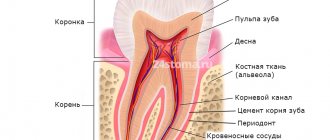
Chronic pulpitis is a form of pulpitis, inflammation of the pulp. Pulp is the soft tissue of the tooth, which is responsible for the blood supply to its hard tissues and consists of nerve endings, blood vessels and connective tissue. As a rule, chronic forms of pulpitis occur when acute forms are suppressed, but sometimes they can be a primary process without an acute stage.
Chronic pulpitis is an inflammatory process of the nerves and blood vessels of the tooth, which gradually causes severe changes in structure and function. If the disease is present, a person reacts sharply to cold and hot foods and experiences pain while chewing solid food. Pathology can be accurately determined using x-rays and electroodontodiagnosis. The development of the chronic form occurs in the absence of proper treatment of acute pulpitis.
Fact: the disease is much more often detected in the chronic form rather than in the acute form. People aged 20-50 years are at risk.
Filling made of light-curing material for classes I and V - 2,000 rubles.
Filling made of light-curing material in classes II, III, IV - 3,000 rubles.
Placing a temporary filling - 400 rubles.
Resection of the root apex (frontal group) - 6,500 rubles.
Resection of the root apex (chewing group) - RUB 9,000.
Mechanical and medicinal treatment of canals for periodontitis (1 canal) - 1,100 rubles.
Closing perforations (MTA) - RUB 6,500.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Causes of pulp inflammation
The main cause of pulpitis is the penetration of infection into the pulp cavity, in which a bundle of blood vessels and nerves is located.
The causative agents of the disease can be both pathogenic (Staphylococcus aureus) and conditionally pathogenic (lactobacillus) microorganisms. They can penetrate into the tooth in several ways:
- through the dentinal tubules in case of poor oral hygiene, accumulation of bacterial plaque and stone in the gum pockets;
- through cracks in the enamel caused by tooth trauma;
- through cracks due to a fracture of the dental crown;
- through the apical opening of the root canal against the background of periodontitis, osteitis and other chronic inflammatory processes of the oral cavity.
- Inflammation can also occur after treatment of deep caries
Recommendations after treatment
The only way to avoid relapse is to maintain proper oral hygiene and visit the dentist regularly. The appearance of pain in a tooth at rest or while eating is a good reason to visit a specialist, as this reflects an inflammatory process in the pulp. Professional cleaning of the oral cavity and visiting the dentist 2 times a year will help you prevent the recurrence of chronic pulpitis. If, after treatment from a specialist, you notice an acute reaction to cold and hot food, experience pain when pressing on your gums and teeth, or notice swelling and discoloration of the enamel, be sure to make an appointment with your doctor.
In the dental department of the CELT clinic, treatment of chronic forms of pulpitis is carried out using modern diagnostic equipment and high-quality filling materials.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Etiology of pulpitis
Based on etiology, which implies the nature of the inflammatory process, pulpitis is divided into three types. The classification is carried out depending on the nature of the irritant acting on the pulp:
- Infectious pulpitis develops in acute, but more often chronic diseases of the teeth and oral cavity (caries, osteomyelitis, periodontitis, etc.). In rare cases, the infection enters the root canal and pulp through the circulatory system from other units of the jaw or internal organs.
- Traumatic pulpitis develops when a tooth is damaged with the opening of a traumatic cavity (crack, chip) into the pulp. Occurs with sports injuries, crown and root fractures.
- Iatrogenic, that is, occurring after dental treatment . Occurs after treatment of deep caries, when the internal tissues of the teeth are irritated by the use of chemical, mechanical or thermal irritants.
Knowledge of the etiology helps the dentist select the most appropriate treatment methods and avoid complications in the future.
