Candida mushrooms: from conditionally pathogenic to pathogenic
These oval or round unicellular microorganisms are present in the normal microflora of most healthy people. They are well protected from external factors and feel quite comfortable at human body temperature.
The very presence of Candida fungi in the body does not equate to a disease: the development of the pathological process begins if, under the influence of any factors, the fungi begin to actively multiply.
In most cases, this occurs due to decreased immunity.
The onset of the disease does not indicate a change in the properties of the fungus, but rather a change in the state of the body, in particular, a sharp decrease in its protective mechanisms.
to contents ^
Risk factors
Factors contributing to infection:
- uncontrolled use of antibiotics (in this case, treatment of intestinal candidiasis is especially often required), weakened immune system;
- failure to comply with personal hygiene rules;
- inflammatory and infectious processes (especially caused by bacterial infection);
- allergic reaction, wearing contact lenses (increases the risk of ocular candidiasis);
- severe stress, psychological and physical fatigue;
- sudden climate change;
- poor nutrition, diabetes and various diseases of the endocrine system;
- leaving the limbs in water for a long time (this can cause fungus on the nails).
These factors can become a trigger for the development of thrush. And before you think about how to cure candidiasis, you first need to eliminate the influence of such negative factors.
Causes of candidiasis
Intensive reproduction of the fungus can be provoked by various factors:
- Prolonged hypothermia or, conversely, being in a climate that is too hot and humid.
- A disease, especially if antibacterial drugs are used in its treatment.
- Severe stress.
- Changes in hormonal levels (with endocrine disorders, use of hormonal drugs, during pregnancy).
- Choosing underwear that is the wrong size or made from synthetic materials.
to contents ^
Prevention
In order not to think later about how to treat candidiasis, it is recommended to regularly prevent candidiasis. To do this, you need to switch to a healthy lifestyle, strengthen your resistance to any stress, infectious diseases, and avoid hypothermia. Hardening, consuming vitamin and mineral complexes, and a proper and balanced diet will also benefit. It is also important to promptly treat any diseases. Diet for candidiasis is also important: avoiding sweets, bread and confectionery, fatty foods, and fried foods. It is better to eat boiled and steamed food, as well as more fresh fruits and vegetables.
Types and symptoms of candidiasis
Manifestations of the disease are very diverse and depend on the specific location of development of the inflammatory process.
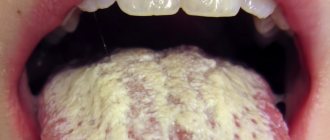
Oral candidiasis
Oral candidiasis is most common in childhood. It manifests itself as redness of the mucous membranes of the throat, gums and tongue. Swelling develops. As the disease develops, areas of white plaque with a cheesy consistency form on the oral mucosa. If treatment measures are not taken, their number increases, and erosions occur under the plaque.
When oral candidiasis becomes chronic, damage to the mucous membranes of the nose, pharynx and esophagus is possible.
to contents ^
Candidiasis of the skin
Fungal pathology can spread in the folds of the skin: in the armpits, under the mammary glands. The folds between the fingers and toes are affected. In some cases, skin lesions outside the folds are noted.
The disease manifests itself in the form of small blisters. Individual areas merge to form affected areas. Between the toes of the limbs there is peeling of the skin, cracks, and itching. Externally, the palms look like they are burned.
to contents ^
Candidiasis of the genital organs
This type of disease affects the external organs of the reproductive system: in women – the vaginal mucosa, in the stronger sex – the glans penis and foreskin. A clear sign of the disease is copious white curdled discharge accompanied by itching. There is discomfort during intimate contact and when urinating.
Candidiasis localized in the intestines
Most often it occurs as a result of previous intestinal infections and the use of antibacterial drugs. In children, this condition can be caused by poor nutrition.
Intestinal candidiasis is manifested by pain in the abdomen, flatulence, diarrhea, and the presence of white cheesy flakes in the stool.
Complications
Medicines for candidiasis must be taken as early as possible, otherwise the disease may become advanced and become chronic. It is dangerous due to numerous complications.
For example, due to urogenital and vaginal candidiasis, diseases of the kidneys, urinary tract, and reproductive organs develop. There may even be infertility, cervical erosion in women, urethritis and prostatitis in men. If such a disease appears during pregnancy, a miscarriage is possible.
With ear candidiasis, sepsis may develop and hearing may deteriorate. With ocular vision, vision drops sharply. With candidiasis of the digestive organs, there is a possibility of developing anemia and peritonitis.
Candidiasis in women
To a greater extent, genital candidiasis occurs among women: about 75% of them have experienced its symptoms at one point. In half of the women who became ill, the disease relapsed.
Candidiasis in women makes itself felt with the following symptoms:
- noticeable milky-white, curd-like vaginal discharge with an unpleasant odor;
- a feeling of itching, irritation, burning, most noticeable after urination and water procedures, as well as before menstruation;
- pain during and after intimate contact.
