Neurologist (algologist)
Vasilenko
Marina Gennadievna
Experience 26 years
Head of the Pain Treatment Center, neurologist-algologist, member of the Society of Neurologists and Neurosurgeons, Russian Society for the Study of Pain, Association of Interdisciplinary Medicine, International Association for the Study of Pain (IASP)
Make an appointment
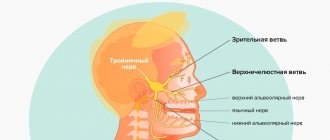
The trigeminal nerve is the largest of the 12 cranial nerves, specifically their fifth pair. It belongs to the nerves of a mixed type and includes very sensitive fibers. This name is due to the fact that the nerve is divided into three branches, providing mobility and sensitivity of the face, mucous membranes of the mouth and teeth. These are the ophthalmic, maxillary and mandibular branches.
Inflammation of the trigeminal nerve is a serious pathology that causes severe pain in the facial area. Otherwise it is called neuritis. In turn, neuralgia is pain along the trigeminal nerve. It can act as an independent sensitivity disorder, but it often accompanies inflammation, i.e. neuritis.
Symptoms and signs
Acute trigeminal neuralgia causes sudden and very severe pain along the nerve fiber. It manifests itself in attacks and is shooting and burning in nature. On average, the duration of an attack is up to 3 minutes; in approximately 7% of patients it lasts up to 3 days. Their number can reach 200 per day.
Pain from trigeminal neuralgia can be observed in different parts of the face. It all depends on which branch of the nerve was affected:
- if maxillary - in the area of the facial muscles, upper jaw and nose.
- mandibular – the pain will resemble a toothache.
- ophthalmic – in the area of the temples, forehead and above the eyebrows.
Against the background of pain, the patient develops increased anxiety and even phobias. A person strives to avoid those poses and movements that provoke unpleasant sensations in him. Other characteristic symptoms of inflammation of the trigeminal nerve:
- facial muscle spasms;
- increased salivation;
- increased or decreased sensitivity of facial skin;
- moderate increase in temperature;
- weakness and muscle pain.
Are you experiencing symptoms of trigeminal neuralgia?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Symptoms of neuralgia
- Facial pain (prosopalgia). A characteristic sign of neuralgia. Sharp and sudden, reminiscent of an electric shock. Usually lasts from 5 to 15 seconds, is paroxysmal in nature and can occur at any time. During periods of remission, the number of attacks decreases. Most often, pain occurs in the area of the cheekbones and lower jaw (both right and left), and can be localized in almost all areas of the face.
- Impaired sensitivity. A severe form of neuralgia can lead to partial or complete loss of sensitivity of the skin.
- Nervous tic of the eyelid (nystagmus), spasms and twitching of facial muscles.
- Loss of coordination and motor skills are rarer manifestations of severe forms of the disease.
- Headaches, fever, chills and weakness are syndromes caused by viruses and infections.
Causes and risk factors
Neuralgia of the trigeminal nerve branch is a disease with many possible causes. First of all, this is compression by vessels: displaced arteries or veins. Inflammation can also be provoked by metabolic disorders and diseases that are associated with them. These are diabetes mellitus, gout and other similar pathologies.
There are other possible causes of trigeminal neuralgia:
- inflammations that occur during dental treatment;
- hypothermia (general or facial area);
- mental disorders;
- purulent diseases of the jaw bones or skull;
- infection of the body with worms;
- chronic caries or sinusitis;
- infectious and viral diseases (herpes, adenoviruses, mumps, pulmonary tuberculosis, herpes zoster);
- very severe allergies;
- brain tumors;
- inflammation of the outer, middle or inner ear;
- multiple sclerosis;
- too narrow canal of the facial nerve from birth;
- injuries or operations on the temporal bone.
Causes
Facial neuritis occurs under the influence of the following etiological factors:
- in 15% of patients this is damage to the branches of the nerve during surgical interventions on the middle ear, mastoid process, and also associated with otitis media and other lesions of the hearing organ, for example, cholesteatoma;
- in rare cases, the disease is caused by infection - herpes virus (Hunt syndrome), mumps, polio, influenza, as well as Lyme disease, transmitted through tick bites;
- in 75% of cases, the cause of neuritis of the facial nerve cannot be determined; in this case, they speak of Bell's palsy, which worsens after hypothermia and colds.
Other causes include head trauma, surgery on the salivary gland, and removal of an acoustic neuroma.
Possible complications
Over time, symptoms of inflammation of the trigeminal nerve can give rise to neuropathic complications and lead to the development of secondary pain syndrome in the head. In the chronic form of the disease, the auditory and facial nerves are irritated. Without treatment, trigeminal neuralgia can lead to more serious complications:
- dystrophy of masticatory muscles;
- decreased sensitivity of the affected area;
- Sykinesia (cooperative movements in which one nerve controls many muscles);
- contracture and spontaneous contraction of the facial muscles;
- conjunctivitis.
Topical diagnosis
Topical diagnosis of NLN is based on its different structure at different levels, therefore, a change in the nerve proximal to the origin of a certain branch causes a loss of the corresponding function, and with a distal change, the function is preserved. This is the basis for the diagnosis of neuropathy along the canal of the facial nerve, where three branches depart from the nerve: the greater petrosal nerve, which supplies fibers to the lacrimal gland, the stapedius nerve, which innervates the stapedius muscle, and the chorda tympani, which provides taste innervation to the anterior 2/3 of the tongue. Determining the degree of neuropathy is based on identifying complete or partial loss of functions of the facial nerve and the dynamics of the development of symptoms.
Disturbances in the motor function of the nerve can be determined visually by facial asymmetry. With significant damage to the nerve, a picture of peripheral paralysis develops: the face is mask-like, the corner of the mouth is lowered, the palpebral fissure is open, the eyebrow is lowered, motionless.
