2511
Temporomandibular joint dysfunction is a rather complex condition that can be experienced by people of different ages and health conditions.
A large number of different symptoms, difficulties with chewing and opening the mouth are a serious reason to visit the dentist to determine whether a pathology of the lower jaw joint, such as Costen syndrome, is developing.
Description of the problem
Costen's syndrome was discovered in the thirties of the 20th century. Otolaryngologist D. Kosten compared cases of patients complaining of ear pain due to pathologies in the structure of the jaw system, and came to the conclusion that there is a relationship between these factors.
Pathological occlusion syndrome, as Costen's syndrome is otherwise called, is a functional disorder of the temporomandibular joint.
This pathology affects the cartilage disc, which provides joint mobility in three directions, due to which complete chewing of food is carried out.
An unevenly distributed load between the jaws leads to inflammation of the cartilage disc, which can lead to its degeneration if not treated in a timely manner.
As a result of this phenomenon, there is a decrease or complete loss of mobility of the mandibular joint.
Possible complications
If the patient neglects all the symptoms, suffers pain and delays treatment of Costen's syndrome, functional and physiological changes occur in the temporomandibular joint, salts are deposited in its area, fluid accumulates in the cavity due to inflammation, and the ligamentous apparatus is weakened. A person loses the ability to chew food normally due to pain, and has to eat soft foods. Because of this, the diet becomes quite meager, and problems with the gastrointestinal tract may occur.
In the future, complete immobilization of the jaw joints may occur, up to the inability to open the mouth, and significant deterioration in hearing and vision. The syndrome can indirectly damage other systems and organs.
Reasons for development
Dentists still have not agreed on what can trigger the development of the syndrome.
The most common factors contributing to the development of the disease are the following:
- incorrect design of the denture, causing uneven distribution of load during chewing;
- various jaw injuries;
- congenital or acquired pathological bite;
- excessively strong one-time or constant loads on the jaw joint;
- bruxism;
- collagen diseases.
The development of Costen syndrome can be caused by a combination of several factors or by one of the above reasons.
If you find any problems in the operation of the dentition, you should consult a dentist.
How can a pacifier affect a child’s bite, tips for selection and use.
Read here all the most important things about the small vestibule of the oral cavity.
At this address https://orto-info.ru/zubocheliustnye-anomalii/chelyustey/krivaya-ne-prigovor.html we will talk about methods for correcting a crooked jaw.
Causes of Costen syndrome
To date, the causes of this pathology remain unknown, but gnathologists are similar in their belief that the main prerequisites for the formation of Costen syndrome are:
- uneven load on the jaws when chewing, due to incorrect design of the denture;
- jaw injuries;
- malocclusions of various origins;
- too intense load on the jaw;
- bruxism – grinding of teeth during sleep;
- collagen diseases.
Risk factors
Dentists note that most often the development of Costen syndrome is observed in patients over 50 years of age. As a rule, the likelihood of its occurrence is higher in women than in men.
People who have a history of the following problems also fall into the risk category:
- injuries of the temporomandibular joints;
- unresolved violation of the structure of the dentofacial rows;
- absence of the last molars in each row;
- osteoarthritis.
Some dentists suggest that genetic predisposition can also become a factor in the development of pathology, however, this assumption has not been proven.
General prevention
In order to never encounter the syndrome, much less its complications, you need to avoid using chewing gum, as well as excessively frequent consumption of solid foods that are difficult to chew. It is also better to give up the habit of clenching your teeth during nervous tension.
It is necessary to solve problems with unhealthy teeth, their partial absence, and malocclusions in a timely manner. This should only be done by qualified personnel. Also, if possible, you should avoid injuries and inflammation of the jaw.
If chewing begins to cause discomfort or other signs of the syndrome appear, you should definitely consult a doctor. The earlier the diagnosis is made, the easier and more successful the treatment will be, and the risk of complications will decrease.
Symptoms
Costen's syndrome is characterized by the presence of a collection of symptoms that are rarely interrelated.
In addition, in the initial stages of the disease, symptoms may not appear, which delays the patient’s visit to the dentist and complicates timely diagnosis.
Most often, patients experience the following signs of disease development:
- pathologies in the functioning of the temporomandibular joint - difficulties during opening and closing of the jaw, the appearance of crunching and clicking, severe pain during chewing;
- the appearance of dryness and acute pain in the root of the tongue and pharynx;
- the formation of a herpetic rash on the mucous membranes of the oral cavity and the outer edge of the ear canal;
- the occurrence of trigeminal neuralgia - severe pain of a paroxysmal nature that affects one side of the face - jaw, cheek, ear, eye;
- pain in the ears and head, which may worsen when sneezing or singing.
