What is submandibular lymphadenitis
Submandibular lymphadenitis is an inflammatory disease of the submandibular lymph nodes, which can take an acute and chronic course. Lymphadenitis of the submandibular lymph nodes is very often odontogenic (when the infection spreads from periodontal tissues (apical or marginal periodontitis), with pericoronaritis of the lower wisdom teeth, with suppuration of a radicular cyst, alveolitis). Also, the cause of an inflammatory process in the lymph node can be an infection in the tonsils, ear, throat and oral mucosa. Acute lymphadenitis can occur in serous and purulent forms.
Content:
- Causes of pathology
- Signs of inflammation of the submandibular lymph nodes 1.1. First stage 2.2. Second stage 2.3. Third stage
- How to cure an enlarged lymph node in the submandibular area
- Prevention of the inflammatory process
Inflammation of the submandibular lymph node is one of the most common types of lymphadenitis.
Its development is caused by inflammatory processes occurring in the oral cavity and less often in other parts of the body. Often the problem occurs with advanced caries, pulpitis, gingivitis, and inflammatory lesions of the tonsils. It is also caused by throat diseases. Let's take a closer look at why the submandibular lymph nodes are enlarged and what should be done to normalize the situation.
Prevention of submandibular lymphadenitis
Prevention of submandibular lymphadenitis involves taking measures to prevent the development of diseases that can cause an inflammatory process in the lymph nodes:
- During periods of acute respiratory infections epidemic, you should avoid crowded places and take all measures to prevent respiratory diseases.
- It is necessary to undergo a timely examination by a dentist and carry out all necessary treatment measures.
- It is necessary to properly and completely treat diseases of the nasopharynx, to prevent acute forms of ENT pathologies from becoming chronic.
Causes of pathology
If the lymph node changes its size, it can be assumed that a viral or bacteriological infection has spread. Taking into account the localization of the lesion, the doctor understands exactly where the source of the disease is located and which organs need urgent medical attention.
Among the dental provocateurs of enlarged submandibular lymph nodes:
- inflammation of the salivary glands;
- gingivitis;
- pulpitis;
- flux;
- stomatitis;
- alveolitis;
- periodontitis;
- deep caries;
- inflammation occurring under the crowns.
But the violation is not always associated specifically with dental diagnoses. Its reasons are:
- Respiratory diseases: pharyngitis, laryngitis, rhinitis.
- Pathologies related to the bone structures of the skull: damage to the bone structures of the lower jaw, damage to the temporomandibular joint, articular capsule.
- Infections: sore throat, measles, tonsillitis, otitis media, chicken pox, mumps. In all these cases, the lymphatic tissues swell a few days after the first symptoms of the disease appear.
- Specific pathologies caused by pathogenic pathogenic agents: toxoplasmosis, tuberculosis, syphilis, gonorrhea.
- Oncological neoplasms. Lymphatic tissue always reacts very sharply to tumor growth. Enlarged submandibular lymph nodes sometimes indicate the presence of a neoplasm in the area of the tongue, neck, or salivary glands.
- Autoimmune disorders. Always associated with disruptions in the functioning of the immune system. Then, by mistake, lymphocytes begin to treat healthy cells as dangerous pathogens. They destroy them, causing inflammation of the lymph nodes.
- Hyperthyroidism. With an exacerbation of this disease, the neck and cheek area swells, the lymph nodes become more voluminous.
In young children, parents may notice large round “balls” under the jaw during the period of active teething. This often causes an increase in body temperature. There is no need to be afraid of such symptoms. It is associated precisely with the inflammatory process provoked by the eruption of milk units. But, if the situation does not return to normal within three to five days, it is still worth showing the baby to a pediatric dentist, surgeon or pediatrician.
Why can a lymph node become inflamed after tooth extraction and what to do about it?
An enlarged lymph node signals the occurrence of an inflammatory process in the body. Typically, during inflammation, the lymph nodes increase in size and some pain appears. Swelling of the lymph nodes of the neck, head and lower jaw is associated with the development of inflammation in the area of the extracted tooth. In this article you will learn how to avoid complications and how to help the body cope with infections faster.
Lymph nodes and where they are located
Let's start with the lymphatic system. It is represented by a collection of vessels of various diameters that permeate our body. The lymphatic system is closely related to the circulatory system (this plays an important role in the development of complications). Lymph, the fluid that flows through the lymphatic vessels, transports tissue fluid and protein molecules. There are large numbers of lymphocytes and granulocytes - cells that are the first to fight pathogens. They are produced in the lymph nodes; when an inflammatory process occurs in the body, the lymph nodes work more intensely, increasing in size.
