Candidiasis or thrush
is a fungal, infectious disease caused by opportunistic fungi of the genus Candida. Microorganisms are present in most healthy people. A person may encounter them for the first time in the womb, during childbirth, or during breastfeeding. Candidiasis develops against the background of reduced immunity, when the body can no longer restrain the active proliferation of the fungus.
The infection affects the mucous membranes of the mouth and genitals. It can develop on smooth skin, nails, and in the intestines, as a type of dysbacteriosis. There is visceral (systemic) candidiasis that affects internal organs. Despite the fact that Candida fungi are present in many people, and the disease itself is considered a neglected disease, it must be treated even if there are no external manifestations.
Causes of candidiasis
- Frequent damage to the skin and mucous membranes, for example, due to illness, working with aggressive chemicals, dry skin, age-related changes.
- Prolonged exposure to water, humid and warm environments. This includes a climate that is not suitable for your skin type, as well as occupational hazards.
- Mechanical damage to the skin and mucous membranes: injection drug addiction, long-term surgical interventions, catheters, shunts, endotracheal tubes.
After entering the body, the fungus may not manifest itself for a long time, since its reproduction will be suppressed by the immune system. In some cases, natural defenses weaken, leading to candidiasis (thrush). Among the factors that contribute to the proliferation of Candida:
- Chronic, endocrine and immune system diseases (diabetes, HIV).
- Metabolic disorders or taking medications that disrupt the natural microflora (antibiotics, hormonal contraceptives).
- Unbalanced diet, lack of sleep, stress and depression.
The fungus can be found in raw meat, unpasteurized dairy products, and, in more rare cases, on fresh vegetables and fruits. You can become infected with candidiasis from animals: dogs, calves, poultry.
Treatment of uncomplicated VK
Uncomplicated VK is caused by strains of C. albicans, most of which exhibit sensitivity to azole antifungals. Treatment of an uncomplicated disease leads to a positive result in 90% of cases, even when prescribing a single dose of oral or a short course of local antimycotics. There are several topical azole drugs to choose from with approximately equal effectiveness.
The empirical prescription of antimycotics for this form of the disease is completely justified. Moreover, the choice of treatment is often based on the patient's individual preferences.
The Candida cell wall is a complex glycoprotein that depends on the constant synthesis of ergosterol. Azole compounds, which are the active ingredients of azole antifungals, block the production of ergosterol, allowing topical antifungals to be effective in 80-90% of cases.
Azole drugs, which are divided into imidazole and triazole derivatives, are the most numerous and effective group of antifungal agents. Azole antimycotics include both systemic drugs (ketoconazole, fluconazole, itraconazole) and local ones (bifonazole, clotrimazole, isoconazole, econazole and others).
In comparative trials of 10-14-day courses of therapy with azoles and nystatin, the preferential effectiveness of the former was revealed (80-95% of mycological cure compared with 70-80% in the nystatin group). In addition, azoles have proven effective even in short courses of treatment.
Therapy for VK in pregnant women involves the use of local antifungal drugs. Safe topical antimycotics include miconazole and clotrimazole; the recommended course of treatment is seven days. In addition, during pregnancy, the polyene antibiotic natamycin is prescribed. The standard regimen of antifungal therapy with local forms of natamycin is designed for use for three days. If necessary, the course can be doubled.
Risk factors for development
The likelihood of infection increases with casual sexual intercourse, uncontrolled use of antibiotics and drugs that disrupt the natural microflora. Foods with large amounts of sugar and carbohydrates create a favorable environment for fungal growth. Excessive sweating also leads to an exacerbation of candidiasis, so it is necessary to wear cotton underwear that allows the skin to breathe and moisture to evaporate.
At the same time, excessive cleanliness can also cause harm. We are talking about douching. It should not be used as a method of contraception, since it is not effective, and also as a means of hygiene, because it leads to the leaching of the protective flora. If you experience discomfort, you should first consult a doctor.
Treatment of complicated RVC
The optimal course of treatment for complicated VK has not yet been precisely determined. Some studies have shown the effectiveness of antifungal suppressive therapy for several months.