Possible complications of the disease
Unfortunately, even with severe symptoms of pulpitis, not all people rush to seek professional dental care. Patients who are afraid of the upcoming treatment of pulpitis endure pain for a long time and try to drown it out by taking pills and using a variety of traditional medicine recipes. However, it is worth remembering once and for all: all these measures are useless and will not help get rid of pulpitis, but they can lead to the development of serious and dangerous complications.
Most often, postponing the treatment of pulpitis “for later” leads to the development of periodontitis, a disease that affects the tissues around the tooth root. Periodontitis can be either acute or chronic. With an acute form of the disease, it will no longer be possible to avoid visiting the dentist: the pain becomes so severe that it is impossible to touch the tooth, the pain does not subside for a minute and the person can neither eat nor speak. Against the background of acute periodontitis, body temperature may rise and swelling of the gums may appear. When the canals are opened, a large amount of purulent fluid comes out of them.
The chronic form of periodontitis is characterized by the formation of fistulas that appear on the gums. Formations appear due to the formation of canals extending from the dental root of the tooth.
From time to time, purulent fluid also leaks from the fistulas, and at this point the pain may subside. Cysts can also form against the background of periodontitis. Granulomas appear at the root of the tooth and look like sacs filled with purulent fluid. The process of treating a cyst is quite complex, and it cannot always be carried out using conservative therapy methods.
However, these are not all the consequences that advanced pulpitis can lead to. If untreated, the disease can cause complications that affect the entire human body. It is worth talking about these complications of pulpitis in more detail, because all of them are quite capable of manifesting themselves if the symptoms of pulpitis are ignored and attempts to cure it on their own. Most often, periostitis occurs against the background of inflammation in the pulp.
With periostitis, inflammation occurs that affects the periosteum of the jaw and is accompanied by the rapid spread of pus through the tissues. A person’s general health deteriorates, a high temperature appears, the shape of the face changes, and a strong feeling of pressure occurs near the diseased tooth. Treatment for this disease requires surgery and can be so painful that it is often performed under general anesthesia.
Osteomyelitis, which can also be a complication of advanced pulpitis, is a purulent process that has developed to such an extent that the pathological phenomenon of bone tissue dissolution is observed. The disease causes loosening not only of the diseased tooth, but also of the healthy “neighbors” located next to it.
It is important to know: Osteomyelitis is a dangerous disease fraught with very serious consequences. If it has developed to a certain stage, then tooth extraction is required, which is very difficult. Osteomyelitis causes thinning of bone tissue and when trying to remove a dental unit, there is a high risk of a jaw fracture or part of it breaking off along with the diseased tooth.
Abscess and phlegmon are inflammations of a purulent nature, differing in the degree of spread. Both conditions are extremely dangerous as they can be fatal. When diseases appear, the infection begins to actively spread in the intermuscular space and affects blood vessels and nerves.
Sepsis is a condition characterized by infection in the blood fluid and its contamination with toxic substances. Sepsis often leads to death because the infection spreads through the blood extremely quickly.
These may be the consequences of pulpitis, which are worth knowing about and taking into account their possibility every time, for some reason, you are going to postpone a visit to the doctor. Remember, pulpitis can only be cured in the dentist’s office and there is no need to be afraid of pain: modern anesthetics completely eliminate any discomfort for the patient during treatment.
Symptoms
Inflammation of the pulp is not difficult to differentiate already at the stage of examining the oral cavity and interviewing the patient. This disease is characterized by:
- sudden onset of pain and its intensification at night;
- a gradual increase in pain intensity and duration in the first 3-5 days from the onset of the disease;
- irradiation (spread) of pain to the ear, eye, chin, depending on the location of the diseased tooth.
A characteristic feature of pulpitis, which makes it possible to distinguish it from caries and other dental pathologies, is a sporadic increase in pain, which is not associated with thermal, mechanical or other effects on the tooth.
Which teeth suffer from pulpitis more often?