In some cases, patients may experience frequent dizziness, hearing loss, and pain in the cervical spine.
Variants of Thoracic Outlet Syndrome
Neurological This form of thoracic outlet syndrome is characterized by compression of the brachial plexus. The brachial plexus is a network of nerves that arise from the spinal cord and pass through the space between the first rib and the collarbone to the arm. These nerves stimulate muscle movement and conduct sensation in the shoulder, forearm, and hand. Most often, it is the neurological variant of thoracic outlet syndrome that is observed, when patients complain of pain in the arm, weakness, numbness, and tingling. Vascular This type of disease occurs when the subclavian vein or artery becomes compressed between the collarbone and the first rib or pectoral muscle. Such patients may develop thrombosis of the subclavian vein or artery with the development of vascular insufficiency in the arm. Mixed When there are signs of compression of the nerves and vessels at the exit from the chest. This is the most painful form, but much easier to diagnose.
Classification
During the development process, pathological bite syndrome goes through four stages, each of which is characterized by the following symptoms:
- First stage. The size of the joint space narrows unevenly, and slight loosening of the ligament apparatus is observed. A person begins to experience the first symptoms of a pathological change in the cartilage disc.
- Second stage. The mobility of the temporomandibular joint decreases, ossification occurs in the area of the condylar process of the mandible.
- Third stage. Degeneration of the cartilage disc continues, and sclerosis of the articular surfaces develops. Movement of the lower jaw is severely limited.
- Fourth stage. The patient experiences a strong proliferation of fibrous tissue, and the mobility of the lower jaw is completely absent.
A person experiences persistent pain in the jaw area, radiating to the ear or cheek. At this stage, treatment is carried out exclusively by surgical methods.
TMJ dysfunction - symptoms and treatment
There is no single, universal method for treating TMJ dysfunctions. Full treatment may be hindered by pain that does not allow the necessary therapeutic measures to be carried out.
Conservative therapy allows you to relieve acute manifestations of pathology, ensures the weakening or complete disappearance of symptoms and restores the function of the lower jaw in full.
Physiotherapy is effective in reducing pain. To reduce pain, fluctuarization is used in the TMJ area. The essence of the procedure is the use of alternating, partially or fully rectified low-voltage electric current with a chaotically varying oscillation frequency. Fluctuarization helps reduce pain after 2-3 sessions. If the myogenic nature of the pain is caused by myositis (inflammatory damage to the skeletal muscles) due to contact involvement of the muscle in the inflammatory process, then treatment should first of all be aimed at eliminating the cause of the inflammation.
Amplipulse therapy (sinusoidal modulated current therapy) has shown effectiveness in the treatment of myofascial syndrome (a chronic condition in which pain points form in muscle tissue), reducing the tone of spastically contracted muscles.
Pain of joint origin is treated by prescribing phonophoresis with hydrocortisone, which allows to relieve pain in the acute period and reduce inflammation.
All types of treatment must be carried out under the control of electromyography to assess the effectiveness, equalize and normalize the electrical potentials of the muscles.
During complex treatment, the patient himself must perform myogymnastics after proper training in the technique. It includes passive and active exercises for the moving muscles of the lower jaw and neck muscles. Passive exercises are carried out without load; the patient needs to perform various movements of the lower jaw. Active exercises also include various movements of the lower jaw, but with a load (the patient’s arms counteract the movement being performed) [3]. Exercises should be done 3 times a day for 10-15 minutes.
To normalize bite and occlusal disorders, special orthopedic treatment methods are used - correction of occlusion and the use of orthopedic structures (splints, mouth guards, bite blocks, myostimulation, etc.).
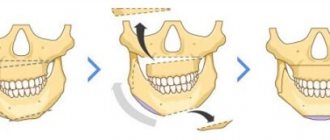
Surgical treatment methods are used for serious morphological pathological changes in the joint. The main indication for surgical treatment is anterior displacement of the intraarticular disc.
Surgical treatment consists of focal chondroplasty of the disc or head of the lower jaw using autologous cartilage (usually nasal cartilage). It is also possible to reduce the disc and suturing the stretched intra-articular ligaments and joint capsule. These methods are aggressive for a complex articular system and they do not always give good results [11].
