Any surgical intervention is serious and the implantation of artificial tooth roots is no exception. The procedure requires attentiveness and concentration not only from the attending physician, but also from the patient. Proper preparation will reduce the likelihood of unpleasant and undesirable consequences. Detailed tips and recommendations will help you understand what you need to know before dental implantation, how to behave and what to prepare for.
Before surgery, it is necessary to carry out professional oral hygiene.
If the operation is performed with an anesthesiologist, you must come with an accompanying person, or the operation will be cancelled.
Recommendations for surgical treatment
After surgery, you may experience pain, which will go away as the tissue heals. Postoperative swelling or hematoma can also occur in areas adjacent to the surgical site, which is a natural consequence of surgery. There may be a slight increase in body temperature.
Please follow our recommendations!
Why do you need to get tested?
Based on the state of the blood, you can objectively assess the actual state of the body and calculate possible risks during surgical procedures. Taking tests helps the doctor confirm possible assumptions about common diagnoses or notice something new that may affect the course of the operation.
There are various types of blood or urine tests that can help identify dangerous pathologies for the body. For example, the level of AST and ALT enzymes may indicate cardiovascular diseases and a previous heart attack. Any surgical interventions are contraindicated within 6 months after myocardial infarction.
For women, it is important to pay attention to thyroid hormone levels and parathyroid hormone, as they reflect the activity of calcium metabolism. Based on these tests, it can be concluded that osteoporosis is present. Often, implantation is not indicated for this disease due to deterioration of the bone tissue.
Another important indicator is blood sugar level. Values greater than 10 mmol/l suggest the presence of diabetes mellitus. For people with a confirmed diagnosis, glucose values should also not exceed 10 mmol/l, because this disease affects the implant’s healing and increases the risk of its rejection and the occurrence of an inadequate immune system response.
In addition to blood counts, doctors prescribe tests to detect various infections. This is important for both the patient and the doctor to ensure the safety of the surgical procedure for all involved. Chronic infections distort the immune response and can cause complications.
Before surgery
- Prepare an ice pack at home.
- On the day of surgery, eat a light meal 2-3 hours before your scheduled time.
- The day before surgery, the consumption of alcoholic beverages is strictly prohibited.
- Be sure to inform your dentist about all the individual characteristics of your body and any allergic reactions, in order to accurately select an anesthetic that is safe for you.
- Visit the toilet before surgery.
- It is better to come to the operation in loose clothes without a collar.
What to consider before planning implantation
When deciding to undergo implantation, you should take your choice of clinic and doctor seriously. The success of the operation, the duration of treatment and the service life of the implants depend on the actions of the patient, but the professionalism of the clinic team plays a decisive role. It is better to consider 2-3 centers at once to compare and choose the best one. When visiting the clinic, you should pay attention to:
- Location. Choose a dentist that is easy for you to get to.
- Equipment. The clinic must be well equipped (for diagnosis, treatment, operations). Plus - the presence of a separate surgical unit and its own dental laboratory.
- Documentation. By agreeing to implantation, the patient signs an agreement with the clinic. Pay attention to the list of services that are included in the cost of implantation, guarantees, price, payment terms (should not change from the moment the contract is concluded). Discuss warranty periods and warranty cases.
- Price. Study the prices of several clinics. When you see a temptingly low price for implantation, you don’t need to be seduced. An operation involving the installation of high-quality implants, performed by a highly qualified implantologist, cannot be cheap.
- Reviews. Study opinions on clinic websites, forums, ask friends or relatives.
- Doctor's qualifications. The implantologist must have a diploma confirming higher education and advanced training certificates. It is better if the operation is performed by a maxillofacial surgeon.
- Comfort. Communication with an implantologist is long-term—the level of trust and approach are important. Choose a specialist whom you can trust with your health.
It is worth focusing on the predicted results of the operation. The doctor must choose the optimal solution to your problem. A professional does not sacrifice smile aesthetics for quality or vice versa, so do not settle for conflicting results.