If a woman ignores such manifestations, the disease can spread to the area of the inguinal folds, affecting the vaginal mucosa and, in some cases, the vaginal area of the cervix.
to contents ^
When to see a doctor
It is necessary to contact a specialist as soon as the first suspicion of candidiasis appears. This applies to symptoms such as mild malaise, discomfort, itching, peeling of the skin, splitting of the nails, redness of the skin and mucous membranes in the mouth, groin, cheesy discharge on the genitals, burning sensation when urinating, vomiting, chest and abdominal pain, diarrhea and etc.
In case of candidiasis, which doctor diagnoses and draws up a treatment regimen for candidiasis depends on the location of the pathological processes. This could be a dermatologist, urologist, gynecologist.
Candidiasis and pregnancy
About 90% of pregnant women suffer from the disease. Such a high prevalence of thrush during pregnancy is due to the fact that in the female body during this period processes occur that give impetus to the active reproduction of the Candida fungus: hormonal levels change, the body’s defense mechanisms decrease, and a lack of vitamins and minerals occurs.
Despite the fact that the disease is diagnosed in the vast majority of pregnant women, a frivolous attitude towards it is unacceptable.
- There is a risk of transmission of Candida fungus to the fetus. This can happen not only during the baby’s passage through the birth canal, but also in utero.
- Infection with the fungus creates conditions for the development of intrauterine oxygen deficiency in the fetus.
- The risk of premature birth, as well as the birth of a baby with low body weight, increases.
- There is a threat of polyhydramnios formation and premature rupture of amniotic fluid.
During pregnancy, the symptoms of candidiasis do not always appear clearly. It is important to carefully monitor the condition of the body, at the slightest suspicion of infection, consult a doctor and not self-medicate.
to contents ^
How the disease is transmitted
Yeast fungi of the genus Candida albicans belong to the opportunistic microflora that lives on the skin and mucous membranes of almost every person who does not have health problems. The activity of the infection is suppressed by the body's protective immune system.
The first acquaintance with Candida fungi occurs during the first year of a child’s life - through contact with an adult, using various household items, eating a certain type of food on the surface of which there are fungi.
A common cause of fungal infection in adults is promiscuity and unprotected sex. Persons who visit swimming pools, baths, saunas and do not observe the rules of personal hygiene are at greatest risk of becoming infected with a pathogenic microorganism.
Candidiasis in men
Representatives of the stronger sex are much less susceptible to candidiasis compared to women. This is due to the anatomical characteristics of the male body.
When affecting the male body, thrush manifests itself as follows:
- There is swelling and redness in the area of the glans penis and foreskin.
- There is a burning sensation and pain when urinating.
- During an erection, intimate contact and after it, pain occurs.
- A white cheesy coating with a sour odor appears.
The appearance of symptoms of candidiasis in a man signals a serious malfunction in the body’s defense system.
Lack of proper treatment in men leads to the development of candidal balanitis (damage to the glans penis) and balanoposthitis (inflammation of the foreskin).
For information about the characteristics of the disease and common myths associated with thrush, watch this video:
to contents ^
Routes of infection
The amount of candida fungus can also increase upon contact with a previously infected person. For example, the causes of candidiasis in this case are as follows:
- during sexual contact (usually in this case the urogenital, vaginal or oral form develops);
- during pregnancy (in this case, the infection is transmitted from mother to child, and he/she develops symptoms of candidiasis at birth);
- during dental procedures (for example, prosthetics - in this case, an adult develops candidiasis in the mouth);
- injuries to the eyes, ears, skin (infection gets into the wounds).
Treatment of candidiasis
The process of getting rid of unpleasant manifestations begins with diagnosis. After examining the patient, a bacterial culture is prescribed - a method that allows one to determine the causative agent of the disease.
During the study, a scraping is taken from the mucous membrane at the site of the lesion. The material is placed in a special environment for several days, where the fungus grows, forming colonies. Based on the data obtained, a final diagnosis is made and a treatment regimen is prescribed.
to contents ^
Drug therapy for candidiasis
For any type of localization of the lesion, complex treatment is required:
Normalization of the immune system: restoration of intestinal microflora, use of immunomodulators.
Elimination of local manifestations of the disease: ointments, suppositories, creams, vaginal tablets (Clotrimazole, Pimafucin, Miconazole).
Systemic treatment: tablets or capsules taken orally (Diflucan).
It is impossible to destroy Candida fungus using antibacterial drugs. Sometimes antibiotics only accelerate the spread of fungal pathology, further disrupting the state of the intestinal microflora.