In the complex issue of treating TMJ dysfunction, over time, the most effective scheme has proven to be the use of medication, manual therapy, physiotherapy and orthopedic treatment aimed at restoring the dentition and normalizing the bite.
Consequences
Lack of treatment in the initial stages of the disease can lead to a significant deterioration of the situation, increased pain and decreased mobility of the temporomandibular joint.
Among the common complications of Costen syndrome, the most common conditions are:
- Indigestion. Due to limited mobility of the jaw joint and severe pain that accompanies the chewing process, grinding hard foods in the oral cavity is noticeably impaired. This entails an increased load on the organs of the gastrointestinal tract.
- Weakening of the ligamentous apparatus. As a result of this phenomenon, a fairly free exit of the head of the lower jaw from the articular fossa occurs.
- Accumulation of inflammatory exudate in the joint cavity. An excessive amount of fluid in the joint cavity contributes to a loose fit of the disc to the head. As a result, popping sounds occur when the jaw moves.
Stages of development and diagnosis
The syndrome does not appear immediately. In its development, it goes through four stages, each of which is characterized by the following pathologies:
- The gap between the joints decreases, the ligaments are slightly weakened.
- The posterior process of the lower jaw, connecting to the temporal bone, ossifies, and the mobility of the joint decreases.
- The cartilage is destroyed, dense connective tissue forms on the surface of the joints, and jaw movements are limited.
- The joint is completely immobilized, the patient constantly experiences severe pain, which analgesics cannot cope with.
The earlier the disease is detected, the easier it is to treat, so you need to consult a doctor in a timely manner. The specialist will diagnose and prescribe appropriate therapy.
Because symptoms are nonspecific and each may indicate a different problem, a comprehensive examination is required to make a diagnosis. The doctor carefully listens to all the patient’s complaints, then conducts a computer and magnetic resonance imaging examination of the joint area, nasopharynx, and paranasal sinuses. The latter method is especially informative, since it allows you to visualize individual elements of the joint without radiation exposure to the body.
Since the temporomandibular joint is connected by ligaments to the malleus of the middle ear, hearing acuity is measured using an audiometer. If the clinical picture is similar to arthrosis or arthritis, panoramic X-rays of the lower jaw are taken. With the syndrome, they should not be affected by pathological changes. In addition, electromyography of the muscular masticatory apparatus and impedance examination of the middle ear may be needed.
Additionally, the doctor can check the smooth sliding of the heads of the jaw joints. To do this, the patient is asked to tightly close the ear canals with his fingers and move his jaw. In the case of Costen's syndrome, characteristic clicking and crunching occurs due to the loose fit of the disc to the articular head.
Sometimes the symptoms described by the patient are very similar to Costen's syndrome, but there is no joint damage. In this case, it is necessary to check the condition of the masticatory muscles. If, with the mouth open, the joints of the middle, ring and index fingers do not pass clearly between the lower and upper incisors, there is a high probability of muscle damage.
If necessary, the doctor carries out other procedures necessary in his opinion, and may also recommend that the patient additionally consult with an otolaryngologist, neurologist, geneticist or orthodontist.
Diagnostics
To determine Costen's syndrome, the dentist must carry out a number of mandatory procedures, since the presence of a variety of symptoms often complicates the diagnosis:
- Examination of the patient and clarification of existing complaints.
- Phalangeal test to detect Costen's syndrome. The essence of the method is that in the absence of disease, during the opening of the oral cavity, the phalanges of three fingers should be located unhindered between the teeth of the opposite jaws.
If this is problematic and only two fingers fit into the gap formed, the dentist concludes that there is temporomandibular joint dysfunction. - Tympanometry of the ear. The examination allows us to identify the presence or absence of middle ear pathologies in order to correctly diagnose the disease.
- An X-ray examination is carried out to determine the condition of the dentition and the structural anomalies present in it.
- Consultation with relevant specialists. To exclude diseases with similar symptoms, an examination by an otolaryngologist, orthodontist, or neurologist may be required.
Indications for compactosteotomy and surgical technique.
In this publication, see photos of tooth protrusion.
Follow the link https://orto-info.ru/zubocheliustnye-anomalii/zubov/kolichestva/skuchennost-i-sposobyi-ustraneniya-problemyi.html if you are interested in methods for treating crowding of the lower row of teeth.
Temporomandibular joint dysfunction
For many years, lung cancer has maintained a leading position in prevalence and mortality among cancer diseases. How common is this disease in Russia? What trends are visible?