Pulpitis can affect any unit in the oral cavity, but on some teeth the disease manifests itself more often. For example, the sixth or first molars are most at risk of developing pulpitis. These teeth are among the first to erupt and are located in an area that makes good hygiene difficult. Moreover, they have a unique structure, which makes it difficult to notice carious damage on them in a timely manner. People often do not notice spots of caries in deep fissures (pits) on the surfaces of the six, and this inattention is quite capable of leading to the gradual development of pulpitis.
If we talk about the front teeth, then the central and lateral incisors will be the most vulnerable to pulpitis.
Pulpitis on fangs is very rare; these teeth are massive and have a unique structure that does not allow caries to develop on them as actively as on other units.
The lower teeth are less susceptible to caries and pulpitis because the units in this area are constantly washed by saliva. Saliva contains useful components that strengthen tooth enamel and protect it from the action of pathogenic microorganisms. However, due to frequent washing of the lower teeth with saliva, another negative phenomenon occurs: hard plaque (tartar) quickly forms. Therefore, you should take care of your dental health equally and thoroughly clean and monitor the condition of all units in the oral cavity, regardless of their location.
Forms and types
The classification of pulp inflammation divides the disease into two forms according to the nature of the development of the pathology:
- Acute pulpitis is a first-time inflammatory process that lasts from 3 to 5 days and is accompanied by intense symptoms.
- Chronic pulpitis is a long-term inflammation that develops in the absence of treatment for acute pulpitis. Symptoms tend to periodically worsen, and in the intervals between them there is no discomfort or it is very mild.
Both forms have several subtypes, which differ in localization, degree of spread, and the nature of the development of the inflammatory process.
Types of acute pulpitis
There are four types of acute pulp inflammation:
- Focal pulpitis . It is diagnosed during primary inflammation, when the carious cavity reaches the pulp. The localization of the pathological focus is the upper part of the tooth. This type of disease is accompanied by the most intense symptoms and signs of inflammation spreading along the trigeminal nerve and nearby lymph nodes.
- Diffuse pulpitis . Diagnosed 1-2 days after the onset of acute inflammation. The lesion is located throughout the coronal part of the tooth, sometimes down to the neck and root part of the pulp. Attacks of pain last relatively short time and worsen when the patient lies down.
- Serous pulpitis . An advanced form of acute pulpitis, accompanied by painful pain symptoms that do not subside.
- Purulent pulpitis . The final stage of acute inflammation, in which a focus of suppuration forms in the pulp. The process is accompanied by signs of acute intoxication of the body, increased pain when eating warm and hot food. Symptoms weaken when cold is applied to the diseased tooth.
Classification of chronic pulpitis
Chronic pulpitis occurs in three types:
- Fibrous inflammation is the most common variant and lasts about 3 months after the initial inflammation. It is accompanied by bleeding of the pulp when touched, periodic pain in the tooth when it comes into contact with cold or hot food.
- Hypertrophic inflammation is a condition accompanied by the formation of a polyp inside the pulp. It looks like a piece of gum growing out of a tooth. Pain with this type of chronic pulpitis is minimal or absent.
- Gangrenous inflammation is the most dangerous pathological process, which is accompanied by active necrosis of tooth tissue. Accompanied by an unpleasant putrid odor from the mouth.
Good to know! In addition to the listed types of acute and chronic pulpitis, dentistry distinguishes deep root, two- and three-channel inflammation, as well as pulpitis under a filling.
Clinical manifestations
Treatment of chronic pulpitis does not always begin on time, since this disease is very insidious. Acute pain is always the reason for seeking professional help, but with chronic pulpitis, pain symptoms are not pronounced and the patient prefers to postpone his visit to the dentist. In this case, the disease develops quite quickly and, at best, will lead to an exacerbation of chronic pulpitis with severe pain symptoms or to the occurrence of periodontitis, in which it can be very difficult to save the tooth from removal. No less pleasant consequences may include the formation of cysts, ulcers, phlegmons and even sepsis. This is why timely diagnosis of chronic pulpitis is so important!