The process of getting rid of thrush during pregnancy differs from the treatment of this disease in patients of other categories. First of all, it is necessary to exclude the possibility of adverse effects of drugs on the fetus. Therefore, topical agents with low toxicity and absorption, with a minimum number of side effects, are prescribed.
to contents ^
Candidiasis and diet
Human immunity largely depends on the state of the intestinal microflora. With an existing fungal disease, it is almost always impaired. Therefore, to speed up recovery, it is important to follow a diet, which is an element of general treatment.
It is necessary to exclude from the menu foods that contain large quantities of simple carbohydrates: confectionery, sweets, honey, sweet fruits and packaged juices, alcohol.
- The consumption of pasta and starchy vegetables: potatoes, carrots, pumpkin should be limited.
- It is recommended to give preference to lean varieties of meat and fish, stewed, boiled and baked vegetables.
- To normalize the intestinal microflora, you need to include fermented milk products in your menu.
During the treatment of a fungal infection, it is recommended to drink less coffee and tea: the substances contained in them may reduce the effectiveness of antifungal drugs.
to contents ^
Traditional methods in the treatment of candidiasis
There are many popular ways to get rid of unpleasant symptoms, but it should be remembered that they are auxiliary and often minimize pathological symptoms without eliminating the cause of the disease.
- Pour 2 tablespoons of dry calendula (flowers) into 200 ml of boiling water, leave for 40 minutes to infuse. It is recommended to wash the genitals with the strained product. In addition to calendula, you can use celandine, chamomile, oak bark, and yarrow for these purposes.
- Baking soda is a common way to treat candidiasis at home. This substance has a detrimental effect on the fungal habitat. Dissolve 2 tablespoons of baking soda in a liter of boiled water. You can wash the genital area daily with this solution (it is better to do the procedure in the evening). It is important not to leave excess moisture on the genitals after it.
In women, soda procedures should be carried out with caution: this can provoke disturbances in the vaginal microflora.
Therapy with traditional methods and herbal medicine for candidiasis should be carried out in parallel with drug treatment recommended by a doctor.
to contents ^
Modern ideas about fungal pathology of the digestive tract
In gastroenterology, as in other areas of medicine, methods for diagnosing and treating fungal infections are dynamically developing based on the study of physiology, microbiology, pharmacology, molecular pathology and medical genetics. Already known variants of the disease are studied in detail and rare and new nosological forms are described.
Fungi, being normal commensals of the gastrointestinal tract (GIT), become pathogenic under certain conditions. This applies mainly to yeast-like fungi Candida spp., the species and even strains of which differ in factors of aggression, ability to adhere and invade [15].
Candida albicans is the most common causative agent of gastrointestinal candidiasis. However, in recent years, Candida non-albicans (C. krusei, C. tropicalis, C. kefyr, C. glabrata, C. parapsilosis) have played an important role; in persons with immunodeficiency their proportion is more than 50%, with “relatively normal” immunity - 15%.
Candida fungi (opportunistic microorganisms) colonize the gastrointestinal tract - this phenomenon is called colonization - the process is asymptomatic. A study of healthy adult volunteers found that Candida albicans was present in the oropharyngeal area in 20–30% of them, in the small intestine in 50–54%, in the large intestine in 55–70% and in feces in 65–70% [ 9, 13]. A study of the composition of the oral microflora in the population of several European countries revealed the presence of fungi in 10–25% of people, and in stool in 65–80% [11, 17]. Colonization of the pharynx by Candida fungi in patients with hematologic malignancies has been studied in detail: it was 33% [8]. In biopsy specimens of gastroduodenal ulcers, yeast-like fungi are found in 17–30% of cases [12]. In 50% of German residents, fungi are present in the intestinal microbiota, and in hematologic cancer patients, intestinal colonization is 63–65% [10, 11]. We must not forget that in 0.8–4% of patients, fungi are accidentally detected in the cystic and ductal bile, and in case of cholelithiasis - in 15–20%.
The asymptomatic presence of fungi in the gastrointestinal tract may cease when they acquire pathogenic properties. Thus, in patients with neutropenia, fungi from the intestines can disseminate to the liver, spleen and lungs, and in a catheter-associated situation, fungi enter directly into the bloodstream, reaching the heart and kidneys.
The yeast-like fungus Cryptococcus neoformans plays a minor role in gastrointestinal pathology as an etiological factor. It most often affects the nervous system and, disseminating from the primary focus, involves the gastrointestinal tract. Isolated cases (usually postmortem) of cryptococcal esophagitis, stomatitis, terminal ileitis, colitis, cholecystitis, and pancreatitis have been described. As a rule, they belonged to HIV-seropositive patients, as well as to patients suffering from hypergammaglobulinemia E with recurrent abscesses of the liver and perianal area.
