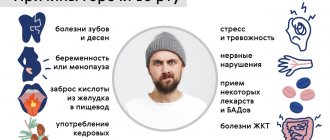
Top 5 Causes of Bad Breath
Frequent communications with other people are an integral part of modern life. While bad breath can cause “forced silence.” How to avoid becoming an introvert against your will? And where to look for the cause of the trouble?
1. Insufficient hygiene and dental diseases
Food debris on teeth and gums provides food for oral bacteria. And the “waste” of such a diet becomes volatile compounds (ammonia, hydrogen sulfide and others), a large concentration of which is felt as an unpleasant odor.
In addition, such conditions contribute to the proliferation of pathogenic flora, which:
- firstly, it disrupts the pH of the oral cavity (due to bacterial waste products) and promotes demineralization of enamel and tooth tissue itself;
- and secondly, it increases the concentration of volatile substances in the oral cavity and contributes to the appearance of an unpleasant odor.
Thus, both improper hygiene and excess bacteria and signs of inflammation in gum disease, even with good hygiene, may be to blame for the appearance of a “problematic” odor.
In the first case, normal hygiene procedures twice a day, as well as rinsing after meals during the day, are sufficient to eliminate the problem. And in the second, the solution obviously requires the participation of a dentist.
Dry oral mucosa
This phenomenon often occurs while taking certain medications and is caused by insufficient saliva production.
In this case, the cleansing properties of saliva practically disappear, which contributes to the “accumulation” of food debris in the oral cavity and their “decomposition”, and also significantly “makes life easier” for bacteria.
Chronic diseases of the respiratory system
Chronic tonsillitis, pharyngitis, and sinusitis are a reliable source of excessive growth of bacteria in the oral cavity. Here we are most often talking about staphylococci and streptococci, which have pronounced pathogenic properties.
An unpleasant odor can also appear with purulent diseases of the bronchi and lungs, as well as with tumors at the stage of destruction. In this case, the smell from the mouth often becomes putrid in nature, and the cough is accompanied by copious sputum production.
Digestive system diseases
“Stomach” odors are often sour (with normal and high acidity) or “rotten” in nature (with low acidity), and appear under the following conditions:
- reflux of stomach contents back into the esophagus (reflux),
- narrowing of the gastric outlet (pyloric stenosis),
- the presence of ulcerative and oncological processes in the stomach or duodenum.
The smell can also be associated with liver damage, and then it has a characteristic “liver” tint.
Severe metabolic disorders
We are talking primarily about diabetes mellitus and its severe complication – ketoacidosis. The smell from the mouth in which case resembles “acetone”, and the condition itself can be fatal.
How to find the reason
1. You can confirm the “microbial” origin of bad breath by inoculating a swab from the throat and nose. The study will not only “show” the quantity and quality of microorganisms, but will also allow you to select an effective antibacterial drug, if necessary.
Culture is also relevant for sputum, if it is separated.
And also, in any case, an examination by a dentist and an ENT doctor is recommended.
2. It is quite difficult to check the condition of the stomach and duodenum using laboratory methods, therefore, if a “gastric” origin of the odor is suspected, a consultation with a gastroenterologist and FGDS is recommended.
3. The liver is one of the most multifunctional organs, so it is not surprising that many people experience its damage at a young age.
You can check the digestive function of the organ using a blood test for liver enzymes (ALT, AST), bilirubin, alkaline phosphatase and gamma-GT, both individually and in the format of the Liver Examination complex. Base".
4. A blood test for glucose levels and glycated hemoglobin (average level over the last 3 months) is “meant” to control the risk of diabetes.
HEPATIC ENCEPHALOPATHY in the practice of an emergency physician
What clinical symptoms allow one to diagnose PE? What are the manifestations of neurological disorders at different stages of development of PE? What are the features of the development of PE in alcoholism? What mistakes should a doctor avoid when treating PE?
Etiology and pathogenesis
Hepatic encephalopathy (HE) is a potentially reversible disorder of nervous and mental activity that occurs in any liver disease that occurs with insufficiency of hepatic cellular function. In most cases, PE complicates the course of the terminal stage of chronic diffuse liver diseases or acute necrotizing (fulminant) hepatitis. It has been established that with liver damage of any etiology, PE can lead to the development of coma and become the direct cause of death of the patient (see Table 1).
| Table 1. Causes of development of PE. | ||
| Encephalopathy variant | Survival | Etiology |
| Acute encephalopathy without liver fibrosis/cirrhosis | 20–45% | Viral hepatitis. Alcoholic hepatitis. Acute poisoning (chemical and biological poisons, drugs). Withdrawal syndrome |
| Acute encephalopathy due to fibrosis/cirrhosis of the liver | 70-80% | Forced diuresis Vomiting, diarrhea Bleeding Gastrointestinal tract Infections Alcohol intake Withdrawal syndrome Constipation Excess protein in the diet Surgical interventions Taking sedatives |
| Chronic portosystemic encephalopathy in end-stage liver disease | 100% | Portosystemic shunting Intestinal contamination Excess protein in the diet |
| Figure 1. Mechanism of development of PE. |
The pathogenesis of PE is not fully established. It is believed that the development of HE is the result of a combined effect on the central nervous system of several mechanisms, the activity of which is initiated and maintained by a pronounced impairment of the hepatic clearance of toxins and metabolites (see Figure 1). The most important factors for the development of PE are considered to be:
- a rapidly increasing increase in plasma ammonia concentration;
- an increase in plasma concentration and an imbalance between the synthesis and catabolism of neurotransmitters and their precursors in the central nervous system.