The main manifestation is an acute reaction to cold and hot food. However, it occurs late (sometimes 5-10 minutes after consuming food or liquid). In a calm state, a person experiences heaviness inside the tooth.
The hypertrophied form is not accompanied by severe pain. Overgrown tissue appears that ruptures when eating food. Pain may occur when eating hard foods or when pressing on the inflamed area.
Gangrenous pulpitis causes severe pain when eating hot food, which does not go away for a long time. The pulp begins to rot, which causes bad breath. The color of the tooth enamel changes (it becomes dark gray).
An exacerbation is accompanied by severe pain even without mechanical and thermal effects on the affected area. There are positive symptoms of vasoparesis, swelling of the gums, and pain in the trigeminal nerve.
Complications
In the absence of adequate treatment, pulp inflammation spreads beyond the boundaries of the root canal, to the periodontium and periosteum. In addition to the formation of a purulent focus (abscess) that opens onto the mucous membranes of the oral cavity next to the affected tooth, there is a possibility of developing more serious complications:
- flux or inflammation of the periosteum, which leads to the loss of a diseased tooth, and sometimes healthy teeth located nearby;
- osteomyelitis or purulent inflammation of the bone, which requires complex, expensive therapy;
- phlegmon - lesions of the soft tissues of the face, their “melting” with purulent exudate.
Each of these complications can, with a certain degree of probability, lead to life-threatening conditions, for example, sepsis.
Classification of dental pulpitis
Depending on the characteristics of the course, clinical signs and causes of the development of the pathological process, several forms or types of pulpitis are distinguished. In addition, some types of the disease have subtypes, which somewhat complicates the classification. But it is precisely thanks to an accurate understanding of the characteristics of the disease, as well as modern diagnostic methods, that the doctors at the Academy Dent clinic are able to select the most effective and correct treatment.
Acute pulpitis
The most common form of the pathological process is acute. This type of pulpitis develops quickly, has a clear clinical picture and occurs mainly in adults. In dental practice, there are 2 subtypes of acute pulpitis:
- Focal – considered the initial stage of the disease, which lasts from 1 to 2 days. The pathological process is characterized by the maximum proximity of the source of inflammation in that part of the pulp that is close to the carious formation on the tooth. Pain in this case is episodic, lasting no more than 30 minutes, after which it subsides for 1-2 hours and reappears.
- Diffuse is the stage subsequent to chaga, in which the inflammatory process covers the entire pulp core. The pain intensifies and can radiate to various parts of the jaw, as well as the temples, occipital region, and cheekbones. The duration of pain attacks increases and they become more frequent. The duration of this phase is measured for up to 2 weeks. If the disease is not cured during this time, pulpitis progresses to a chronic form.
Chronic pulpitis
Diagnosed after 2 weeks of the acute form of the disease. After 14-21 days, pain and other symptoms of the disease gradually weaken, but do not disappear completely. The tooth reacts sharply to external stimuli, and the pain intensifies. Periodic bleeding from the area of the pulp nucleus is added to the clinical picture, and the process of gradual destruction of the bone tissue of the affected unit of the dentition begins. The classification of chronic pulpitis is more extensive; it includes the following subtypes:
- Fibrous is the initial stage of the chronic form of the pathological process, in which it can occur covertly without causing discomfort to the patient. When examining the oral cavity, the doctor identifies an extensive carious cavity, although externally it may not be connected to the pulp chamber, which may result in incorrect treatment.
- Gangrenous is the next stage after fibrous, which is characterized by atrophy of nerve fibers, as well as a change in the color of the pulp nucleus to dark gray. The disease in this form is accompanied by increased pain in the tooth, and there is a pronounced foul odor from the oral cavity. Upon examination, the dentist reveals not only an extensive, but also a deep carious cavity.