To determine the autonomic function of the facial nerve, the functions of tear and salivation are examined. Tear production is examined using the Schirmer test (ribbons of filter or litmus paper are inserted into the lower fornix of the conjunctiva of the eye of the subject, resulting in lacrimation; the intensity of tear production is determined by the length of the wet paper in millimeters). Salivation is examined by radiometric determination of the concentration ability of the salivary glands and determination of the intensity of salivation by the amount of saliva received (while the patient under study is sucking a slice of lemon, saliva is collected separately for a minute from the pre-catheterized right and left parotid ducts). The study of taste sensitivity in the anterior 2/3 of the tongue is carried out using the method of chemical density testing, in which the thresholds of the main taste sensations (sweet, salty, sour and bitter) are determined by applying appropriate solutions to the tongue.
When to see a doctor
If you experience symptoms of trigeminal neuralgia, you should immediately consult a doctor, as it may be a sign of another serious disease. In the treatment of neurological pathologies, accurate and timely diagnosis is extremely important. This is done by a neurologist, with whom you can make an appointment at our clinic in the center of Moscow. The specialist knows not only how to relieve trigeminal neuralgia, but also how to correctly diagnose it in order to prescribe effective treatment in the future.
Differential diagnosis
Paralysis of facial muscles is not difficult to establish; it is more difficult to differentiate primary from secondary NLN. Combined neuropathy of the facial and other cranial nerves (impaired sensitivity in the face, weakness of masticatory muscles, noise in the ear, hearing loss, oculomotor and vestibular disorders), pyramidal and other conduction disorders indicate the secondary nature of the disease. In all cases of LPN, an otoneurological examination should be performed. Otitis is especially chronic and may be accompanied by NLN in the canal. Primary neuropathy may be indicated by the acute development of the disease, the connection of its occurrence with cooling - in some cases after a sore throat or flu. To identify early signs of contractures, a study of the state of electrical excitability of the facial nerve is performed.
It is important to differentiate idiopathic NLN from corticonuclear disorders and exclude secondary forms of facial neuropathy. Idiopathic LLN is usually unilateral. In most cases, the PMM is rough and equally expressed in all muscles. The absence of paresis of the orbicularis oculi and forehead muscles (or the obvious predominance of muscle weakness of the lower half of the face) suggests corticonuclear disorders, which are also accompanied by deviation of the tongue and, as a rule, more or less pronounced motor disturbances or increased reflexes and pyramidal signs in the ipsilateral limbs. The superciliary reflex does not disappear with central PMM. In addition, in the case of corticonuclear disorders, dissociation is possible between voluntary and emotionally regulated (smile, laugh, cry, etc.) contractions of the facial muscles. For example, with predominantly cortical disorders, the patient may have pronounced facial asymmetry with voluntary baring of teeth, while when laughing, the face is almost symmetrical (with deep subcortical lesions, the opposite situation is possible).
Partial PMM (eg, weakness of only the orbicularis oculi muscle or the buccal muscle) is uncommon in idiopathic LLN. Most of these cases are associated with tumors of the parotid gland (or other space-occupying processes in this area), causing compression of individual branches of the facial nerve.
Differential diagnosis for NLN should be made with Lyme disease and Melkersson–Rosenthal syndrome. Lyme disease is a common cause of LFN in endemic areas. Although NLN is one of the most common clinical manifestations of Lyme disease, it is rarely observed as the only manifestation of the disease; other symptoms (intoxication, skin rashes, joint changes) are more often present. Epidemiological history data are also important (stay in an endemic area, tick bite or the possibility of one). The diagnosis is confirmed using serological tests (enzyme immunoassay).
Melkersson–Rosenthal syndrome is a recurrent NPL (often with a change in the side of the lesion) in combination with a folded tongue, granulomatous cheilitis, swelling of the face and lips. The syndrome is caused by angiotrophic edema, which causes compression of the nerve in the canal. After each episode, there is a spontaneous, but usually incomplete restoration of the function of the facial muscles. Autosomal dominant inheritance is assumed.
Diagnosis of trigeminal neuralgia
A preliminary diagnosis can be made by a neurologist based on the patient’s complaints, studying the history of his disease and an objective examination of the face with an assessment of symmetry at rest and when trying to smile. Also, during the consultation, the doctor may conduct additional tests, asking the patient to close his eyes, purse his lips, frown, etc.
Laboratory and instrumental diagnostics of trigeminal neuralgia include the following examinations:
- general blood and urine tests;
- computed tomography (CT) and magnetic resonance imaging (MRI);
- radiography of the paranasal sinuses;
- panoramic radiography of the oral cavity;
- electroneuromyography to determine the localization of inflammation.
Symptoms
A common characteristic sign of the disease is immobilization and distortion of part of the face, in which it turns into a sedentary or completely motionless mask. Additional symptoms depend on where the inflammation occurs.
The facial nerve is a paired nerve; when it leaves the brain, it divides into two symmetrical branches. One of them is responsible for the innervation of the right side, and the other is responsible for the innervation of the left side of the face.
As a rule, inflammation affects only one of the two symmetrical parts, so the symptoms of neuritis are almost always unilateral. Contractions of the facial muscles become difficult or impossible, this manifests itself when trying to frown, smile, close an eye or raise an eyebrow. The face becomes distorted and asymmetrical.
The corner of the mouth and the edge of the eye are lowered, the nasolabial fold is smoothed out. When you try to close your eyelids, the eyeball turns upward (Bell's palsy). When you try to close your eyelids, a gap remains between them, this is called lagophthalmos or “hare's eye.”
Since the facial nerve consists primarily of motor fibers, inflammation of the facial nerve results in muscle symptoms. Sensitive, painful symptoms (in the form of neuralgia) are not typical for such neuritis.
However, the common nerve cord includes the intermedius nerve, which consists of sensory fibers and provides the sensation of taste to the outer two-thirds of the tongue, as well as the functioning of the salivary glands. Therefore, with neuritis of the facial nerve, symptoms such as disturbance, partial loss of taste, and increased salivation (drooling) are possible.
Another possible symptom is tear gland dysfunction, dry eye, or watery eyes. A combination of these two symptoms is possible - the so-called “crocodile tears”, when the eye becomes abundantly moisturized when eating, but remains dry the rest of the time (Bogorad syndrome).
Paresis or paralysis of the face usually develops within 24 hours after the appearance of pain behind the ear - the first sign of neuritis. As the disease progresses, symptoms such as hearing loss or intolerance to loud sounds (hyperacusis) are possible.