The drug of choice for RVC is oral fluconazole. For severe recurrent VK, fluconazole is administered at a dose of 150 mg (three doses) every 72 hours for nine days, after which treatment is continued at 150 mg per week for a long time. This antifungal regimen significantly reduces the likelihood of relapse compared with three doses of fluconazole without maintenance treatment.
Long-term suppressive therapy with oral fluconazole is convenient and well tolerated compared with other antifungal agents. Studies have shown that the effectiveness of a suppressive treatment regimen for RVC reaches 90%. Contrary to expectations, the development of resistance to C. albicans or superinfection with non-albicans species was not confirmed in patients taking fluconazole for a long time. However, in patients with persistent infection, identification of the pathogen is recommended.
Other oral agents that have proven effective in the treatment of RVC can be used as drugs for suppressive therapy. The following are prescribed as alternative treatment regimens:
- ketoconazole 100 mg per day (due to the hepatotoxicity of oral ketoconazole, preference is usually given to other drugs);
- itraconazole 200 mg twice a day for one day every month;
- clotrimazole vaginal suppositories.
For women who prefer topical treatment, clotrimazole is recommended at a dosage of 500 mg per week or 200 mg twice a week. The use of other local antifungal drugs is also permissible, and it practically does not matter which active ingredient is used.
In patients with RVC who do not undergo maintenance therapy, the probability of relapse within six months after successful treatment of the next episode of the disease is 70%. The risk of relapse in women taking antimycotics as suppressive treatment is 40-50% within one year after stopping the drugs.
Classification of the disease
Based on the depth of damage, candidiasis is divided into superficial and systemic forms. The first appear on visible parts of the body: mucous membranes, skin and its appendages. The second, systemic, are combined forms of the disease affecting internal organs. Without proper treatment, systemic (visceral) candidiasis can lead to the development of candidal sepsis. Most often, the fungus affects:
- gastrointestinal tract (esophagus, stomach, intestines);
- urinary organs (bladder, urinary tract, kidneys);
- lower respiratory tract (trachea, bronchi, lungs).
The disease is also classified based on the rate of spread of infection and the presence of relapses. Candidiasis of the liver and spleen often takes a chronic form. The acute, generalized form is asymptomatic candidemia, candida septicemia, candida thrombophlebitis, myositis, arthritis, cerebral candidiasis and other forms.
Classification of candida lesions according to ICD-10
- Candidiasis.
- Candidal stomatitis.
- Pulmonary candidiasis.
- Candidiasis of the skin and nails.
- Candidiasis of the vulva and vagina.
- Candidiasis of other urogenital locations.
- Candidal meningitis.
- Candidal endocarditis.
- Candidal septicemia.
- Candidiasis of other locations.
- Candidiasis, unspecified.
Officially, the diagnosis is made in accordance with ICD-10. In practical healthcare, such a classification is not entirely convenient, so they use the classification of deep candidiasis, which is a deeper list. When making a diagnosis, first indicate the name and form of the infection with a description of all localization points.
Skin treatment is carried out by a pediatrician in children and by a dermatologist in adults. Therapy is also carried out by doctors of other specializations, depending on the affected organ. For example, this could be a dentist, neurologist, gynecologist, pulmonologist.
Symptoms of candidiasis
The symptoms of the disease are directly related to the affected organ. Superficial forms have obvious signs, while systemic forms can be asymptomatic or be similar to other diseases. In the presence of chronic diseases (diabetes mellitus, HIV, AIDS, leukemia and other types of oncology), candidiasis may not be detected at all. Since its symptoms will be perceived by the patient as an unhealthy state due to the existing disease. To make matters worse, Candida susceptibility testing is not considered a routine procedure in many teaching hospitals and laboratories.
Candidiasis of the skin and nails
The infection is expressed in the form of allergic rashes (candidamycids), erythematous-squamous spots, urticarial and bullous type rashes. Nail pathologies are divided into:
- parochinia - purulent inflammation of the periungual and subungual spaces, absence of eponychium (skin at the base of the nail plate);
- onychia - purulent inflammation of the nail fold, deformation of the nail with discoloration and brittleness.
Candidal skin lesions may be accompanied by fever, inflammation and swelling of the lesions.