Gastrointestinal diseases caused by dimorphic pathogenic fungi (pathogenicity group II) have been reported in South America, but occasionally occur as sporadic cases throughout the world. Most dimorphic fungi in nature exist in a mycelial form; once in the body, they are transformed into yeast-like ones and acquire pathogenic properties. The oral route of penetration is not typical; these fungi enter the gastrointestinal tract through dissemination from other organs. Blastomyces dermatitidis produces granulomatous lesions in the stomach and small intestine. Coccidioides immitis, Histoplasma capsulatum, Paracoccidioides brasiliensis and Sporothrix schenckii infect the intestine only when disseminating from skin lesions and the respiratory tract [6, 15].
Fungi Aspergillus spp. rarely cause gastrointestinal disease, only in cases of persistent neutropenia, cachexia and other aggravating conditions.
Fungi of the Zygomycetes class can lead to the development of intestinal zygomycosis, which is usually associated with amebiasis, starvation, diabetic ketoacidosis, and renal hemodialysis. Penicillium spp. and Geotrichum also rarely affect the gastrointestinal tract.
Yeast-like, mold and some dimorphic fungi are opportunistic, opportunistic microorganisms that are widespread in the environment and can easily enter the skin, mucous membranes of the oral cavity, genitals and the respiratory tract. In addition, fungi are characterized by an endogenous mode of existence (mycocarriage).
The gastrointestinal tract is covered with a mucous membrane, consisting of two components - a superficial slippery, mucous layer through which microorganisms easily move along the entire gastrointestinal tract, and a deeper dense glycoprotein layer with sialic acid residues, which forms a physiological barrier. Adhesion and subsequent invasion of fungi through this dense layer are possible only due to the production of proteolytic “invasion enzymes” by fungi: coagulase, catalase, caseinase, phospholipase, as well as fibrillar protein complexes and endotoxins [15].
With physiological well-being, there is a certain balance between macro- and microorganisms, in which, on the one hand, factors of the body’s resistance to microscopic fungi play a role, and on the other, factors of the pathogenicity of fungi.
The body's resistance depends on membership in risk groups and the state of the immune system.
Let us list the risk factors for the development of fungal infections of the gastrointestinal tract.
- Damage to the mucous membranes of the oral cavity (lichen planus, dentures, trauma, xerostomia, use of hormonal inhalers).
- Chronic gastrointestinal diseases (atrophic gastritis, gastric hypoacidity, achalasia, bulbitis, erosive and ulcerative diseases of the esophagus and intestines, diverticulosis, polyposis, gastroesophageal reflux disease, enterocolitis, Crohn's disease, irritable bowel syndrome, stomach contamination with Helicobacter pylori, dysbiosis, mixed intestinal infection ).
- Trauma to the mucous membrane (burns, esophagogastric tube, endotracheal intubation).
- Pregnancy.
- Newborn period (prematurity, massive infection when passing through the birth canal, natural imperfection of the immune system).
- Old age (aging of the immune system, concomitant diseases, decrease in the amplitude of longitudinal contractions of the esophagus, the strength of sphincter contractions, impaired absorption processes, etc.).
- Oncological and hematological diseases (neutropenia).
- Endocrinopathies (especially diabetes mellitus).
- AIDS, HIV infection.
- Transplant operations.
- Conditions requiring stay in intensive care units.
- Severe allergic diseases.
- Taking antibiotics, cytostatics, hormones and other chemotherapy drugs in inadequate doses.
- Eating disorders, including fasting for the purpose of weight loss.
- Alcoholism, smoking, drug addiction.
An important component of defense against gastrointestinal invasion is the gut-associated immune system. The cellular part of this system includes intraepithelial lymphocytes, which prevent the pathogen from dispersing through the lamina propria and aggregating in Peyer's patches. Intestinal B lymphocytes are involved in the production of secretory IgA and IgM, which reduce the ability of fungi to adhere.
T cells of a healthy body produce protective interferon, enhance phagocytosis, and activate T-cytotoxic lymphocytes. CD4 and CD8 strengthen local immunity in the gastrointestinal tract. Moreover, it turned out that the cytotoxicity of CD8 plays a more significant role in preventing the disease than previously thought.
Macrophage and neutrophil phagocytosis are also important in protection, preventing the dissemination of fungal, especially candida, infections.
In HIV patients and patients with neutropenia, in whom phagocytosis is sharply suppressed, local invasion and dissemination of the infection occur very quickly. It is known that neutrophils, although they cannot completely protect the gastrointestinal mucosa from the “attack” of fungi, but thanks to their own “killer” substance, through a specific mechanism, they trigger the activation of complement, which enhances phagocytosis. It should be noted that phagocytosis is especially important during candida infection, but “does not work” in tissues against encapsulated cryptococci and most filamentous fungi.