Ear pain with neuritis can radiate to the back of the head, temple, and be accompanied by loss of coordination, dizziness, and hearing loss. The complex of these symptoms is called Hunt syndrome.
Disruption of the innervation of the external eye muscle with neuritis of the facial nerve is manifested by convergent strabismus. Along with the characteristic signs of inflammatory damage to the facial nerve, symptoms of concomitant diseases may be observed, for example, shooting pain in the ear with otitis media. Or symptoms of cerebrovascular accident due to atherosclerosis.
From the point of view of Tibetan medicine, inflammation of the facial nerve, like other neuritis and neuropathies, refers to disorders of the governing basis Wind (Rlung - Tib.).
This is a light and cold base that has a great influence on other control systems of the body. Its disorder usually manifests itself not only with local symptoms (neuralgia, numbness, paresis, paralysis), but also with metabolic, immune, cardiovascular, respiratory, digestive, excretory, reproductive systems, as well as hormonal regulation.
Sanzhizhapova Avgustina Dondopovna Reflexologist, neurologist Experience 39 years
Treatment
Treatment of inflammation of the trigeminal nerve is carried out depending on the severity of symptoms. First, conservative therapy is prescribed. If this does not help, doctors resort to surgical methods. Their essence is to eliminate the cause of neuralgia. This may be compression of the nerve by the vessel. Surgical treatment is carried out using radiofrequency destruction, microvascular decompression or percutaneous surgery.
What drugs are most effective for the treatment of trigeminal neuralgia:
- antibiotics. Prescribed for infectious nature of the disease;
- glucocorticosteroids. Relieves severe inflammation in the body;
- non-steroidal anti-inflammatory drugs (NSAIDs). Helps suppress inflammatory processes;
- painkillers. Relieves soreness in the facial muscles;
- muscle relaxants.
To improve metabolic processes in the nervous tissue, the patient is prescribed B vitamins. How to relieve acute pain with trigeminal neuralgia:
- use anticonvulsants;
- provide physical rest, preferably bed rest;
- Apply an anti-inflammatory ointment or a warm compress to the site of pain.
Treatment for inflammation of the facial nerve
Drug treatment
Treatment of trigeminal neuritis is complex. The disease is first treated with medication - the patient is prescribed drugs that will alleviate the situation. These include painkillers, decongestants, vasodilators and B vitamins. Most often, the recommended medications are tablets, but you can speed up the recovery process by using ointments and gels. Sometimes doctors prescribe intramuscular injections.
In special cases, the recovery process of the facial nerve may be slowed down. Then the patient is prescribed glucocorticosteroids, which improve the metabolic processes of nervous tissue. Various biostimulants and hyaluronidases also contribute to a speedy recovery.
You cannot prescribe medications for yourself. Be sure to see a neurologist or neuropathologist at the first symptoms to determine the diagnosis and treatment strategy. Recovery medications are recommended to patients on a case-by-case basis, paying attention to the presence of chronic diseases, symptoms, and so on.
Surgery
Another way to treat the facial nerve is surgery. However, doctors turn to this option quite rarely - only when the trigeminal nerve is ruptured. Surgery is also required if there is no effect from the conservative method after six months or a year. Surgical intervention is only relevant during the first year of the presence of the disease; later, the muscles on the face irreversibly atrophy.
The surgical process involves suturing the damaged area of the facial nerve to restore its motor function.
Massage
The next treatment method is massage for the treatment of the facial nerve. The purpose of this method is to remove swelling, improve blood circulation, restore sensitivity and conduction of nerve impulses. Massage is contraindicated for tuberculosis, oncology, atherosclerosis and elevated temperature.
Initially, the massage therapist works only with the healthy side of the face, collar area, neck and area above the shoulders. Basically, the master uses rubbing, stroking, kneading and vibration.
For noticeable desired changes, it is necessary to conduct ten to twenty massage sessions from five to fifteen minutes. The duration is determined based on the degree of inflammation of the trigeminal nerve, the goals of therapy and the dynamics of recovery.
Physiotherapy
The next treatment method is physical therapy. It alleviates the severity of symptoms, helps to activate metabolic processes in tissues and restore the functions of the facial nerve.
Doctors prescribe this course of treatment from the first days of the onset of neuritis. The list of physical procedures includes:
- Ultrasound
- Laser irradiation of blood
- Electrophoresis of drugs
- Microwave therapy
- Exposure to ultra-high frequency electricity
- Ozocerite treatment
- Myoelectrostimulation
- Darsonvalization
This complex is indicated for the first week of treatment. Doctors prescribe it together with medication. This tandem helps speed up the process of restoration of the facial nerve. And its most important advantages are the absence of side effects and painlessness.
Alternative Methods
There are also alternative treatment methods. These are procedures aimed at restoring facial muscles and eliminating the symptoms of facial neuritis. Such procedures include:
- Clay or paraffin masks
- Acupuncture
- Reflexology
- Injections to eliminate muscle disorders
- Therapeutic baths
- Taping – stretching the face using adhesive plasters
- Immunosorption – purification of blood from antigens and antibodies
- Biofeedback – facial muscle training
Gymnastics for the face
Also, in conjunction with complex treatment, you can do facial exercises. Before this, you need to consult with a specialist; the doctor will draw up an individual list of exercises based on the severity of the process, location of the lesion and symptoms. Typically, such gymnastics takes about ten minutes a day.
A standard set of exercises includes relaxing and tensing individual facial muscles. For example, to restore articulation, it is recommended to pronounce the sounds “u”, “o”, “and”. Afterwards, you need to bring your lower lip under your upper teeth and reproduce the sounds “v” and “a”.
Gymnastics for inflammation of the trigeminal nerve:
- Close eyes
- Raise your eyebrows
- Frown
- Squint
- Smile with your mouth closed
- Smile with your mouth open
- Puff up your cheeks
- Pull them back
- Whistle
- Widen your nostrils
- Curl your lips
- Raise your upper lip and return to the starting position
- Lower your lower lip and return to the starting position
- Take water into your mouth
- Rinse your mouth
- Close your mouth
- Run the tip of your tongue along your gums
- Move your tongue right and left
Home remedies
Before treating trigeminal neuralgia at home, you should consult a doctor, since many remedies can only worsen the situation. If the specialist allows it, it is also possible to use various home recipes.