- Hypertrophic is an even more severe form of chronic pulpitis, which is characterized by the formation and spread of granulation tissues with the subsequent formation of a polyp. The latter fills the space of the carious cavity and partially the root canal; when pressed, it responds with acute pain and the appearance of blood. If there is no impact on the tooth, the pain subsides.
- Acute – the last and most severe stage of the chronic form of pathology, in which the symptoms of acute and chronic pulpitis are combined. This stage is especially dangerous due to large-scale destruction of bone tissue and a high probability of periodontal infection, with the subsequent development of periodontitis.
Progression of the pathology to a chronic form (in any manifestation) in most cases threatens the impossibility of therapeutic treatment. The doctor has to remove the pulp core, and in case of large-scale destruction of bone tissue, the tooth itself.
Retrograde pulpitis
Retrograde pulpitis differs from the previously described forms in the cause of its occurrence. Infectious lesions of the pulp occur not from outside, but from within the body (for example, with the bloodstream with concomitant diseases). The main causes of retrograde pulpitis include:
- Periodontal diseases - in cases of progression of periodontitis, periodontal pockets form in the tissues of the oral cavity. In these cavities, which can reach half the length of the root part of the tooth in depth, pathogenic bacteria accumulate. These bacteria are able to penetrate into the cavity of the pulp nucleus through the holes at the apexes of the roots, provoking the development of an infectious process.
- Other pathologies - an infection from the bloodstream can penetrate into the pulp in diseases such as influenza, chickenpox, dental cyst, sinusitis, sepsis, etc.
In addition to the causes of development, the retrograde form of the pathology differs in its clinical picture. First of all, this is expressed in pain; pain is characterized by patients as pulsating, from acute to minor and periodic.
Treatment
To treat pulpitis, exclusively surgical methods are used - vital or devital removal of the pulp followed by filling the cavity. During vital removal, the doctor injects an anesthetic and removes the inflamed pulp tissue with a bur or mechanically. During devital removal, the pulp is first exposed to special drugs that kill the neurovascular bundle.
Important! Treatment of a tooth with pulpitis with arsenic is an outdated method that is used extremely rarely.
After careful mechanical treatment of part or all of the pulp, the doctor performs a filling in several stages: first, he isolates the root canals, then places a photopolymer filling in the tooth crown. If a significant part of the crown is destroyed, there is intense purulent and necrotic processes, the doctor may remove the tooth.
Types of chronic pulpitis
It is customary to distinguish the following types of chronic pulpitis:
- Hypertrophic – characterized by the formation of granulation tissue and dentin dystrophy. In this case, the overgrown granulations extend beyond the pulp chamber and enter the carious zone. If the form is polypous, then polyps are formed. Severe exacerbation can provoke pulp gangrene.
- Fibrous - differs from other types in that it leads to the appearance of coarse fibrous connective tissue. When examined, the pulp looks like a scar cord with a color change to white-gray. Gangrene, phlegmon and abscesses develop as complications.
- Gangrenous - represents complete tissue necrosis and tooth destruction (the color changes to gray-black). But in rare cases, it is possible to save small areas of the pulp.
Pulpitis of baby teeth
Pulpitis of baby teeth is dangerous because the pathological process from the affected tooth can move to the rudiments of permanent units. If the inflammation has not become irreversible, biological treatment is carried out. This gentle technique involves suppressing infection and the inflammatory process with maximum organ preservation of the pulp and neurovascular bundle.
Good to know! In case of pulpitis of primary teeth, it is extremely undesirable to remove the nerve from the tooth and fill the root canals, since this part of the teeth is not yet formed.
After using antiseptics and anti-inflammatory drugs, preparations with calcium hydroxide and calcium hydroxyapatite are placed into the pulp. These products will stimulate the formation of secondary dentin within a week. Only after this the doctor will place a permanent filling.