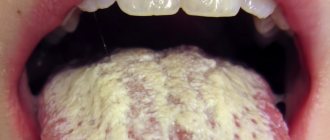
Candidiasis (thrush) of the oral mucosa
The fungus can affect both individual areas of the oral cavity and completely all mucous membranes: lips, gums, cheeks, palate, tongue, tonsils, uvula and pharynx. This is expressed in the presence of a white coating, compared to a curd mass. Swelling and redness may appear. There is often pain when swallowing, talking, or palpating. Saliva becomes viscous and bad breath appears.
Thrush may be accompanied by candidal cheilitis - damage to the lips and corners of the mouth. Painful cracks appear, covered with a white coating, and pieces of skin peel off from the lips. The disease is characterized by a long course with the possible addition of bacterial infections.
Intestinal candidiasis
Intestinal infection with fungi of the genus Candida can be an independent disease or develop as a result of damage to the oral cavity. Expressed as severe dysbacteriosis with the following symptoms:
- diarrhea;
- excessive gas formation;
- nagging pain in the rectum;
- an admixture of white flakes in the stool.
In most cases, symptoms are sluggish or completely absent. The disease is dangerous because the body does not receive enough vitamins and microelements, which is especially dangerous for a growing child.
Candidiasis of the genitourinary system (urogenital candidiasis)
Unlike sexually transmitted diseases, candidiasis of the genitourinary system is often hidden and asymptomatic. The fungus is discovered during a planned infection or against the background of other diseases. Symptoms begin to appear against the background of declining immunity, ongoing pathological processes of microflora destabilization and re-infection. In women, candidiasis manifests itself as follows:
- itching and burning of the external genitalia;
- swelling and redness;
- white, cheesy discharge;
- pain during sexual intercourse.
In men, the symptoms are similar:
- itching and burning of the head of the penis;
- white plaque and discharge:
- pain during sexual intercourse and urination.
Fungal infections of the bladder, excretory tract and kidneys are characterized by frequent urination, including false urges, pain in the suprapubic region. Candidiasis can be accompanied by bacterial infections. Complications include: cystitis, pyelonephritis, necrosis of the papillae, abscesses, formation of mycelium in the renal pelvis. Without proper treatment, against the background of chronic diseases, there is a risk of developing kidney failure.
Treatment of RVC caused by non-albicans Candida species
Non-albicans species respond very moderately to therapy with azole antimycotics. Therefore, the treatment regimen in such cases is selected individually, based on the severity of the disease and response to drugs.
Topical boric acid has been used to treat RVC for many decades. However, boric acid preparations can be absorbed through the vaginal mucosa into the blood and have a toxic effect. To avoid absorption, boric acid-based vaginal products are released in gelatin capsules. The recommended treatment regimen is one 600 mg capsule per day for two weeks.
There is no ready-made dosage form in Russia, but capsules can be prepared in pharmacies ex tempore. Studies have shown that treatment with vaginal boric acid capsules is effective in 70% of cases of C. glabrata-associated RVC.
An alternative to toxic boric acid is suppositories with amphotericin B. The antibiotic penetrates the cell membrane of the fungus and, by binding to ergosterol, destroys the cell wall. The course of treatment is 50 mg at night per os for two weeks. This treatment regimen is successful in 70% of patients suffering from disease caused by non-albicans species that are not amenable to azole therapy, especially C. glabrata.
Local preparations for vaginal use containing 17% flucytosine have also proven activity against non-albicans Candida species. Fungal cells absorb flucytosine, after which it is deaminated and converted into 5‑fluorouracil, which is incorporated into Candida DNA instead of uracil. As a result, protein synthesis is disrupted and the cell dies. A combination of 17% flucytosine cream and 3% amphotericin B cream is also possible. The average duration of treatment with flucytosine should be at least two weeks. The peculiarity of the drug is its high cost.
Diagnosis of candidiasis
The study is based on the isolation and identification of a species of fungus of the genus Candida. Currently, there are about 150 species, differing in morphological and biochemical properties. The most common fungus is C. albicans, accounting for up to 80% of cases of candidiasis of the digestive tract and up to 70% of genital infections. Before prescribing treatment, it is also necessary to determine the sensitivity of the isolated strain to antimycotics (antifungal medications): amphotericin B, voriconazole, itraconazole, fluconazole, flucytosine.