According to recommendations for trigeminal neuralgia, it is worth consuming orally or lubricating the affected side with birch sap. You need to drink 4-5 glasses per day. Heated buckwheat folded in cotton cloth will help relieve pain. The compress is made 2 times a day, keeping it at the site of inflammation until it cools down. At home, it is useful to massage the sore area: rub, stroke and lightly knead the area of inflammation.
Pain relief for occipital neuralgia
Damage to the nerve fibers of the cervical plexus - this disease occurs most often due to a complex of dystrophic disorders in the articular cartilage (cervical osteochondrosis). Shooting acute pain, manifested in paroxysms, goes from the neck to the back of the head. Thyme tincture helps to remove it. To do this, pour 50 g of thyme into 100 g of vodka and leave for 5 days. Take 15 drops of the prepared solution orally, after diluting it in 100 g of water, three times a day.
For external use, oil made from fir cones and young shoots is used. The oil is rubbed into the local area of pain using a gauze pad 6–8 times a day. For the same purposes, an infusion of marshmallow root is suitable, which is prepared as follows: 10 g of raw material is crushed and poured into 1 tbsp. warm water, then leave for 6–8 hours. Moisten a soft cloth with the decoction and apply it to the place where the pain is felt the most. A warming bandage is applied on top.
Myths and dangerous misconceptions in treatment
Due to the fact that neuralgia does not affect the general condition of the body, many patients postpone visiting a doctor and treating the trigeminal nerve. In fact, this is the wrong approach, since the disease can lead to paralysis and muscle paresis. In addition, it has a significant impact on psychological and social aspects of life.
No less important is the fact that painkillers for trigeminal neuralgia provide only a temporary effect. Over time, anticonvulsant medications may also stop working as they become addictive. Therefore, you should not abuse medications. They only relieve the symptoms of neuralgia, and its cause can only be identified by a qualified specialist.
Treatment of neuralgia
Treatment of neuralgia is a long and difficult process, but doctors at the CELT Pain Clinic know how to carry it out with maximum positive effect. For this, two treatment methods are used.
Conservative method of treating neuralgia
Conservative treatment involves taking medications:
- antispasmodics;
- anticonvulsants;
- non-steroidal anti-inflammatory drugs;
- glucocorticoids;
- anticholinesterase drugs;
- antidepressants;
- vitamins
It is very important to correctly calculate the dosage of medications (this is done by the doctor) and take them regularly (this is the patient’s function), since this is the only way to achieve the desired effect. In complex conservative therapy, physiotherapeutic methods of treatment - Bernard currents - help to achieve a good effect; acupuncture; paraffin applications, etc.
If conservative therapy does not bring the desired effect, the attending physician may decide on surgical treatment.
Surgical method for treating neuralgia
The following surgical treatment methods have proven themselves well:
- microvascular decompression of the root using implants that prevent compression on the nerve;
- radiofrequency destruction, which involves destruction of the nerve root;
- stereotactic radiosurgery (implies a targeted impact on the pathological focus with ionizing treatment using Gamma Knife and CyberKnife devices);
- balloon compression (carried out without violating the integrity of the skin) - a conductor with a balloon at the end is inserted into the area of the trigeminal nerve ganglion using a special needle. By inflating the balloon, the doctor compresses the nerve, which leads to its destruction and cessation of pain impulses.
In any case, the key to successful treatment is timely consultation with a doctor. Contact the CELT clinic, our specialists are always ready to help and relieve you of pain!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Prevention
There is no specific prevention against neuralgia. Doctors only recommend eliminating as much as possible exposure to the body of those risk factors that can lead to nerve inflammation. To avoid this, it is necessary to prevent hypothermia of the face, especially in the summer when using fans and air conditioners. It is important to harden yourself and worry less in order to reduce the impact of stress. It is also imperative to treat underlying diseases that are risk factors for neuralgia.
Possible causes of inflammation
- Hypothermia. The disease can be caused by prolonged exposure to the cold.
- Presence of facial injuries. The inflammatory process can occur as a result of bruises and blows. A special risk group includes people who have suffered traumatic brain injuries.
- Presence of head pathologies. This could be oncology, benign tumors or vascular aneurysm.
- Viral and infectious diseases. These include pulpitis, meningitis, herpes zoster, periodontitis, chronic caries and others. The cause of inflammation can also be a progressive herpes virus.
- Mental disorders, endocrine diseases, immune problems and chronic allergies.
Modern approach to the treatment of trigeminal neuralgia
Trigeminal neuralgia (TN) (synonyms: tic douloureux, or Fothergill's disease) is one of the most common facial pain (prosopalgia) and is one of the most persistent pain syndromes in clinical neurology [1]. TN is a typical example of neuropathic pain (NP) of a paroxysmal nature and is considered the most painful type of prosopalgia. TN most often has a chronic or recurrent course, is accompanied by a large number of comorbid disorders, is much more difficult to treat than many other types of chronic pain and leads to temporary or permanent disability, which makes it a major economic and social problem [2]. Chronic NP has a significant negative impact on the quality of life of patients, causing sleep disturbances, increased anxiety, depression, and decreased daily activity [3]. The high intensity and persistence of TN, its special, often painful nature, and resistance to traditional methods of pain relief give this problem exceptional relevance. Trigeminal neuralgia is a disease characterized by the occurrence of paroxysmal, usually unilateral, short-term, acute, sharp, intense, electric shock-like pain in the area of innervation of one or more branches of the trigeminal nerve [4, 5]. Most often, the lesion occurs in the zone of the II and/or III branch and extremely rarely - in the I branch n. trigeminus [6].
According to WHO, the prevalence of TN is up to 30–50 patients per 100,000 population, and the incidence is 2–4 people per 100,000 population. TN is more common in women than in men, debuts in the fifth decade of life and in 60% of cases has a right-sided localization [7, 8].
According to the International Classification of Headache Disorders (2nd edition), proposed by the International Headache Society (2003), TN is divided into classical, caused by compression of the trigeminal root by tortuous or pathologically altered vessels, without signs of obvious neurological deficit, and symptomatic, caused by proven structural damage to the trigeminal nerve, different from vascular compression [9].