Symptoms that will help you diagnose pulpitis yourself
Knowing the main symptoms of the disease, it is quite possible to independently diagnose it in yourself and consult a doctor for therapeutic measures. Pulpitis has quite specific symptoms and differs from caries in that pain when the pulp chamber is damaged can occur without external irritants and spontaneously. With carious lesions, pain syndrome always appears against the background of external influences: for example, when eating, as a reaction to sour or sweet foods, to temperature stimuli. Moreover, when the provoking factor is eliminated, the pain quickly subsides (usually within ten minutes). If the factor is eliminated, but the pain does not go away, there is every reason to suspect pulpitis.
Pain with pulpitis usually occurs at night and is not as unbearable as with periodontitis.
Attacks of pulpitis pain can intensify and then disappear, while acute periodontitis is characterized by constant, severe pain, which interferes not only with eating, but even with speaking.
Different forms of pulpitis may have their own unique symptoms. For example, with prolonged attacks of aching pain, you can suspect the development of chronic pulpitis. Symptoms of the chronic form of the disease may be similar to those of chronic periodontitis, however, against their background, fistulas do not form, the gums do not hurt or swell.
When talking about the symptoms of pulpitis, it is important to make the following useful remark: any toothache is already a reason to see a doctor. Teeth don’t just hurt; there is always a reason that needs to be identified and eliminated. This approach will help you avoid complex dental treatment and associated costs and keep your teeth healthy and strong for many years.
Why diagnosis and treatment of chronic pulpitis is an urgent need
Toothache is a painful and extremely unpleasant phenomenon that comes unexpectedly and, as they say, at absolutely the wrong time. There are many reasons for its occurrence, but the most important thing is that if the symptoms appear, then they will not go away.
No matter how much is said about timely diagnosis and treatment, many still try to dampen the pain on their own, and only turn to the dentist when the pain becomes unbearable . This is why a disease such as chronic pulpitis is often encountered in dentistry.
Practice shows that it takes very little time for pulpitis to transition from the normal stage to the chronic stage - only two weeks .
Pulpitis itself is an inflammation of the pulp (neurovascular bundle) of the tooth, the main symptoms of which are acute pain that appears most often at night. It may go away and come back after a while.
In dental practice, approximately 15-20% of patients are diagnosed with this disease, and this, by the way, is almost every fifth.
Treatment of pulpitis
Pulpitis requires repeated visits to the dentist. Treatment of the initial stage of damage to incisors and canines takes 1–2 visits, more complex cases require 3–4 visits to the doctor. With serous pulpitis, complete recovery is possible with preservation of tissue viability. The first stage of therapy is opening the pulp chamber and removing carious areas. Further steps depend on the degree of tissue damage.
1. Conservative treatment
Drug therapy is recommended at the onset of the disease, if it is not aggravated by the inflammatory process. Antibiotics may be prescribed to stop the infection. At the next appointment, using an x-ray, they check whether the inflammation has been eliminated. If the dynamics are positive, a permanent filling is installed. Otherwise, more drastic measures are required: removal of the entire pulp. If you keep the pulp in the canals, the tooth will continue to be nourished and strengthened by dentin.
Devital extirpation
During the first appointment, the carious cavity is opened so that the doctor has access to the pulp. A devitalizing paste is placed there. Namely, today it continues to be briefly called “arsenic”. However, in fact it is a paste based on formaldehyde, resorcinol and paraformaldehyde. They are safe compared to arsenic compounds and are non-toxic. You can walk with a devitalizing paste, which is fixed with a temporary filling, for one week. Usually within 7 days it completely kills the pulp tissue. After the specified period, the dentist removes the paste; it cannot be left in the tooth cavity longer, otherwise it will poison the adjacent tissues, and the tooth will soon crumble.
At the next appointment, the doctor removes the pulp. Large, curved canals are carefully cleaned with special instruments. This procedure is called nerve ablation. Next, the empty canals are disinfected and filled with filling material. It is necessary to fill them completely, otherwise there is a risk of re-inflammation; for this, the doctor measures the length of the canal with apex locator electrodes. They are lowered into each channel, since their length can be different. The obtained data is compared with an x-ray.