After operation
— To avoid severe swelling and bleeding during the first 24 hours after surgery, it is necessary to apply an ice pack to the cheek on the side of the operation for 15-20 minutes with breaks of 30-40 minutes.
- Rinsing your mouth when bleeding is unacceptable!
— After sinus lift surgery, you should not drink through a straw, blow your nose vigorously, or puff out your cheeks.
- To reduce the likelihood of nosebleeds (after upper jaw surgery) and reduce post-operative swelling, you should sleep with your head elevated (add an extra pillow) for several days after surgery.
— It is not recommended to use tobacco products 1 week before and 2 weeks after surgery.
— It is prohibited to drive a car on the day of surgery with premedication.
- It is not recommended to eat until the anesthetic wears off. In the first days after surgery, it is recommended to eat soft, non-hot foods.
— It is not recommended to drink alcohol, coffee, or strong tea to avoid the negative effects of these drinks on blood circulation and wound healing.
In what cases is dental treatment performed under anesthesia in adults?
The problem of ordinary fear of the dentist does not require such a radical measure as anesthesia, but can be easily solved with the help of sedation. This is a gentle alternative to general anesthesia, in which the person is half asleep, physically and emotionally relaxed, and also does not retain memories of what happened. By the way, the vast majority of clinics, when offering dental treatment under anesthesia, still mean sedation. However, real “general anesthesia” with loss of consciousness is very often used in modern dental practice.
Meanwhile, the main dental interventions for which general anesthesia may be a better choice than local anesthesia are only complex maxillofacial operations, as well as a number of indications that are worth knowing about:
- allergy to local anesthetics;
- low pain threshold;
- large volume of required treatment;
- developed gag reflex;
- increased fear of dental treatment.
Additional Tips
Avoid lifting heavy objects, bending over, playing sports, or taking hot baths for 5 to 7 days after surgery.
Within a few days, performance and the ability to drive may be reduced.
Remember to take medications prescribed by your dental surgeon after surgery.
We kindly ask you!
Appear for examination and removal of stitches 5-7 days after surgery, in agreement with your surgeon. You must immediately notify your surgeon or clinic administrator of any changes in your health.
Recommendations for caring for dental implants
The service life of the implant depends on:
- The correctness of the surgical and prosthetic stages carried out in the dental clinic.
- The patient's compliance with the recommendations given by the dentist immediately in the postoperative period and the period after implant prosthetics.
- Careful hygienic care of the “implant-crown” structure.
- Blood supply to bone tissue and gums in the area of implantation. (Smoking cigars and cigarettes has a very, very negative effect on peripheral blood circulation, which can even interfere with implant implantation.!!!)
Initial appointment and consultation before dental implantation
At the first appointment, a competent specialist can interview the patient and conduct an initial diagnosis. It is very important from the very beginning to find out about the patient’s health status, the presence of chronic diseases or conditions in the acute stage, and be sure to obtain all the information about the medications taken.
In the questionnaire that patients fill out before surgery, it is necessary to honestly answer questions and indicate chronic pathologies, as well as allergies, if any.
These data will influence the choice of treatment tactics and the drugs used, in particular the choice of anesthetic.
In some cases, the doctor may prescribe an additional examination in the form of a general blood test.
Why is it important? Because many diseases and borderline health conditions affect metabolism, and this in turn affects the healing process, which is the most important stage in implantation. Future prosthetics and the service life of crowns depend on the engraftment of the titanium root.
Oral hygiene
Regardless of the size or number of implants, they must be cared for as if they were regular teeth. Brush and floss your dental implants twice a day. Use special fluffy dental floss (for example, Oral-B superfloss or ultrafloss).
When brushing your teeth, pay special attention to the back teeth and between teeth. Use a soft or medium-hard brush. In addition, use an irrigator for additional deep cleaning of the interdental spaces with water irrigation.
There are special brushes that can be used to clean interdental spaces - dental brushes. Ask your dentist about them - in some cases they are not recommended.
Visit your dental hygienist twice a year; they are the only ones who can clean your implants as thoroughly as necessary. Regular visits to the dentist are very important. Your dentist will check the condition of your gums, jaws and implants.