The most common cause of TN is compression of the proximal part of the trigeminal root within a few millimeters of the entrance of the root into the pons (the so-called “root entry zone”). In approximately 80% of cases, compression occurs by an arterial vessel (most often a pathologically tortuous loop of the superior cerebellar artery). This explains the fact that TN occurs in old and senile age and practically does not occur in children. In other cases, such compression is caused by an aneurysm of the basilar artery, space-occupying processes in the posterior cranial fossa, tumors of the cerebellopontine angle and multiple sclerosis plaques [1, 8, 10, 11].
At the extracranial level, the main factors leading to the occurrence of TN are: tunnel syndrome - compression in the bone canal through which the nerve passes (usually in the infraorbital foramen and mandible), associated with its congenital narrowness, the addition of vascular diseases in old age, as well as as a result of a chronic inflammatory process in adjacent areas (caries, sinusitis); local odontogenic or rhinogenic inflammatory processes. The development of TN can be provoked by infectious processes, neuroendocrine and allergic diseases, demyelination of the trigeminal nerve root in multiple sclerosis [7, 12].
Depending on the impact of the pathological process on the corresponding part of the trigeminal system, TN is divided into predominantly central and peripheral genesis. In the occurrence of TN of central origin, neuroendocrine, immunological and vascular factors play an important role, which lead to impaired reactivity of cortical-subcortical structures and the formation of a focus of pathological activity in the central nervous system. In the pathogenesis of peripheral TN, a large role is played by the compression factor, infections, injuries, allergic reactions, and odontogenic processes [7, 8, 12].
Despite the large number of literature reviews and meta-analyses that have appeared in recent years on the problem of treating NB [13], which includes TN, there is no consensus among researchers regarding the basic principles of drug therapy for this disease [14]. Treatment of neuropathic pain is still insufficiently effective: less than half of patients experience significant improvement as a result of pharmacological treatment [15, 16].
The problem of treating trigeminal neuralgia today remains not fully resolved, which is associated with the heterogeneity of this disease in terms of etiology, pathogenetic mechanisms and symptoms, as well as the low effectiveness of conventional analgesics and the development of pharmacoresistant forms of TN that require surgical treatment. In modern conditions, treatment tactics for this disease include medicinal and surgical methods.
The main directions of drug therapy are: eliminating the cause of TN, if it is known (treatment of diseased teeth, inflammatory processes in adjacent areas, etc.), and carrying out symptomatic treatment (relief of pain).
Pathogenetic treatment of patients with TN includes the use of drugs with neurometabolic, neurotrophic, antioxidant, and antihypoxic effects. In recent years, the high effectiveness of the use of metabolic drugs in the complex treatment of NB has been discovered [8, 17]. In the treatment of patients with TN, the high effectiveness of the metabolic drug Actovegin, a deproteinized derivative from the blood of young calves, has been shown. The main effect of this drug is to stabilize the energy potential of cells by increasing intracellular transport and utilization of glucose and oxygen. Actovegin also has an antihypoxic effect, being an indirect antioxidant. In addition, the effect of Actovegin is manifested by indirect vasoactive and rheological effects by increasing capillary blood flow, reducing peripheral vascular resistance and improving the perfusion of organs and tissues [17]. Such a wide spectrum of pharmacological action of Actovegin allows its use in the treatment of TN. During an attack, it is advisable to use Actovegin intravenously in a slow stream or drip for 10 days at a dose of 400–600 mg/day. In the interictal period, the drug is prescribed orally at a dose of 200 mg 3 times a day for 1–3 months [8]. The pathogenetic treatment of patients with TN includes the use of high doses of B vitamins as part of multicomponent preparations, which is due to their multimodal neurotropic effect (impact on metabolism, metabolism of mediators, transmission of excitation in the nervous system), as well as the ability to significantly improve nerve regeneration. In addition, B vitamins have analgesic activity. Such drugs, in particular, include Milgamma, Neuromultivit, Neurobion, containing a balanced combination of thiamine (B1), pyridoxine (B6), cyanocobalamin (B12). Vitamin B1 eliminates acidosis, which reduces the pain threshold; activates ion channels in neuronal membranes, improves endoneurial blood flow, increases the energy supply of neurons and supports axoplasmic transport of proteins. These effects of thiamine promote nerve fiber regeneration [18–20]. Vitamin B6, by activating the synthesis of the myelin sheath of nerve fiber and transport proteins in axons, accelerates the process of regeneration of peripheral nerves, thereby exhibiting a neurotropic effect. Restoration of the synthesis of a number of mediators (serotonin, norepinephrine, dopamine, gamma-aminobutyric acid (GABA) and activation of descending inhibitory serotonergic pathways included in the antinociceptive system leads to a decrease in pain sensitivity (antinociceptive effect of pyridoxine) [18, 21]. Vitamin B12 is involved in processes of regeneration of nervous tissue, activating the synthesis of lipoproteins necessary for the construction of cell membranes and the myelin sheath; reduces the release of excitatory neurotransmitters (glutamate); has an antianemic, hematopoietic and metabolic effect [18, 22]. For rapid relief of pain and pathogenetic neurotropic effects in TN, it is advisable use of the parenteral form of the drug Neurobion - a combined preparation of B vitamins containing the optimal amount of vitamin B12 in both ampoule and tablet form. Neurobion is used in a dose of 3 ml per day intramuscularly 2-3 times a week - 10 injections (for severe pain syndrome can be used daily in the same dosage for 10–15 days). Then, to enhance and prolong the therapeutic effect and prevent relapse of the disease, Neurobion is prescribed in tablet form at a dosage of 1 tablet orally 3 times a day for 1–2 months [8].
Anticonvulsants are also the drugs of choice for the treatment of TN, and carbamazepine was one of the first drugs officially registered for the treatment of this condition [24].
In the early 90s of the last century, a new generation of antiepileptic drugs appeared, and now anticonvulsants are usually divided into first and second generation drugs.