Ksenia Sarantseva
, PhD, oncologist, researcher at the chemotherapy department No. 17 of the National Medical Research Center of Oncology named after. N. N. Blokhina
Lung cancer is a very common disease. More than 50 thousand new cases are detected in Russia every year. And, unfortunately, so far we have not seen any trends towards a decrease in morbidity and mortality. This is mainly due to the fact that smoking is extremely common in the Russian Federation - one of the factors that does not allow these indicators to decrease.
Men are generally more susceptible to lung cancer. What is the situation with morbidity among women?
Indeed, women get lung cancer slightly less often than men. But despite this, the disease occurs quite often. According to statistics, this type of cancer ranks on average third or fourth in terms of incidence among women and is second only to breast and skin cancer. Moreover, in recent years we have noticed an increase in the number of new cases among women.
What are the reasons for the increase in incidence among women?
Several important factors can be identified. Firstly, this is smoking. The problem of female smoking is very relevant in Russia and many other countries. Secondly, for a long time women were not considered as potential patients with lung cancer, and they were less likely to undergo diagnostic and screening programs. Fortunately, the view on this problem is now changing, which is responsible for the growth to a certain extent.
For what reasons is lung cancer often diagnosed at late stages? How to suspect the disease in time?
Unfortunately, lung cancer is mainly diagnosed at stages III-IV, and this is a worldwide problem. Late diagnosis is associated with the peculiarity of the disease, which is asymptomatic in the early stages. The first manifestations, such as cough or shortness of breath, indicate a fairly common process. To date, there are no 100% early diagnostic methods. As practice shows, the most informative in this regard is a low-dose CT study, but it is not available in every region of the Russian Federation.
Regular preventive examinations and clinical examinations according to age, timely fluorography or chest x-rays make it possible in some cases to identify, perhaps not early, but not yet advanced forms of a lung tumor. It is also worth noting that during the pandemic, people actively underwent CT examinations, and therefore a large number of new cases were identified.
Are there any symptoms that can help diagnose cancer at an early stage?
Unfortunately, as I mentioned earlier, there are no specific symptoms. Their appearance signals an already widespread tumor process. In general, I can say that it is important to be attentive to your health. If symptoms such as weakness, fatigue and weight loss are noted, which are difficult to associate with changes in lifestyle, diet or other diseases, and a cough has appeared - although not painful, but which was not there before - of course, all of the above is a reason consult a specialist and carefully understand the causes of these symptoms.
Tell us what types and stages of lung cancer exist?
Lung cancer can be divided into two subtypes, each of them is a completely separate disease with its own course. These are non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC occurs in 70-80% of cases, SCLC - in approximately 20%. NSCLC is divided into several histological variants, each of which should be considered as a separate disease: adenocarcinoma, which is often associated with the presence of genetic damage - the so-called mutations - as well as squamous cell lung cancer, which is more often detected in people with a long history of smoking. There are also other, rarer options, for example, large cell lung cancer, but in most cases in practice the first two options are encountered.
In oncological practice, it is customary to distinguish 4 stages:
- the first stage is the most localized, when we are dealing only with a fairly small tumor (up to 3 cm) without affecting nearby lymph nodes;
- the second stage is characterized by the presence of a formation up to 5 cm in size and damage to nearby intrathoracic lymph nodes;
- in the third stage, the spread by lymph nodes exceeds more than one lymphatic collector;
- the fourth stage is characterized by distant lesions, for example, not only the lung is affected, but also, say, the brain, liver or kidneys.
Stages are an element that the oncologist focuses on when selecting treatment tactics for a particular patient.
Fortunately, today there is no stage at which we cannot treat the disease. How is lung cancer diagnosed? How long does it take to make a diagnosis?
According to modern standards, we should spend no more than two to three weeks from the moment a tumor in the lung is identified on an x-ray or computed tomography until the start of treatment. What this process looks like: at the first stage, the patient complains to a therapist and undergoes an initial examination - a chest x-ray or a low-dose CT scan, the results of which may suggest the presence of a darkening or formation in the lung. If radiography was performed, then an additional spiral computed tomography is mandatory to clarify the nature of the changes.
The next stage of diagnosis is morphological verification, that is, obtaining a piece of tissue or several cells from this formation. A biopsy can be performed in several different ways.
Surgery may be performed if the tumor is small and localized. Thus, the patient will immediately receive both radical treatment and verification (that is, confirmation) of the diagnosis. However, most often verification begins with a transthoracic biopsy, when a puncture is made through the chest and a column of tissue is taken. There are also other options for endoscopic interventions (for example, bronchoscopy).