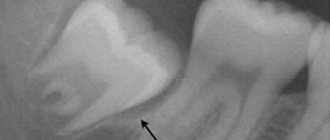
Photo 1 shows inflammation of the lymph node
But how does this relate to tooth extraction?
Most of the lymph nodes are concentrated in the head and neck area. Surprisingly, it is true: inflammation in the lymphatic system in 60% of cases occurs due to dental pathologies. The process of tooth extraction is a very traumatic event. In addition, a large number of opportunistic microorganisms live in the oral cavity.
Attention: Opportunistic pathogens are those that are normally present on the surface and inside the human body, but do not cause harm to it. However, when conditions change, they can become pathogenic and lead to the development of diseases.
So, bacteria entering the wound formed after tooth extraction can cause an infectious process. The nearby lymph nodes of the jaw, neck and head will react most quickly to it, actively producing cells of the immune system. Therefore, the patient can feel enlarged lymph nodes, which in some cases can be painful.
Why does the problem occur after tooth extraction?
After tooth extraction, in 99% of cases the lymph node swells. Dentists identify two main reasons:
1. This is a defensive reaction to interference, and it is the norm. As a rule, after tooth extraction, the lymph nodes in the neck or under the jaw become enlarged.
Attention: When wisdom teeth, or numbers of eights, are removed, the lymph nodes in the neck become enlarged. The procedure is quite traumatic and affects a large number of tissues, so in 90% of cases the lymph node becomes enlarged. It may also be accompanied by fever, soreness, inability to open the mouth wide, and general malaise.
- Tooth extraction was carried out against the background of an existing purulent-inflammatory process. In some cases, tooth extraction is a necessary step in solving advanced dental inflammatory diseases of the oral cavity, which include:
- fistula;
- periodontitis;
- flux;
- granuloma;
- cyst.
- In this case, the inflammatory process can result in a number of complications, so it is recommended to fight the infection with the help of antimicrobial drugs, rinsing with furatsilin or chlorhexidine, potassium permanganate or salt solution, as well as applying lotions.
Attention: Prevention is easier than cure!
Reasons for the development of lymphadenitis.
So, we have already found out that when teeth are removed, especially wisdom teeth, the lymph nodes become inflamed. This process is called lymphadenitis. The development of lymphadenitis in the head and neck area is promoted by:
- tonsillitis (inflammation of the tonsils);
- laryngitis (inflammation of the larynx);
- stomatitis (damage to the oral mucosa);
- gingivitis (inflammation of the gums).
What to do if the lymph node under the jaw is inflamed?
When the lymph node under the jaw becomes inflamed, the following symptoms occur:
- a significant increase in the size of the inflamed lymph node;
- when pressed, a dense movable tubercle is felt;
- severe pain in the gums and inflamed lymph nodes, which can spread to the head and neck;
- limited jaw movements;
- difficulty chewing and swallowing;
- general weakness, malaise;
- sleep disturbance;
- chills, increased body temperature up to 40 ◦C.
In such cases, the doctor identifies the degree of inflammation and prescribes appropriate treatment.
The dentist identifies the source of pathology by palpation (feeling with fingertips) of an enlarged lymph node, which is easily detectable. In some cases, pressure even causes pain. It is interesting that the skin first acquires a reddish tint due to increased blood flow in the area of inflammation, and then changes to bluish.
The body’s immune capabilities play a major role in activating the lymph nodes under the chin and in the lower jaw area. Lymphatic tissue, as the main part of the immune system, protects the body from pathogenic environmental factors. However, there are some diseases in which the immune system itself suffers. They are called autoimmune.
Such diseases include, for example, systemic lupus erythematosus, rheumatoid arthritis and serum sickness. With these pathologies, the protective function of the body is sharply reduced and, for example, if a child suffers from this serious illness, the lymph nodes under the lower jaw can increase even when baby teeth erupt.
What complications may arise?
Complications of an inflamed lymph node can be:
- angina;
In the photo on the left - healthy tonsils, in the photo on the right - inflammation of the tonsils
- laryngitis or pharyngitis;
The photo shows dental flux
- laryngitis or pharyngitis;
In the photo on the left - healthy tonsils, in the photo on the right - inflammation of the tonsils
The photo shows laryngitis
- otitis.
Otitis. The photo shows an inflammatory process in the ear
They occur when pathogenic microflora spreads to other nearby areas. There is no way around this without a course of antibiotic therapy. In order not to struggle with complications later, it is necessary to diagnose and properly treat inflammation in a timely manner.
Complications of extraction
A separate group of complications are those that arise during tooth extraction. There may be, for example,
- alveolitis;
- flux;
- abscess;
- phlegmon;
- osteomyelitis.