First generation anticonvulsants include phenytoin, phenobarbital, primidone, ethosuximide, carbamazepine, valproic acid, diazepam, lorazepam, clonazepam. First-generation drugs are practically not considered as the first line of treatment for NB (with the exception of carbamazepine for TN) due to the insufficient level of analgesic effect and the high risk of adverse reactions. The most common side effects of first-generation anticonvulsants include: central nervous system reactions (drowsiness, dizziness, ataxia, sedation or increased excitability, diplopia, dysarthria, cognitive impairment, memory and mood impairment), hematological disorders (agranulocytosis, aplastic anemia, thrombocytopenia, leukopenia), hepatotoxicity, decreased bone mineral density, skin rashes, gingival hyperplasia, gastrointestinal symptoms (vomiting, anorexia). Second generation anticonvulsants include pregabalin (Lyrica), gabapentin (Neurontin, Gabagamma, Tebantin), lamotrigine (Lamictal), oxcarbazepine (Trileptal), topiramate (Topamax), levetiracetam (Keppra), tiagabine (Gabitril), zonisamide (Zonegran), vigabatrin (Sabril), felbamate (Taloxa). These drugs have more favorable pharmacokinetic characteristics and safety profiles, as well as a low risk of drug interactions compared to first-generation anticonvulsants [24, 25].
The main mechanisms of action of 1st and 2nd generation anticonvulsants are presented in table [26].
The first anticonvulsant successfully used to treat TN was phenytoin (Difenin) [27]. Diphenin, a derivative of hydantoin, similar in chemical structure to barbituric acid, is contraindicated in severe diseases of the kidneys, liver, and heart failure.
According to the recommendations of the European Federation of Neurological Societies (2009), pharmacotherapy for TN is based primarily on the use of carbamazepine (Finlepsin, Tegretol) proposed by S. Blum in 1962 (200–1200 mg/day), which is the drug of first choice (level of evidence A) [27, 28]. The analgesic effect of this drug is mainly due to its ability to reduce the permeability to sodium of the membranes of neurons involved in nociceptive reactions. The following treatment regimen with carbamazepine is usually prescribed. In the first two days, the daily dose is 200 mg (1/2 tablet in the morning and evening), then within two days the daily dose is increased to 400 mg (morning and evening), and after that - to 600 mg (1 tablet in the morning, at lunchtime and in the evening). If the effect is insufficient, then the total amount of the drug per day can be increased to 800–1000 mg. In some patients with TN (about 15% of the population), carbamazepine does not have an analgesic effect, so in such cases another anticonvulsant, phenytoin, is used.
Three placebo-controlled studies conducted about 40 years ago, which included a total of 150 patients with TN, showed the effectiveness of carbamazepine on both the frequency and intensity of paroxysms [24]. A number of authors have shown that carbamazepine can reduce pain symptoms in approximately 70% of cases. [29]. However, the use of carbamazepine is limited by pharmacokinetic factors and occasional severe side effects (for example, Stevens-Johnson syndrome), especially in elderly patients.
Oxcarbazepine (Trileptal) is structurally similar to carbamazepine, but is much better tolerated by patients and has far fewer side effects. Typically, oxcarbazepine is used at the beginning of treatment for TN at a dose of 600–1800 mg/day (Evidence Level B) [30].
As additional therapy for TN, the effectiveness of lamotrigine (Lamictal) at a dose of 400 mg/day [31] and baclofen at a dose of 40–80 mg/day [32], which are second-line drugs, has been shown (level of evidence: C). Small open studies (class IV) indicate the effectiveness of clonazepam, valproate, and phenytoin [33, 34]. This therapy is most effective in the classical form of TN. For TN of peripheral origin, it is preferable to include non-narcotic analgesics in treatment regimens, and in the case of the development of chronic pain syndrome (more than three months), the prescription of antidepressants (amitriptyline) is indicated [7, 12].
Gabapentin (Neurontin) is the first drug in the world to be registered for the treatment of all types of neuropathic pain. Many studies have shown the effectiveness of gabapentin in patients with TN who do not respond to treatment with other drugs (carbamazepine, phenytoin, valproate, amitriptyline); in most cases, complete relief of pain was observed [35]. The therapeutic dose ranges from 1800 to 3600 mg/day. The drug is taken 3 times a day according to the following regimen: 1st week - 900 mg/day, 2nd week - 1800 mg/day, 3rd week - 2400 mg/day, 4th week - 3600 mg/day.
The results of an open-label, prospective, 12-month study of 53 patients with TN were recently published, evaluating the effectiveness of pregabalin (Lyrica) at a dose of 150–600 mg/day. Treatment with pregabalin resulted in pain relief or at least a 50% reduction in pain intensity in 25% and 49% of patients, respectively [36]. In another multicenter, prospective, 12-week study of 65 patients refractory to prior analgesic therapy, treatment with pregabalin at a mean dose of 196 mg/day (monotherapy subgroup) and 234 mg/day (polytherapy subgroup) resulted in a ≥50% reduction in pain intensity in on average in 60% of patients, and also reduced the severity of anxiety, depression and sleep disorders [37]. When treating TN, the initial dose of pregabalin can be 150 mg/day in 2 divided doses. Depending on the effect and tolerability, the dose can be increased to 300 mg/day after 3–7 days. If necessary, you can increase the dose to the maximum (600 mg/day) after a 7-day interval.
The use of levetiracetam (Keppra) in the treatment of TN was first reported in 2004 by KR Edwards et al. [38]. The mechanism of action of levetiracetam is unknown; There is evidence obtained from animal experiments that it is a selective blocker of N-type calcium channels [39]. The properties of this drug are particularly suitable for the treatment of TN patients with severe pain who require a rapid response to therapy. The pharmacokinetics of levetiracetam are linear and predictable; Plasma concentrations increase proportionally to the dose within the clinically reasonable range of 500 to 5000 mg [40]. Unlike other anticonvulsants, especially carbamazepine, the hepatic cytochrome P450 system is not involved in the metabolism of levetiracetam and the drug is excreted through the kidneys [41]. In addition, this drug is characterized by a favorable therapeutic index and has a small number of adverse side effects (which is the main problem when using drugs to treat TN) [42]. Commonly reported side effects of levetiracetam are asthenia, dizziness, drowsiness, headache and depression. A 10-week, prospective, open-label study showed that higher doses of levetiracetam, ranging from 3000–5000 mg/day (50–60 mg/kg/day), were required for the treatment of TN compared with the treatment of epilepsy, but did not caused significant side effects. This circumstance indicates the prospect of using this drug for the treatment of TN [43].