Smoking is bad for your health and for dental implants, too. To have a good prognosis for the lifespan of your implants, it would be a good idea if you stopped smoking.
3D planning for dental implant installation
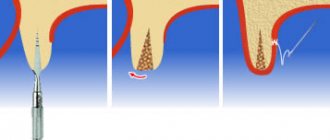
The results of a CT scan and other measurements of the jaw are entered into a special computer program to visually reconstruct the jaw.
The implantologist calculates the location for the implants and draws up a detailed surgical plan. In difficult situations, the doctor models the jaw visually and then creates a 3D model of the patient’s jaw (using a 3D printer). The model is made of special plastic that imitates the jaw with the patient’s bone density. Using a lithographic model, the implantologist reproduces the operation, studies the structure of the jaw and the nuances of installing implants.
Eating
Avoid chewing hard candy, ice, or other hard foods (such as hard chocolate or dry fish) as they may loosen or break the abutment screw.
Avoid foods such as caramel or toffee, as they may stick to the crown and cause the abutment screw to loosen.
Do not open bottles or crack nuts with your teeth for the same reasons.
Wear protective sports mouth guards when participating in sports and avoid direct blows to the face.
Refrain from grinding your teeth. If creaking occurs unintentionally or during sleep (bruxism), notify your dentist and he will make you a thin night guard.
The length of their service depends on the quality and regularity of care for implants.
Before and after implantation
Before surgery:
Prepare several days off after the date of the planned operation.
Do not smoke or reduce the number of cigarettes you smoke.
If you are sick on the eve of the operation, please notify the implantologist.
Ask your implantologist about the medications you will need immediately after surgery.
Patients suffering from compensated diabetes mellitus must follow a strict diet 2 weeks before surgery and 2 weeks after it.
Get a good night's sleep the night before surgery.
Make sure you are accompanied if you plan to undergo anesthesia, sedation or a complex operation, do not plan to be behind the wheel.
If you have herpetic rashes on the mucous membrane, the operation should be rescheduled.
Mandatory tests
The doctor individually informs each patient what tests are taken before implantation, which are indicated for all patients at risk. For healthy patients, X-ray diagnosis is often sufficient, provided there are no chronic diseases.
Below is a list of tests that a specialist prescribes without fail:
- General blood analysis
- General urine analysis
- Blood chemistry
- Blood sugar test (included in biochemistry)
- ESR
- HIV
- Syphilis
- Hepatitis B, C
- Rh factor, blood group
The list changes at the discretion of the doctor depending on the patient’s health. Based on the results of the research, the specialist may delay the operation.
Relative contraindications to implantation include:
- Exacerbations of chronic diseases
- Exacerbation of infectious diseases
- Increased blood sugar
- Myocardial infarction less than 6 months before surgery
- Hormonal disorders
- The need for bone grafting (to be decided individually, in some cases it is possible to do bone grafting and implantation in one visit)
- Pregnancy and lactation
- Lack of oral sanitation
- Taking medications that affect blood pressure, blood clotting, etc.
Among these factors, the doctor also makes an individual decision about the possibility of surgery.
There are a number of contraindications that completely exclude surgical intervention.
Absolute contraindications:
- Hemophilia
- Presence of malignant tumors
- Mental illness
- Allergy to anesthetics
- Diabetes mellitus type 1
- Immune system disorders
- Severe pathologies of the cardiovascular system
For all conditions, there is a certain list of tests and corresponding symptoms, according to which the surgeon determines to delay implantation or even choose a different tactic for treating the patient.
After operation:
If you have had dental implants, you may experience some of the typical discomforts associated with any type of dental surgery. These may include:
- Swelling of the gums and face.
- Gum injury.
- Mobility of adjacent teeth.
- Pain at the implantation site.
- Minor bleeding.
- Bruises and bruises.
You may need painkillers and antibiotics. Follow the recommendations of the implantologist.
What must be observed after implantation:
- Brush your teeth with a soft brush before removing sutures
- Eat soft foods for 5-7 days. Do not eat hot, spicy or salty foods.