It is important to understand that a diagnosis can only be made after the oncologist receives a cytological (examination of tumor cells on glass) or histological (examination of a piece of tumor tissue) conclusion, which will indicate that the patient is suspected or confirmed to belong to one of the morphological types of lung tumors: non-small cell (adenocarcinoma or squamous cell) or small cell lung cancer. The doctor can then determine the clinical stage and choose a treatment option for the patient.
Lung cancer is often detected in late stages. Tell us what treatment options exist in this case and how effective is the therapy?
We truly have a large arsenal of drugs and technical capabilities for the treatment of lung cancer. In recent years, a very big breakthrough has been made when immunotherapy entered our practice.
What is in the oncologist’s arsenal today: first of all, this is classical chemotherapy, which everyone is accustomed to, but it is being replaced by more effective combination regimens that combine chemotherapy and immunotherapy, as well as monotherapy with immune checkpoint inhibitors, that is, immunotherapy in the form self-treatment. Another important area is targeted therapy, which is indicated for patients with a genetic disorder that led to the development of a tumor. Such therapy is prescribed if the patient, based on the results of molecular genetic testing, has a mutation in the EGFR gene or a translocation of the ALK gene. In these cases, there are drugs that block the work of this particular gene, returning the body to an almost healthy state. For such patients, targeted therapy is indicated.
Surgical treatment does not lose its relevance, especially if we are talking about the early stages, which can also be combined, for example, with chemotherapy or immunotherapy before surgery, which allows achieving significant results. Thus, I can say for sure that today Russian oncologists have a large number of different methods of treating lung cancer in their arsenal.
What myths about the disease do you come across most often?
The most important (and most dangerous!) myth is that lung cancer is a death sentence; it is a disease that is pointless to treat. Of course, just a few decades ago the life expectancy of our patients barely reached nine months. But today the level of medicine allows us to achieve the point that you can live with lung cancer for several years with virtually no signs of the disease.
In addition, many people believe that lung cancer is a disease of smokers or older people. Unfortunately, genetic damage also plays a significant role in the development of lung cancer, and in our practice we often encounter very young patients who have never touched tobacco.
Another common myth is the existence of traditional medicine that can treat more effectively than the drugs that oncologists can offer. In reality, the opposite often happens: out of ignorance, patients begin to take various extracts from plants and herbs, which may contain plant poisons, for example. After such “pseudo-treatment”, some of them have impaired liver function, and we are no longer able to carry out traditional treatment, which in any case puts a strain on this organ.
Therefore, if you notice unusual or suspicious symptoms, please consult a doctor and under no circumstances seek help from people who promise a complete cure in the shortest possible time!
Treatment
After making a diagnosis, the specialist makes a decision on the need for specific therapeutic measures.
Their complexity depends on the severity of the pathology, however, in any case, the patient must follow the following recommendations to help reduce the load on the jaw joint:
- Stick to a diet. It is necessary to stop eating hard foods and switch to soft and pureed foods. It is advisable that the basis of the diet be
cereals, purees, dairy products.
- Avoid prolonged socializing and chewing gum to reduce the impact on the jaw.
- Reduce stress levels in everyday life, since high nervous tension increases pain impulses.
- Sanitate the oral cavity to eliminate problems that may serve as aggravating factors.
Drug therapy
To eliminate the inflammatory process and relieve pain, specialists can prescribe the patient a complex of medications, which includes:
- Painkillers and anti-inflammatory drugs - Ibuprofen, Dexalgin, Brustan, Ketonal. The drugs have a high analgesic effect and reduce the manifestation of the inflammatory-degenerative process in the cartilage disc.
- Activators of metabolism in tissues - injections or Solcoseryl gel, tablets, ointment or Actovegin gel. Thanks to these drugs, the regenerative process is stimulated and tissue trophism is improved.
- Drugs from the muscle relaxant group help reduce the tone and tension of the jaw muscles and reduce the severity of muscle spasms. Most often, experts prescribe drugs such as Baklosan, Sirdalud, Tizanil.
- Multivitamin complexes – Neurodiclovit, Milgamma, Neurobion, Neuromultivit. Due to the high content of B vitamins in these preparations, pain in inflamed joints is relieved, the processes of creation and blood circulation are improved, and the functioning of the central nervous system is stabilized.
- Sedatives - Afobazol, Fabomotizol, Noofen, which reduce feelings of anxiety and tension, making the pain impulse less pronounced.