One domestic study reported positive results with a combination of carbamazepine and gabapentin [44].
Since the 1970s, antidepressants have been used to treat TN [45]. Currently, the effectiveness of the use of tricyclic antidepressants (TCAs) in the treatment of TN has been proven [46].
Until now, the selection of analgesic therapy for NB is more an art than a science, since the choice of drugs is carried out mainly empirically. There are often situations when the use of one drug is not effective enough and there is a need for a combination of drugs. Prescribing “rational polypharmacotherapy” (simultaneous use of drugs with neurotropic, neurometabolic and analgesic mechanisms of action) allows increasing the effectiveness of treatment with lower dosages of drugs and fewer side effects [47].
For patients suffering from unbearable pain for a long time, and if conservative therapy is ineffective in the case of classical TN, surgical treatment is recommended. The following approaches are currently used:
1) surgical microvascular decompression [48]; 2) stereotactic radiation therapy, gamma knife [49]; 3) percutaneous balloon microcompression [50]; 4) percutaneous glycerol rhizolysis [51]; 5) percutaneous radiofrequency treatment of the Gasserian node [52].
The most effective method of surgical treatment of TN is the P. Janetta method, which consists of placing a special gasket between the trigeminal nerve and the irritating vessel; in the long-term period, the effectiveness of treatment is 80% [53–55].
In conclusion, we note that the treatment of TN should be multidisciplinary in nature, and the choice of various treatment methods and the risks of possible complications should be discussed with the patient.
Literature
- Karlov V. A. Neurology of the face. M.: Medicine, 1991. 288 p.
- O'Connor AB Neuropathic pain: quality-of-life impact, costs and cost effectiveness of therapy // Pharmacoeconomics. 2009. Vol. 27, No. 2. P. 95–112.
- Jensen MP, Chodroff MJ, Dworkin RH The impact of neuropathic pain on health-related quality of life: review and implications // Neurology. 2007. Vol. 68. P. 1178–1182.
- Pain syndromes in neurological practice. Ed. A. M. Veina. M.: MEDpress-inform, 2001. 368 p.
- Love S., Coakham HB Trigeminal neuralgia: pathology and pathogenesis // Brain. 2001. Vol. 124, No. 12. P. 2347–2360.
- Turbina L. G., Gordeev S. A., Zusman A. A. Trigeminal neuralgia. Epidemiology, pathogenesis, clinic, diagnosis, treatment // Collection of works of the Moscow Regional Association of Neurologists “World Stroke Day in the Moscow Region October 29, 2009”: Collection. articles. M., 2009. pp. 65–70.
- Gritsai N. N., Kobzistaya N. A. Classical trigeminal neuralgia and odontogenic pain syndrome // News of medicine and formation. 2009. No. 299. pp. 23–25.
- Tovazhnyanskaya E. L. Trigeminal neuralgia: modern aspects of complex therapy // International. neurol. magazine 2010. No. 3 (33). pp. 141–145.
- International classification of headaches. 2nd edition. M.: GlaxoSmithKline Trading, 2003. 380 p.
- Kress B., Schindler M., Rasche D. MRI volumetry for the preoperative diagnosis of trigeminal neuralgia // Eur. Radiol. 2005. Vol. 15. P. 1344–1348.
- Rasche D., Kress B., Stippich C. et al. Volumetric measurement of the pontomesencephalic cistern in patients with trigeminal neuralgia and healthy controls // Neurosurgery. 2006. Vol. 59. P. 614–620.
- Stepanchenko A.V. Typical trigeminal neuralgia. M.: Publishing house. Group "VHM", 1994. 39 p.
- Saarto T., Wiffen PJ Antidepressants for neuropathic pain // Cochrane Database Syst. Rev. 2007. Vol. 4:CD005454.
- Chong MS, Bajwa ZH Diagnosis and treatment of neuropathic pain // J. Pain Symptom Manage. 2003. Bd. 25. (Suppl. 5). S. 4–11.
- Dworkin RH, Backonja M, Rowbotham MC et al. Advances in neuropathic pain: diagnosis, mechanism, and treatment recommendation // Arch. Neurol. 2003. Vol. 60. P. 1524–1534.
- Finnerup NB, Otto M, McQuay HJ et al. Algorithm for neuropathic pain treatment: an evidence based proposal // Pain. 2005. Vol. 118, No. 3. P. 289–305.
- Ametov A. S., Dadaeva E. E., Strokov I. A. et al. Actovegin in the treatment of diseases of the central and peripheral nervous system // Rus. honey. magazine 2007. T. 15, No. 24. pp. 1824–1827.
- Lutsky I. S., Lyutikova L. V., Lutsky E. I. B vitamins in neurological practice // International. neurol. magazine 2008. No. 2. pp. 89–93.
- Ba A. Metabolic and structural role of thiamine in nervous tissues // Cell. Mol. Neurobiol. 2008. Vol. 28. P. 923–931.
- Gibson GE, Blass JT Thiamin-dependent processes and treatment strategies in neurodegeneration // Antioxid. Redox Signal. 2007. Vol. 9. P. 1605–1619.
- Wilson RG, Davis RE Clinical chemistry of vitamin B6 // Adv. Clin. Chem. 1983. Vol. 23. P. 1–68.
- Solomon LR Disorders of cobalamin (vitamin B12) metabolism: emerging concept in pathophysiology, diagnosis and treatment // Blood Rev. 2007. Vol. 21. P. 113–130.
- Trigeminal neuralgia. Internet review // Int. neurol. magazine 2010. No. 2 (32). pp. 103–104.
- Wiffen PJ, McQuay HJ, Moore RA Carbamazepine for acute and chronic pain. Cochrane Database Syst. Rev. 2005. Vol. 3:CD005451.
- Richter RW, Portenoy R, Sharma U et al. Relief of diabetic peripheral neuropathy with pregabalin: a randomized placebo-controlled trial // J. Pain. 2005. Vol. 6. P. 253–260.