The most insidious of them is considered to be alveolitis, or inflammation of the socket of an extracted tooth. It develops due to a dentist’s mistake or when the patient’s postoperative regimen is violated. The cause of the development of alveolitis is the destruction of a blood clot that should form at the site of the extracted tooth. Without it, the hole becomes as if unprotected and pathogenic microorganisms enter it. This is how alveolitis develops.
The photo shows alveolitis (inflammation of the socket of an extracted tooth)
In addition, the tooth socket may begin to fester. Severe pain, swelling, uncharacteristic discharge and bad breath occur. It is necessary to treat the inflammation, since with its further progression, nearby tissues suffer: gums, periosteum, mucous membrane and others.
To treat alveolitis, you must immediately seek medical help. The dentist will clean the hole, removing all foreign elements, and treat it and other foci of infection that may also arise in the oral cavity with an antiseptic solution.
Dentists also consider dry socket to be a complication of extraction. As mentioned above, a blood clot must form, which will promote tissue restoration and wound healing. If the hole remains dry, then the risk of infection in the wound increases, the pain intensifies and an unpleasant taste appears.
With wisdom teeth, things are even more complicated - due to their distant location, the patient cannot always see that the blood clot has disappeared. Therefore, he seeks help only when pain develops. In the case of a dry socket, the doctor places a cotton swab on the wound, soaking it with antiseptics and an antibiotic solution. That is, a cotton swab literally replaces a blood clot. Thanks to this, the hole is protected and its regeneration is accelerated. The cotton swab must be changed every day until the hole is completely healed.
Treatment of lymphadenitis
Diagnostic measures aimed at eliminating the problem include:
- dental treatment
- drug therapy
- special regime.
1. Dental treatment involves getting rid of the causes that cause the lymph nodes to enlarge. The doctor may suggest:
- professional teeth cleaning;
- treatment or filling of root canals;
- sanitation of abscesses;
- cleaning the hole;
- resection of damaged parts of teeth;
- replacement of fillings and crowns.
Attention: After appropriate treatment, the lymph nodes do not return to normal immediately. Their increased size can last up to 2 weeks. If enlarged lymph nodes cause pain and discomfort to the patient, he may additionally be prescribed physical therapy, as well as choose medications.
2. Drug therapy consists of the dentist prescribing medications when inflammation is detected. Typically it is:
- antibiotics to eliminate pathogenic bacteria;
- immunostimulants and multivitamin preparations (to speed up the body’s recovery);
- home treatments in the form of lotions and rinses.
In case of fever, antipyretic drugs are prescribed, and in case of severe pain, which often accompanies dental surgery, analgesics are prescribed. Thus, etiotropic (antimicrobial drugs) and symptomatic (to relieve symptoms) therapy is carried out.
3. To speed up the relief of inflammation, the patient should follow a special regimen. These include:
- reduction of physical activity;
- in case of severe lymphadenitis, even bed rest is recommended; the need to drink up to 3 liters of warm liquid (herbal teas, fruit drinks and plain water help well - they help get rid of intoxication caused by inflammation as quickly as possible);
- rinsing (you can rinse your mouth with a decoction of chamomile or calendula);
- salt lotions (a concentrated salt solution is prepared, a large piece of cotton wool or a cotton pad is soaked in it, and it is placed behind the cheek where the dental procedure was performed. The hypertonic solution will help the cotton wool absorb metabolic products during inflammation).
Patients will have to make extensive adjustments to their teeth brushing. If there is inflammation in the oral cavity and, as a result, in nearby lymph nodes, it will not be enough to use only a brush and paste. It is recommended to use an irrigator and dental floss, and after all these procedures, use a mouth rinse.
Caution: Buy a paste that contains antiseptics such as chlorhexidine, chlorine, silver and zinc. It will provide you with additional sanitation of the operated area and will not allow inflammation to develop.
The basic principles that ensure effective treatment of inflamed lymph nodes are:
- good timely diagnosis;
- bed rest;
- the use of alternative medicine methods in the form of lotions and rinses;
- antibiotic therapy;
- adequate sanitation of the oral cavity.
Attention: Treatment of inflamed lymph nodes should not be delayed, as pathogenic organisms can enter the circulatory system, which will cause sepsis.
What medications are prescribed?
Often, antibiotic therapy for enlarged lymph nodes and inflammation includes penicillin antibiotics, for example, Amoxiclav, Ampicillin or Amoxicillin. In case of allergy to antibiotics of the penicillin group, antibiotics of other groups may be prescribed. The most effective of them are macrolides and fluoroquinolones.
Attention: The course of antibiotic therapy should not exceed 5, and in some cases – 7 days. Carefully read the instructions prescribed for this antibiotic and follow them! To avoid developing resistance, follow your doctor's recommendations.
Signs of inflammation of the submandibular lymph nodes
How the disorder manifests itself depends on how far the disease process has progressed. If you do not carry out the necessary therapeutic measures, one stage will quickly pass into another.