Normal biochemical, histochemical and physiological processes in the gastrointestinal tract, timely regeneration of epithelial cells, acid-enzyme barrier, and full peristaltic activity are also protective factors that prevent the penetration of fungal and bacterial flora [4]. The role of stomach acid in preventing the introduction of fungi into the mucosa is undeniable. In an environment with low acidity, Candida fungi acquire pathogenic properties, vegetative forms appear, and pseudomycelium or mycelium is formed, damaging the mucous membrane. In HIV-infected individuals, who are characterized by achlorhydria, ingested Candida fungi can cause gastric candidiasis, while in people with normal immunity this localization is rare. The role of gastric acidity in the development of bacterial and fungal infections of the intestine has not been confirmed.
Obligate microorganisms of the stomach and intestines (aerobic lactobacilli, anaerobic bifidum bacteria, normal E. coli, etc.) also play a protective role. The use of antibiotics kills, along with pathogenic ones, these “beneficial” bacteria, opening adhesion receptors for fungi on the mucous membrane [2].
It is also impossible not to mention Helicobacter pylori, which quite often lives in the stomach, causes gastritis, peptic ulcers, and sometimes has a carcinogenic effect. In turn, treatment of helicobacteriosis with antibiotics leads to activation of Candida fungi and gastric candidiasis [1]. Associations of fungi with Helicobacter pylori and other bacteria in the gastrointestinal tract are common, which requires a thoughtful, adequate approach to treatment tactics.
The stomach may also contain Saccharomyces cerevisiae and some species of Candida, which can ferment and ferment sugars that enter the stomach with food into wine alcohol. This phenomenon is called the “brewery” syndrome [14].
Virulence of fungi, pathogenic factors, as well as polysaccharides (mannans), plasmacoagulase, endotoxins, lipids, glucoconjugates, influence the development of the disease. Even the intraspecific abilities of fungi determine whether candidiasis or disease will develop in each particular case [13]. For example, serotype B of Candida albicans is considered to be more virulent and the most common causative agent of oropharyngeal candidiasis in HIV-infected patients; it also affects the genitourinary system and is often isolated from the pharynx of homosexuals.
Microscopically, the factors of aggression of Candida fungi are manifested by the formation of germ tubes, pseudohyphae and true mycelium - due to them, fungi can grow into the wall of phagocytes. However, yeasts that are not able to produce mycelium, such as Candida glabrata, Cryptococcus neoformans, can also cause gastrointestinal diseases.
Diagnostics
A thorough study of the medical history, identification of risk factors, chronic gastrointestinal diseases, and pathognomonic clinical symptoms play a big role in the timeliness of diagnosis.
In recent years, endoscopic technologies have expanded the possibilities for diagnosing fungal esophagitis and gastritis. During esophagogastroduodenoscopy, attention is paid to hyperemia and ulceration of the mucous membrane, the presence of white deposits and “films”, narrowing of the lumen of the esophagus, and accumulation of mucus. During this procedure, it is imperative to take material for microbiological examination, since the etiology of these manifestations is not always fungal. Moreover, the information content of plaque research is higher than that of biopsy specimens (95% compared to 39%).
Video information endoscopic studies with digital recording and image analysis are especially promising. A clear distinction between unchanged and pathological tissues and analysis of histochemical processes in the mucous membrane of the digestive tract are possible using endoscopic spectroscopy and fluorescence endoscopy. Video and colonoscopy, chromoendoscopy against the background of “medicinal” sleep using Diantek technology have a high quality of research, painless manipulations and the absence of stress and fear in patients.
It should, however, be emphasized that invasive manipulations with inflamed gastrointestinal mucosa are unsafe, can promote fungal and bacterial dissemination, and sometimes lead to injury and perforation of the wall of the esophagus or stomach. Endoscopic ultrasonography with Doppler mapping and contrast enhancement of tissue and vascular structures is promising; it allows detailed differentiation of all layers of the wall of the digestive tract. Non-invasive methods - virtual endoscopy, which allows obtaining a three-dimensional image, magnetic resonance imaging - have a great future [3].
Studying gastroduodenal motility using scintigraphy and electrogastrography is also important for diagnosis and prescribing additional medications, since impaired motor function of the stomach and “stagnation” in the gastrointestinal tract create conditions for the proliferation of fungi and bacteria. Colonoscopy makes it possible to assess the condition of the intestinal mucosa, the presence of white plaque, ulcerative defects, etc. In the future, methods based on new scientific and practical research will be introduced in gastroenterology: enzyme immunoassay of fecal antigens, PCR and even genetic testing [3] .
Another fairly informative method in gastroenterology is radiography of the esophagus, stomach and intestines. It makes it possible to identify filling defects (barium depot), ulceration, deformation, convergence of folds, changes in the contours and depth of peristalsis, narrowing or expansion of the esophageal tube. Using X-rays of the stomach, you can evaluate its motility and the timeliness of evacuation of the food bolus, which is important for understanding the pathogenesis of the disease.
| Figure 1. Candidal esophagitis. Budding cells and pseudohyphae of Candida albicans fungi on an esophageal ulcer |
| Figure 2. Candidal enteritis. Thickened villi and defect of the small intestinal mucosa; pseudohyphae of Candida fungi |
Laboratory confirmation of a fungal disease of the gastrointestinal tract is possible through microscopy and/or cultural examination of swabs from the mucous membranes of the oral cavity and esophagus, the contents of the stomach and intestines, pathological “films”, plaque, etc. Quantitative assessment of fungi in biosubstrates should be carried out in comparison with clinical symptoms, with taking into account the presence of background diseases, mixed infections, etc. For example, the detection of single Candida colonies on the mucous membranes is not a basis for diagnosing candidiasis in immunocompetent patients.