- Starting from the third day after surgery until the sutures are removed, you should rinse your mouth with a chlorhexidine solution twice a day (after brushing your teeth).
- Do not overheat in the sun or in a sauna.
- Do not engage in active sports.
- Do not smoke or reduce the number of cigarettes you smoke.
- Do not fly on an airplane, do not swim, do not dive for 2 weeks (especially important after sinus lift surgery).
- Do not blow your nose or sneeze with your mouth open (especially important after sinus lift surgery).
- If swelling, discomfort or other symptoms increase within a few days after surgery, or the temperature rises, contact your implant surgeon.
- After tooth extraction
- If you have had a tooth removed, you must take care of your oral cavity. By following certain recommendations, you will feel better and healing time will speed up.
What to take with you to the hospital?
You should be prepared to stay in the clinic for several days. Be practical and use common sense. Do not take valuables, fashionable clothes or large amounts of money with you. Bring a small bag with the essentials. You will need leg compression stockings, which help reduce the risk of blood clots during long surgery. This can include elastic bandages or special compression stockings. Immediately after the operation, to protect the sutures of the anterior abdominal wall, you will need to constantly wear a bandage - this is a special wide elastic belt that helps support the muscles of the anterior abdominal wall at times when there is strong pressure on it - when you stand up, cough, sit down or bend over. You will only be in bed for one or two days after surgery, after which you will be encouraged to get up and walk around. You may want to wear a robe or comfortable pajamas and slippers with non-slip soles. After surgery, for some time, a small amount of wound discharge may be released from the sutures, which, even through a sterile dressing, can stain clothing. Therefore, prepare two sets of clothes and do not take expensive or favorite things, as they may get damaged in the hospital.
Don't forget toiletries such as a toothbrush, toothpaste, comb, deodorant, perfume or cologne, they will help you feel more “human” after surgery. During surgery, patients should not wear contact lenses, so do not wear them on the day of surgery; instead, it is better to wear glasses and leave contact lenses for the period after surgery. Before the operation, give valuables and wallet to your family members, leave a small amount of money to pay for television or telephone. You may also benefit from a good book, some magazines or a craft kit to help pass the time during your final days in the clinic when you feel better.
If you regularly take any medications (for example, for high blood pressure or diabetes), be sure to take them with you. It is very important that you continue to take these medications until the day of surgery, unless your doctor prescribes something else.
Stopping bleeding:
To control bleeding, it is necessary to bite down on a gauze pad placed by the dentist in the oral cavity. The pressure promotes the formation of a blood clot in the socket. If you have heavy bleeding that has not stopped within an hour of tooth extraction, you should bite into a regular tea bag. Tannin in tea helps in the formation of blood clots. Hold the tampon or tea bag until the bleeding stops.
Additionally, cool the extraction area, apply a cold compress to the face in the area of tooth extraction for 10-15 minutes. at one o'clock. A slight bleeding on the first day after removal is normal.
Diagnosis of cataracts
Modern equipment makes it possible to detect disturbances in the structure of the lens even at the initial stages of cataract development. Also, the patient himself should notice characteristic signs - narrowing of the visual field, loss of light sensitivity, visual clouding of the intraocular media, interfering with good vision. Cataracts most often develop in older people, along with other pathologies of the visual tract, especially presbyopia, a natural age-related farsightedness.
The main method for diagnosing cataracts is biomicroscopy, which involves examining the ocular media at multiple magnification under a special slit lamp. Such an examination allows you to determine the size and degree of cataracts, make predictions regarding the speed of spread of the process and the urgency of the operation.
It is also important to determine the degree of visual acuity, the preservation of the peripheral vision field, and to examine the fundus of the eye for changes in the neurovascular structures of the eye. An appointment with an ophthalmologist after 40 years of age must be accompanied by tonometry - measuring intraocular pressure to diagnose glaucoma.
Optical coherence tomography is a method for accurately determining the state of preservation of intraocular structures. Next, modeling and selection of a suitable intraocular lens are used.