious inflammatory processes of the periodontium.
Also, this method of treatment will have to be abandoned if caries is detected in the neck or roots of the tooth, if prosthetics are needed in the future, if you are allergic to the materials used, as well as if existing diseases worsen at the time of treatment.