The canal is treated, disinfected, and dried. Afterwards, the doctor fills it with special material. Our clinic uses the method of three-dimensional obturation of root canals with thermally modified gutta-percha. Gutta-percha pins are placed in the canals so that the sealer does not reach the upper hole by a few millimeters. Part of the pin is heated and removed. The dentist can monitor the process using x-rays.
When the canals are filled, the dentist again places a temporary filling. It is necessary for the gutta-percha to completely dry out and remove all moisture from it. This takes 4-5 days, after which you can install a permanent filling and restore the tooth.
The main disadvantage of devital extirpation is the duration of treatment, consisting of several visits to the doctor’s office:
- The first step is to open the pulp, remove carious lesions and apply a devitalizing paste.
- The second visit is to remove the nerve, clean the canals and fill them with gutta-percha.
- The final stage is filling and restoration of the tooth.
Causes
Treatment of the disease primarily depends on the causes of its occurrence. Factors that often lead to inflammation:
- Untreated caries in a timely manner. In a mild form, the disease does not affect the pulp in any way, since the carious lesion extends only to the superficial tissues. As the crown is destroyed, caries affects all cellular structures and reaches the roots.
- Chronic periodontitis (except for mild forms). Deep periodontal pockets that form with this pathology reach the root plexuses. Pathogenic microorganisms that multiply in these cavities spread throughout the tooth and reach the pulp.
- Injury. Impact, bruise and other external influences contribute to the disruption of the established blood supply process and lead to a pathological process.
- Poor quality dental treatment. If the dentist did not clean the tooth cavity well before placing the filling, leaving carious particles, they will spread into deeper layers and reach the neurovascular bundle. Also, due to the fault of the doctor, the patient may receive a thermal burn of the pulp if the specialist neglected the rules while drilling the crown and did not cool it enough with water. The disease is also provoked by overdrying of the dentinal tubules by air flow.
- Exposure to acids, alkalis, medications, toxic filling compounds and other chemicals.
- Blood infection. Infection can penetrate into the pulp not only through carious holes, but also during sepsis.
- The patient's individual predisposition to tooth wear and the formation of mineral deposits in the pulp chamber.
Types of pathology
There are 2 main forms of the disease: acute and chronic. In the first case, a person suddenly experiences a sharp, paroxysmal pain (most often at night), which does not depend on external factors and does not go away when the irritants are eliminated. At first, a dark hole appears on the enamel, which grows over time and affects deep tissues, including reaching the canals.
If the inflammation does not go away after 3 weeks, the disease becomes chronic. Dull aching pains appear with a certain frequency and are disturbing not only at night.
Types of acute pulpitis:
- Focal. It is observed only for a few days. The pain lasts up to 20 minutes, with the intervals between attacks being about 2-3 hours. There is swelling of the gums.
- Diffuse. It extends to the coronal part, nerve endings and root. There is a disruption in the blood supply to tissues. The pain becomes throbbing and lasts much longer than with the focal form.
- Purulent. The cavity of the affected unit fills with pus. A painful pulsation is felt. The patient's condition is constantly deteriorating.
- Serous. Most often, this type is observed in children (pulpitis of temporary teeth). This is a pathology of infectious etiology, which is accompanied by short attacks of pain.
Classification of chronic dental pulpitis:
- Fibrous. Is a consequence of acute. It can proceed latently for several months with periodic periods of exacerbation. The gums are not swollen, the pain is aching and occurs infrequently.
- Gangrenous. This is a complication of acute fibrotic disease, in which the death of pulp tissue and destruction of the coronal part occurs.
- Hypertrophic. In the carious cavity, tissues of a bright red hue are clearly visible, which constantly bleed, especially when pressed.