Physiotherapy
If a disease is detected at the initial stage, a set of physiotherapeutic procedures, which includes the following measures, may be sufficient to eliminate it:
- fluctuarization of the masticatory muscle area - the procedure has a relaxing and analgesic effect;
- electrophoresis of drugs allows you to increase their effectiveness in reducing pain, relaxing muscles and improving regenerative processes;
- diadynamic therapy - exposure to continuous pulsating current for several minutes produces a pronounced anesthetic effect and helps improve tissue trophism;
- UHF therapy , which is a general and local effect of an electric field, allows you to deeply and evenly heat the inflamed tissue, increasing the rate of its regeneration.
To increase the effectiveness of therapy, experts recommend combining physiotherapeutic procedures with massage of the jaw area, myogymnastic exercises, and acupuncture procedures.
In addition, the orthodontist may recommend the use of a special device that limits the degree of opening of the oral cavity, which reduces the load on the joints.
Surgery
The surgical method of eliminating Costen's syndrome is used at an advanced stage of the disease when other methods of therapy are ineffective.
Surgery is risky because there is a risk of severe bleeding, nerve damage, or scarring of the joint.
At the same time, surgery to remove elements of the temporomandibular joint, such as the cartilage disc or head, may be the only option to restore the proper functioning of the jaw.
In this case, in place of the removed elements, the specialist installs a graft, which allows you to restore proper contact and opening of the jaw rows, as well as establish a painless chewing process.
Discussion
The pathology of the TMJ has been the subject of study by dentists, maxillofacial surgeons, neurologists and ENT doctors for many years [8–12]. Within each specialty, as a rule, narrow aspects of the pathogenesis of Costen syndrome and the possibility of their correction are considered. Thus, maxillofacial surgeons restore the correct relationships of the elements of the TMJ, the activities of orthodontists are aimed at restoring adequate occlusal relationships, neurologists use mainly medicinal methods to combat tinnitus, and ENT doctors often identify and treat dysfunction of the auditory tube, which is associated with noise in the ear and dizziness. At the same time, a general idea of the problem that takes into account all components of the disease is not formed, and therefore, treatment results are rarely satisfactory.
The paired TMJ is one of the most complex joints of the human body and includes a special type of head of the jaw bone, the presence of an intra-articular disc and the Pinto ligament connecting the disc to the handle of the malleus, masticatory muscles that have a certain effect on the muscles of the middle ear and muscles that regulate the lumen of the auditory tube. The abundance of options for disruption of these diverse connections gives rise to a wide range of clinical manifestations of TMJ pathology, representing Costen's syndrome. One should also take into account the different adaptation limits of patients: from the absence of clinical symptoms even in the presence of articular pathology to a detailed picture of articular dysfunction when the compensation limit is reached.
The severity of the pain syndrome can increase with the formation of central sensitization due to disruption of the functioning of the central mechanisms of pain perception [13]. This usually occurs along with the development of emotional distress due to chronic pain; the pain syndrome acquires a special character and requires the prescription of antidepressants and/or anxiolytics [14].
It turned out that only a combined effect, including drug therapy, correction of osteopathic dysfunctions and splint therapy, led to a complete clinical effect and stable restoration of intra-articular relationships (n=14; 93%). In the only case of a partial effect of complex therapy, there was an anterior displacement of the heads of the mandibular bone without restoration of the relationships when opening the mouth, combined with pronounced occlusal disorders. Resistance to therapy in this situation was due to the length of the medical history (16 years) and the formation of dystrophic changes in both TMJs.
It should be noted that if drug treatment of pain, myofascial and anxiety-depressive syndromes was carried out within the framework of current recommendations, then the osteopathic component of therapy included a kinesiological assessment of postural disorders with their subsequent correction [15-17]. This approach made it possible to more effectively combat pain and inactivate myofascial trigger points in groups 1 and 3.
Price
The cost of eliminating Costen syndrome depends on the severity of the pathology and treatment methods:
| Procedure name | Cost of carrying out, rub. |
| Fluctuarization | 800—1700 |
| Electrophoresis | 900—2700 |
| Diadynamic therapy | 500—1500 |
| UHF therapy | 600—1500 |
| Acupuncture | 3 000—4 000 |
| Massage | 1 700—3 200 |
| Surgery (arthroplasty) | 55 000—100 000 |
The large difference in prices is explained by the location of the clinic, the professionalism of the staff and the average cost of similar services in different cities of the country.
Additional information about the temporal joint anomaly is presented in the video.