In stool, the number of colonies (more than 105–106) acquires diagnostic significance. Culture results are interpreted differently, with a lower diagnostic threshold, in immunosuppressed individuals, neutropenic patients with AIDS, and in intensive care units. You should also pay attention to the ability of fungi to vegetate and form mycelium, as this is one of the laboratory signs that confirm the diagnosis of candidiasis.
Histological (Gomori-Grokkot staining, PAS reaction) and cytological (Romanovsky-Giemsa staining) studies of biopsy specimens make it possible to detect tissue forms of fungi. Many authors consider these methods to be the most reliable. In addition, mycelium and pseudomycelium in tissues confirm the presence of an invasive form of fungal infection of the gastrointestinal tract (Fig. 1, 2).
Candidiasis
This is the most common fungal opportunistic visceral pathology. The aggressive properties of Candida fungi are manifested in their ability, through the stage of adhesion and invasion, to infect the mucous membranes of any organs, including the gastrointestinal tract. Moreover, the stratified squamous epithelium of the oral cavity and esophagus is most often subject to “attack”, and less often the single-layer cylindrical epithelium of the intestine. Therefore, as a rule, in the upper parts of the gastrointestinal tract, invasion of Candida fungi occurs, and in the parts located below the stomach, colonization occurs. At the same time, in the intestine, even at the adhesion stage, clinical symptoms can be observed - manifestations of non-invasive candidiasis [10].
Ulcerative defects of the esophagus, stomach and intestines support fungal colonization up to invasion. Gastrointestinal candidiasis often leads to candidemia.
Classification of candidiasis
I. Oropharyngeal candidiasis.
- Oral candidiasis in newborns.
- Pseudomembranous candidiasis.
- Atrophic candidiasis of the oral cavity (more often in the elderly).
- Erythematous candidiasis (new form).
- Median rhomboid glossitis.
- Leukoplakia associated with candidiasis.
- Angular candidal cheilitis.
- Candidal gingivitis (rarely occurs in isolation).
II. Candidal esophagitis.
- No erosion.
- With erosions.
III. Stomach candidiasis.
- Erosive-fibrinous gastritis (diffuse).
- Secondary candidiasis against the background of peptic ulcer.
- IV. Intestinal candidiasis.
- Pseudomembranous.
- Collagen.
- Lymphocytic.
V. Candidal proctosigmoiditis.
VI. Perianal candidiasis.
VII. Secretory diarrhea associated with candidiasis.
| Figure 3. Candidal glossitis. Typical white plaques and erosions on inflamed infiltrated mucosa |
Among all localizations of candidiasis of the digestive tract, oropharyngeal takes 1st place (Fig. 3).
Hippocrates mentioned oral candidiasis, and it was first described by the surgeon Langenberg in 1839.
Candidal stomatitis in newborns is a common disease. In the first days after birth, the baby’s mucous membranes are resistant to fungi.
Subsequently, insufficient secretion of IgA and a gradual decrease in antimicrobial immunity transmitted from the mother lead to high morbidity. The pathognomonic syndrome is white cheesy deposits on the oral mucosa, the so-called “thrush” [16].
Candidiasis is also associated with wearing dentures. In this case, atrophic candidiasis develops, a huge number of fungi accumulate in the cheek folds against the background of red point inflammation of the mucous membrane; Infestation is usually absent.
Candidal esophagitis in general hospitals occurs in 1.3–2.8% of patients, in transplant departments - up to 4%, with disseminated carcinomatosis - from 2.8 to 6.7%. This disease often occurs without subjective complaints and is detected accidentally during “continuous” studies of the population in 1–7% of cases [5, 17]. Sometimes patients note pain and discomfort when passing solid and liquid food, dysphagia, and hypersalivation. According to the depth of the lesion, four types are endoscopically distinguished - from mild edema, hyperemia, single white plaques < 1 mm in diameter to massive inflammation, deformation and bleeding of the mucosa, ulceration, even perforation.
Gastric candidiasis, as a rule, develops secondary to peptic ulcer and gastroesophageal reflux disease. Achlorhydria, in turn, promotes the colonization of fungi on the mucous membrane, with subsequent invasion, especially in defect areas (ulcers, erosion), which slows down repair, pain syndrome appears, and sometimes bleeding of the ulcer is noted.