Symptoms
Despite the fact that each type of disease has its own distinctive features, there is a list of symptoms characteristic of all forms of pathology. At the initial stage of the disease, the tooth begins to react painfully to cold and hot, as well as to other irritants. Then a sharp throbbing pain appears, which intensifies at night and when lying down. Soreness occurs spontaneously or under the influence of irritating factors.
External manifestations of the disease, regardless of its type:
- darkening of the enamel;
- tooth mobility;
- bleeding;
- redness of the gums;
- swelling of the tissues around the diseased tooth;
The chronic form of pulpitis can be asymptomatic. It is characterized by a putrid odor from the mouth and aching pain.
Important! Very often the patient cannot understand which tooth hurts. The pain may radiate to the neck or ears. To determine the location of inflammation, a doctor’s examination and additional diagnostic tests are necessary.
Diagnostic methods
To make an accurate diagnosis, the dentist conducts and prescribes the following studies:
- inspection of the damaged cavity using a mirror and probe;
- checking the tooth’s reaction to temperature fluctuations (thermometry);
- exposure of the crown to a weak electric current (electroodontodiagnosis), with the help of which one can distinguish the disease from deep caries and determine in what form it occurs;
- X-ray.
Features of treatment
The therapeutic regimen directly depends on the stage of the disease and the location of inflammation. Treatment methods for pulpitis used in dentistry:
- Biological. Only the source of infection is eliminated, the progression of the disease is stopped, and the inflammation gradually goes away. Medicines are introduced into the cavity, which stop the growth and reproduction of pathogenic microflora and help eliminate inflammation.
- Conservative (vitalization). The doctor preserves the living pulp, but removes its coronal part. The tooth is completely preserved, while its functioning is restored.
- Devitalization. A special paste is placed into the drilled hole, which promotes the complete death of the pulp. The neurovascular bundle is removed, then the specialist places a temporary filling. When tissue inflammation completely disappears, the filling material is replaced with a permanent one. Devitalizing paste is used by pediatric dentists for tooth pulpitis in a child.
- Surgical. Surgical removal is divided into amputation (partial removal of pulp tissue) and extirpation (the pulp is completely removed).
Attention! The sooner the patient contacts the dentist, the higher the likelihood that the tooth can be saved. A qualified doctor will be able not only to cope with swelling and inflammation, but also to restore the integrity of the crown and restore the lost whiteness of the enamel.
Is it possible to cure a disease with folk remedies?
Pulpitis requires qualified medical care and cannot be treated on its own. Home methods for relieving pain and reducing inflammation can only temporarily alleviate the patient’s condition. Without timely conservative or surgical treatment, severe complications are possible.
Possible complications
If you do not receive treatment on time or do it incorrectly, the risk of complications increases, such as:
- periodontitis (damage to hard tissues around the tooth root with pulpitis);
- periostitis (inflammation of the periosteum, or flux);
- abscess (purulent inflammation accompanied by intoxication of the body);
- sepsis (blood poisoning);
- chronic pathologies of internal organs and systems.
Preventive measures
In order to avoid long-term treatment and surgical intervention, you need to take care of the prevention of pulpitis by adhering to the following rules:
- brush your teeth 2 times a day, rinse your mouth after eating, remove plaque and tartar in a timely manner;
- visit the dentist for preventive examinations at least once every six months;
- do not use toothpicks or other traumatic devices;
- eat a balanced diet, ensure that the body receives a sufficient amount of vitamins and minerals;
- give up bad habits (smoking, drinking alcohol), large amounts of sugar and junk food;
- treat caries and other dental pathologies in a timely manner, without bringing them to severe stages.
Sharp pain radiating to the neck, temples or ears is a reason to urgently visit a dental clinic. If treatment is not started in time, serious complications are possible, including complete tooth loss and a septic process.
By following preventive measures, you can protect yourself from the occurrence of pulpitis and other oral diseases.