First stage
The size of the lymph nodes changes very slightly, but the person already feels that they hurt when pressed. Discomfort occurs when turning the head. Body temperature often rises and a sore throat appears. A tickle or dry, unproductive cough is annoying. Pain occurs only on one side of the neck or on both sides at once. The first case is more likely if it is a viral disease.
Second stage
It is called “acute lymphadenitis”. Now the lymph node can be distinguished visually - it becomes convex and protrudes forward. Externally it resembles a subcutaneous ball. Its diameter reaches three centimeters, but can be more impressive.
The node is painful to the touch. Because of this, it is difficult for the patient to turn and tilt his head, and open his mouth wide. The mobility of the upper and lower jaw is significantly limited.
The pain may radiate to the cheek or ear. Body temperature increases. Overall performance decreases.
Third stage
Called purulent lymphadenitis. Here, the inflammatory process even affects structures adjacent to the lymph node. The patient complains of pain in the throat, collarbone, armpit, and head. The nerve endings of the teeth may become inflamed. Then acute toothache occurs.
Pus formed in lymphoid tissues consists mainly of necrotic cells. If it gets into the blood (and such a possibility always exists), the outcome can be extremely unfavorable, so the inflammatory process should not be started.
Patients can understand that the submandibular lymph node is inflamed and needs treatment as soon as possible by the following signs:
- the “ball” enlarges and becomes red or bluish;
- every day it becomes more dense and solid;
- the skin located above the lymph node takes on a red tint and is hot to the touch;
- the lower jaw area swells.
Submandibular lymphadenitis in children
In children, submandibular lymphadenitis occurs less frequently than in adults. In children under three years of age, the disease cannot develop at all, which is due to the peculiarities of the formation of the lymphatic system.
Photo: submandibular lymphadenitis in a child
If a child is bothered by pain in the neck or jaw area, parents should carefully palpate the nodes. Healthy lymph nodes are quite soft and mobile, and the procedure itself is absolutely painless. If pain occurs or a lump is detected, you should immediately contact your pediatrician.
The main cause of inflammation of children's lymph nodes is diseases of the teeth, gums and infection in the nasopharynx. The doctor determines the treatment regimen for submandibular lymphadenitis in a child individually, taking into account the patient’s age and the admissibility of taking medications.
How to cure an enlarged lymph node in the submandibular area
Therapy must be carried out under medical supervision. Its main goal is to eliminate the infection that caused the disorder. If the root cause of the condition is not established, it will not be possible to be completely cured.
If the problem is related to an oral disease, mandatory treatment is carried out. For severe inflammatory pathologies of internal organs, antibiotic therapy is carried out. For pathologies of a viral nature, patients are prescribed antiviral drugs.
If the examination reveals that pus has accumulated inside the tissues, it is drained using a drainage tube. Additionally, a puncture is taken to recognize the pathogen and understand whether the disease has a benign or malignant course.
As soon as the infectious focus disappears, the lymph nodes begin to shrink, stop hurting and gradually reach their normal state.
Diagnosis of enlarged submandibular lymph node
As a rule, identifying the cause of the pathology is not difficult. In severe lymphadenitis, inflammation of the lymph nodes is distinguished from phlegmon and other similar diseases. In the case of chronic pathology, an immune puncture is performed.
The initial examination is carried out by a therapist, who, if necessary, refers the patient to a specialist (ENT specialist, dentist, oncologist, etc.). In addition to palpation, the following laboratory and instrumental examinations are performed:
- Ultrasound of the submandibular nodes and internal organs;
- chest x-ray;
- HIV test;
- magnetic resonance imaging;
- blood test for cancer markers;
- puncture of the lymph node under the jaw;
- bacteriological culture for the sensitivity of purulent flora to antibiotics;
- CT scan;
- clinical and biochemical blood tests.
Prevention of the inflammatory process
To reduce the risk of developing lymphadenitis, you must strictly follow the recommendations:
- Have annual preventive examinations at the dental clinic. Treat all emerging oral diseases in a timely manner. Avoid caries and take care of your gums.
- Do not ignore the presence of infections and treat them. During therapy, strictly follow all medical prescriptions.
- For any damage to the skin, treat wounds with antiseptics. This minimizes the risk of contracting an infectious disease.
- If you feel unwell, consult a doctor and get laboratory tests. This simple measure allows you to detect violations at the earliest stages.
It is necessary to understand that using “grandmother’s” methods for inflamed lymph nodes is dangerous. So, under no circumstances should you heat the inflamed area or apply cold compresses to it. It is unacceptable to massage him or put pressure on him. All of these actions can make the situation worse. Then it will be much more difficult to reverse the disease.