Candidiasis of the intestine usually manifests itself as abdominal discomfort, diarrhea, bloating, pain and other symptoms. The study of intestinal microbiocenosis allows us to specify amorphous “enterocolitis”, namely to differentiate pseudomembranous colitis caused by Clostridium difficile, an acute process in the intestine caused by rotoviruses and Escherichia coli, from candidiasis or dysbiosis with a predominant candidal component.
Fungal infection of the biliary system is facilitated by previous biliary dyskinesia, dyspancreatism, giardiasis, cholestasis, hypotension of the gallbladder and other lesions. Under these conditions, favorable conditions are created for the proliferation of fungi and other microorganisms. The cause of candidal cholecystitis can be bile duct stones, which are often a “reservoir” of fungi; some authors even call them “fungal bodies” or “candidal stones”.
Mycoses of the biliary tract are more common than is commonly believed. Microbiological examination of portions of bile obtained through multifractional duodenal intubation makes it possible to differentiate fungal from bacterial or functional pathology of the duodenum, gallbladder, biliary tract and liver.
Treatment
Treatment of candidiasis of the digestive tract, as well as other fungal infections, should be complex and etiopathogenetic.
If complaints from the gastrointestinal tract appear, the patient should first of all follow a strict diet and give up bad habits.
It is necessary to take medications aimed at eliminating factors predisposing to the development of candidiasis and correcting concomitant diseases.
- If candidiasis is suspected that has developed against the background of nonspecific ulcerative colitis, Crohn's disease, or chronic inflammation of the intestinal wall, glucocorticosteroids with minimal systemic effect and “mild” immunomodulators are selected.
- Treatment of peptic ulcer and gastroesophageal reflux disease is carried out with antisecretory drugs benzimidazole derivatives - inhibitors of the proton pump of parietal cells (Nexium, Pariet, Lanzap); as well as blockers of histamine H2 receptors (quamatel, ulfamid, ulceran, gastrosidin, famosan).
- In order to prevent the reflux of stomach contents into the esophagus, the tone of the lower esophageal sphincter and the motor activity of the gastrointestinal tract are increased by prescribing modern drugs - antagonists of serotonin 5-HT4 receptors.
- The functional disease “irritable bowel syndrome” is treated with somatostatin analogues, kappa antagonists.
- Anti-Helicobacter therapy with omeprazole, amoxicillin, tinidazole, etc. is carried out with great caution, since Helicobacter pylori often exists in association with Candida spp. fungi, and the latter are sharply activated during antibiotic therapy.
Antifungal therapy is necessary. The list of antifungal agents is updated every year with new effective drugs. Among modern antimycotics, several groups are distinguished.
- Polyenes: amphotericin B (amphoglucamine), lipid complex Ampho B (ampholip), liposomal Ampho B (ambisome), colloidal dispersion Ampho B (amphocil).
- Triazoles: fluconazole (Diflucan), voriconazole (Vfend), ravuconazole (in clinical trials), itraconazole (Orungal), posaconazole (in clinical trials), albaconazole (in clinical trials).
- Allylamines: terbinafine (Lamisil).
- Echinocandins: caspofungin (Cancidas), micafungin, anidulafungin (in clinical trials).
Long-term observations conducted at the Center for Deep Mycoses and devoted to the effectiveness of treatment of fungal diseases of the digestive tract (more than 150 patients) allow us to identify the most effective adequate etiotropic drug from the general range of drugs. This is an antimycotic from the group of triazoles - fluconazole (Diflucan, Diflazone, Flucostat), used in the treatment of yeast-like infections of the gastrointestinal tract (candidiasis, cryptococcosis). It has the highest efficiency, which is based on inhibition of the cytochrome P-450 system and subsequent disruption of ergosterol synthesis in the cell membrane of the yeast-like fungus. Due to its high bioavailability, active absorption in the gastrointestinal tract, and no effect on the synthesis of testosterone and cortisol, fluconazole is well tolerated and does not cause side effects. The drug has a unique ability to penetrate the blood-brain barrier, which is especially important in the case of dissemination of a fungal infection from the gastrointestinal tract into the blood and central nervous system.
When administered per os, the absorption volume of fluconazole in the digestive system is more than 90%, and the degree of its resorption is high even with achlorhydria, which distinguishes this triazole from polyenes and other azoles. The drug does not have a negative effect on absorption processes in the intestines when taken together with antacids. The highest concentration of the drug in plasma when taken orally or intravenously is achieved after 0.5-1.5 hours. At the same time, the half-life is long - 30 hours, and the percentage of binding to plasma proteins is low - 11-12%. The absence of toxic effects of fluconazole is explained not only by weak binding to proteins, but also by a large volume (79.6%) of its excretion through the kidneys in the urine unchanged.