Microscopic diagnostics
1. Microscopy of a smear is taken from the area of the affected mucosa. Allows for comparative characterization of blastospores and pseudomycelia. During the study, fixed and native preparations that stain microorganisms are used. To increase the information content, pseudomycelia of cells are treated with dyes. The contrast in staining of microorganisms makes it easy to distinguish candida from other forms, including bacteria, under a microscope.
2. Bacterial culture allows you to identify the causative agent of infection and determine its concentration. The analysis is used to monitor the effectiveness of treatment, as well as to identify the sensitivity of candida fungi to various antimycotics.
Diagnostics by ELISA and PCP
1. Enzyme-linked immunosorbent assay (ELISA) is based on the determination of antibodies that are produced by the immune system in response to foreign substances in the blood. This technique allows you to identify the pathogen and the degree of its development, establishing whether the disease occurs in an acute or chronic stage.
2. Polymerase chain reaction (PCR) is a highly sensitive test that allows you to directly detect the infectious agent. Thanks to it, it is possible to differentiate Candida fungi with pseudomycelium from those that do not have it. These data are important for subsequent interpretation of results and deeper diagnosis.
Etiology of VK
Candida spp., the causative agents of vaginal candidiasis, are opportunistic fungi that are the most common cause of fungal infections in humans. The genus Candida has about twenty species. As a rule, BK is associated with one species of Candida, but there is a probability (2-5%) of simultaneous infection with two or more species.
In Russia, the USA, Australia and Europe, Candida albicans is most often detected in women with VK (76-89%). It is followed by C. glabrata (7-16%). The percentage of non-albicans Candida ranges from 11 to 24%. Some studies have shown a trend toward an increase in the incidence of non-albicans candidiasis, but recent work by scientists in the United States involving ninety thousand samples refuted this assertion: the proportion of Candida species causing BK remained virtually unchanged from 2003 to 2007.
Etiologically, various candidiasis are clinically very similar, however, atypical pathogens are characterized by resistance to azole antimycotics. C. glabrata and C. krusei are more resistant to azole antifungal drugs than others.
CC dossier
Marina Pozdeeva
pharmacist of the first category and head of the pharmacy. Author of numerous works on pharmacology and pharmacotherapy, Dnepropetrovsk.
These data highlight the importance of identifying Candida spp. in women with a high risk of developing non-Candida albicans-associated VK in order to select effective therapy for the disease.
Interpretation of results
If there are clear signs of candidiasis (thrush), and during a laboratory test blastospores and pseudomycelia of the fungus were identified, the study ends here. A diagnosis is made and treatment begins.
If a microscopic examination gives a negative result, this does not indicate the absence of infection. The disease can occur in a latent chronic form. It is necessary to carry out a number of other tests, for example, microscopic examination of scrapings, determination of Candida DNA in scrapings, urine, and prostate secretions. Also prescribed:
- Clinical blood test.
- Test for HIV infection.
- Determination of trace element reserves in the body.
- Test for glucose and carbohydrate metabolism metabolites.
These laboratory tests can help identify conditions that may be causing the fungus to grow.
Advantages of taking tests at JSC "SZDCM"
- Own laboratory with the latest diagnostic equipment.
- Convenient location of terminals within transport accessibility from anywhere in the city.
- Qualified laboratory technicians and friendly staff.
- Fast analysis and several options for obtaining results. Choose the one that is most convenient for you.
Medical centers and laboratory terminals of the North-Western Center for Evidence-Based Medicine are located in St. Petersburg, Leningrad region, Veliky Novgorod, Okulovka, Kaliningrad and Pskov.
Analyzes
- Bacteriological study for opportunistic pathogenic flora (OPF)
- NC yeasts of the genus Candida: C.albicans, C.krusei, C.glabrata
- Study of the biocenosis of the urogenital tract in women (“Femoflor 13 - screening”)
- Candida albicans
- Mycoses: identification of clinically significant fungi with determination of sensitivity to antimycotic drugs (only for fungi of the genus Candida and Cryptococcus neoformans)
- Specific immunoglobulin E - Candida albicans
go to analyzes