- Kukushkin M. L. Neurogenic (Neuropathic pain) // International. neurol. magazine 2007. No. 2 (12). pp. 141–145.
- Sindrup SH, Jensen TS Pharmacotherapy of trigeminal neuralgia // Clin. J. Pain. 2002. Vol. 18. P. 22–27.
- Jorns TP, Zakrzewska JM Evidence-based approach to the medical management of trigeminal neuralgia // Br. J. Neurosurg. 2007. Vol. 21. P. 253–61.
- Gronseth G., Cruccu G., Alksne J. et al. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies // Neurology. 2008. Vol. 71. P. 1183–1190.
- Jensen TS Anticonvulsants in neuropathic pain: rationale and clinical evidence // European Journal of Pain. 2002. Vol. 6 (Suppl. A). P. 61–68.
- Zakrzewska JM, Chaudhry Z., Nurmikko TJ et al. Lamotrigine (lamictal) in refractory trigeminal neuralgia: results from a double-blind placebo controlled crossover trial // Pain. 1997. Vol. 73. P. 223–230.
- Fromm GH, Terrence CF Comparison of L-baclofen and racemic baclofen in trigeminal neuralgia // Neurology. 1987. Vol. 37. P. 1725–1728.
- Kamchatov P.V. Neuropathic pain: problems and solutions // NeuroNEWS. 2009. No. 4. pp. 45–47.
- Attal N., Cruccu G., Haanpaa M. et al. EFNS guidelines on pharmacological treatment of neuropathic pain // European Journal of Neurology. 2006. Vol. 13. P. 1153–1169.
- Cheshire W. Defining the role for gabapentin in the treatment of trigeminal neuralgia: a retrospective study // J. Pain. 2002. Vol. 3. P. 137–142.
- Obermann M., Yoon MS, Sensen K. et al. Efficacy of pregabalin in the treatment of trigeminal neuralgia // Cephalalgia. 2008. Vol. 28. P. 174–181.
- Perez C., Navarro A., Saldana MT et al. Patient-reported outcomes in subjects with painful trigeminal neuralgia receiving pregabalin: evidence from medical practice in primary care settings // Cephalalgia. 2009. Vol. 29. P. 781–790.
- Edwards KR, O'Connor JT, Button J. Levetiracetam for the treatment of trigeminal neuralgia // Epilepsia. 2004. Vol. 45 (Suppl. 7). P. 306.
- Lukyanetz EA, Shkryl VM, Kostyuk PG Selective blockade of N-type calcium channels by levetiracetam // Epilepsia. 2002. Vol. 43. P. 9–18.
- Patsalos PN Pharmacokinetic profile of levetiracetam: towards ideal characteristics // Pharmacol. Ther. 2000. Vol. 85. P. 77–85.
- Brockmoller J., Thomsen T., Wittstock M. et al. Pharmacokinetics of levetiracetam in patients with moderate to severe liver cirrhosis (Child-Pugh classes A, B, and C): characterization by dynamic liver function tests // Clin. Pharmacol. Ther. 2005. Vol. 77. P. 529–541.
- Zakrzewska JM Consumer views on management of trigeminal neuralgia // Headache. 2001. Vol. 41. P. 369–376.
- Jorns TP, Johnston A., Zakrzewska JM Pilot study to evaluate the efficacy and tolerability of levetiracetam (Keppra®) in the treatment of patients with trigeminal neuralgia // European Journal of Neurology. 2009. Vol. 16. P. 740–744.
- Stepanchenko A.V., Sharov M.N. Use of gabapentin in the treatment of exacerbations of trigeminal neuralgia // Pain. 2005. T. 3, no. 8. pp. 58–61.
- Braune S. Evidence-based pharmacotherapy of neuropathic pain syndromes // MMW Fortschr. Med. 2004. Vol. 146, No. 50. P. 49–51.
- Cruccu G. Treatment of painful neuropathy // Curr. Opin. Neurol. 2007. Vol. 20, No. 5. P. 531–535.
- Hall GC, Carroll D., Parry D., McQuay HJ Epidemiology and treatment of neuropathic pain: The UK primary care perspective // Pain. 2006. Vol. 122. P. 156–162.
- Janetta P. Trigeminal neuralgia: treatment by microvascular decompression // Neurosurgery/Eds. Wilkins R., Regachary S. New York: McGrawy-Hill, 1996. P. 3961–3968.
- Perez C., Galvez R., Huelbes S. et al. Validity and reliability of the Spanish version of the DN4 (Douleur Neuropathique 4 questions) questionnaire for differential diagnosis of pain syndromes associated to a neuropathic or somatic component // Health Qual Life Outcomes. 2007. Vol. 5. P. 66.
- Mullan S., Lichtor T. Percutaneous microcompression of the trigeminal ganglion for trigeminal neuralgia // J. Neurosurg. 1983. Vol. 59. P. 1007–1012.
- Hakanson S. Trigeminal neuralgia treated by the injection of glycerol into the trigeminal cistern // Neurosurgery. 1981. Vol. 9. P. 638–646.
- Sweet WH, Wepsic JG Controlled thermocoagulation of trigeminal ganglion and root for differential destruction of pain fibers. Part I: trigeminal neuralgia // J. Neurosurg. 1974. Vol. 39. P. 143–156.
- Barker FG, Jannetta PJ, Bissonette DJ et al. The long-term outcome of microvascular decompression for trigeminal neuralgia // N. Engl. J. Med. 1996. Vol. 334. P. 1077–1083.
- Tyler-Kabara EC, Kassam AB, Horowitz MH et al. Predictors of outcome in surgically managed patients with typical and atypical trigeminal neuralgia: Comparison of results following microvascular decompression // J. Neurosurg. 2002. Vol. 96. P. 527–531.
- Jannetta PJ Microsurgical management of trigeminal neuralgia // Arch. Neurol. 1985. Vol. 42. P. 800.
S. A. Gordeev*, Doctor of Medical Sciences L. G. Turbina**, Doctor of Medical Sciences, Professor A. A. Zusman**, Candidate of Medical Sciences *First Moscow State Medical University named after. I. M. Sechenov, **MONIKI im. M. F. Vladimirsky, Moscow
Contact information for authors for correspondence