Currently, fluconazole is represented on the Russian market in 18 generic copies, which have similar pharmacokinetic characteristics and are well tolerated by patients. However, in terms of clinical and mycological effectiveness, some of them are somewhat inferior to the original fluconazole - Diflucan.
Fluconazole is available in three forms:
- solution of 50, 100 and 200 ml in a bottle for intravenous use (2 mg/ml);
- gelatin capsules of 50, 100, 150 and 200 mg;
- powder in a bottle for the preparation of 60 ml of suspension with orange flavor for oral administration (50 mg/5 ml).
We have developed complex treatment regimens for candidiasis of the digestive tract, taking into account the location, depth of the lesion, the state of immunoprotective forces, and the presence of aggravating diseases. Fluconazole, which was prescribed to adults at a dose of 2–2.5 mg/kg, an average of 100–150 mg per day, for 2–3 weeks, was given etiotropic significance in this scheme. On the first day the dose was doubled.
Pediatric dosages: for newborns - 7–12 mg/kg per day; for children of preschool and school age 50–100 mg/day; the course of treatment was 7–14 days.
Thus, as our practice has shown, for systemic mycoses, including gastrointestinal candidiasis, fluconazole solution for intravenous administration and suspension are used more often than capsules.
The causes of the development of pathology of the digestive system are diverse, and clinical symptoms are variable. Fungal infections caused by yeast-like, mold and dimorphic fungi account for 8–10% of the total number of gastrointestinal diseases, and up to 80% of the population is colonized by fungi. HIV-infected people and patients with neutropenia are especially susceptible to the disease. Modern endoscopic and radiological methods are used for diagnosis. Conduct a microbiological study of biosubstrates to determine the etiology of the disease. The most common fungal infection of the gastrointestinal tract is candidiasis. The treatment regimen for fungal pathology of the digestive tract includes the prescription of an effective, non-toxic antimycotic, anti-inflammatory, restorative and immunomodulatory agents. Therapy should be carried out against the background of a diet; patients need clinical observation.
Literature
- Bazhenov L.G. et al. The role of fungi of the genus Candida in the microbiocenosis of the stomach during helicobacteriosis // Uspekhi med. mycology. - 2003. - T. I. - pp. 8-9.
- Burova S. A. Features of the course and therapy of fungal infections in children // Doctor. RU. - 2003. - December. — P. 24-25.
- Ivashkin V. T., Lapina T. L. Gastroenterology of the 21st century// Breast cancer. - 2000. - T. 8. - No. 17 (118). — P. 697-703.
- Lazebnik L. B. Aging of the digestive tract and polymorbidity: Lecture for practitioners. doctors//XI Ross. National Congress "Man and Medicine". - 2004. - P. 331-341.
- Lessovoy V.S., Lipnitsky A.V., Ochkurova O.M. Oral candidiasis // Problems of medicine. mycology. - 2003. - T. 5. - No. 1. - P. 21-26.
- Lessovoy V. S., Lipnitsky A. V., Ochkurova O. M. Mycoses of the digestive tract // Problems of honey. mycology. - 2004. - T. 6. - No. 2. - P. 19-23.
- Petrova N. A., Klyasova G. A., Sharikova O. A. Colonization of the pharynx mucosa with yeast fungi in patients with hemoblastosis // Advances in medical sciences. mycology. - M., 2003. - T. 1. - P. 28-29.
- Sergeev A. Yu., Sergeev Yu. V. Candidiasis of the gastrointestinal tract. - M., 2000. - P. 322-345.
- Tolkacheva T.V. et al. Frequency of isolation and species spectrum of yeast fungi in the intestines of patients with hematological malignancies // Uspekhi med. mycology. - 2003. - T 1. - P. 30-32.
- Shevyakov M. A. Candidiasis of the mucous membranes of the digestive tract // Problems of honey. mycology. - 2000. - T. 2. - No. 2. - P. 6-10.
- Shevyakov M. A. Diagnosis and treatment of gastric candidiasis // Problems of honey. mycology. - 2002. - T. 4. - No. 2. - P. 50.
- Cohen R. et al. Fungal flora of the normal human small and large intestine. New E et al Candida infection of the gastrointestinal tract. Medicine, 1972; 51: 367-369.
- Gazzard B. Fungal infection of the gastrointestinal tract. Principles and Practice of Clinical Mycology. Edited by CC Kibller et al., 1996: 165-177.
- Hanss H., Hanss R. Heien in Derm die heimliche gefahr // Haufman Pediatrie. - 1994; 6; 1:56-57.
- Levine J., Dycoski RD, Janoff EN Candida — associated diarrhea: a syndrome in search of credibility // Clin. Inf. Dis. - 1995; 21: 881-886.
- Odds FC Candida and Candidiasis. Bailliere Findall, 1988. London.
S. A. Burova , Doctor of Medical Sciences, Professor
National Academy of Mycology, City Clinical Hospital No. 81, Moscow