Clinical symptoms and diagnosis of PE. The type and amount of excess, “toxic” metabolites circulating in the plasma and central nervous system, to varying degrees, correlate with various symptoms of PE, which include:
- disturbance of consciousness;
- personality change;
- intellectual disorder;
- actual neurological disorders (see Table 2).
| Table 2. Glasgow Consciousness Scale (GCS). | ||
| Symptom | Symptom severity | Point |
| Consciousness | oriented | 5 |
| confusion/lethargy | 4 | |
| Verbal reaction | the answer is out of place | 3 |
| slurred sounds | 2 | |
| No answer | 1 | |
| executes commands | 6 | |
| purposeful response to pain | 5 | |
| undirected response to pain | 4 | |
| Motor reaction | flexion response to pain | 3 |
| extensor response to pain | 2 | |
| no reaction | 1 | |
| spontaneous | 4 | |
| Eye reaction | per voice | 3 |
| for pain | 2 | |
| No | 1 | |
| Total indicator (10–15 points): stupor, 5–10 points: precoma, 0–5 points: coma. | ||
Mechanism of development of PE
Early signs of disturbances of consciousness (US) in PE include a decrease in spontaneous movements, a fixed gaze, lethargy, and apathy. Impaired consciousness in PE is, in principle, characterized by drowsiness and inversion of the normal rhythm of sleep and wakefulness. In this case, deterioration of the condition and transition from drowsiness to coma can occur within a very short time. To determine the degree of NS, the Glasgow scale is often used (see Table 2). However, in clinical practice, to assess the depth of NS specifically in PE, a simpler qualitative scale is used, according to which:
- Stage I of NS is characterized by weakened concentration, euphoria and anxiety;
- stage II is characterized by the appearance of drowsiness, disorientation, personality changes and inappropriate behavior;
- at stage III of NS, stupor, hypersomnia and confusion develop, but the patient can follow simple commands and pronounce words clearly;
- with IV degree NS, the patient falls into a coma and contact with him is impossible.
Neurological disorders in PE are generally not specific and can also develop with uremia, severe respiratory and heart failure. However, one of the most pathognomonic neurological symptoms of PE is considered to be the development of “flapping” tremor (asterixis), the distinctive feature of which is the patient’s inability to maintain a fixed position. The greatest severity of hyperkinesis of the muscles of the limbs when maintaining a constant posture and its decrease during movement make it possible to differentiate asterixis from tremor in alcoholic delirium and neuroencephalopathy.
The most reliable way to determine the degree of intellectual impairment in PE is to conduct a number-binding test (Reitan test). Changes in personality and intelligence in PE are the most difficult to diagnose, since they are always superimposed on constitutional, previously acquired disorders and always require dynamic assessment. The greatest difficulties in clinical practice are encountered in the differential diagnosis of PE and personality disorders that develop with chronic alcohol abuse (toxic or alcoholic encephalopathy, the presence of which does not directly affect the outcome of acute PE, but determines the risk of developing delirium against the background of alcohol withdrawal syndrome). It is important that in alcoholism, acute PE can develop with any of the clinical and morphological forms of alcoholic liver disease (see Figure 2).
| Figure 2. Natural history of alcoholic liver disease in chronic alcohol abuse. |
PE in patients with alcoholism generally has the same characteristic signs as in other cases, however, they often have muscle rigidity, hyperreflexia, and foot clonus. Alcoholic delirium differs from “pure” PE by prolonged motor agitation, increased activity of the autonomic nervous system, insomnia, frightening hallucinations and rapid small tremor (see Table 3). Severe anorexia is often observed, accompanied by nausea and vomiting.
| Table 3. Characteristic features of HE and delirium in alcohol withdrawal syndrome. | |
| Hepatic encephalopathy | Alcohol delirium |
|
|
A characteristic feature of PE is the variability of the clinical picture. It is easy to diagnose PE, for example, in a patient with liver cirrhosis,
with massive gastrointestinal bleeding or sepsis, the examination of which reveals confusion and flapping tremor. In cases where obvious causes of deterioration cannot be identified and there are no signs of liver cirrhosis, it is impossible to recognize the onset of PE unless due importance is given to the subtle signs of the syndrome. Anamnesis data obtained from family members who have noticed changes in the patient’s condition or behavior can be of great importance.
In patients with acute PE without signs of chronic portal hypertension (varicose veins of the anterior abdominal wall, edematous-ascitic syndrome, splenomegaly, liver disease or a history of alcoholism), prehospital diagnosis is especially difficult. In these cases, it should be based, firstly, on a thorough examination of the anamnesis, if possible; secondly, to analyze the effectiveness of standard nonspecific therapy for coma. Differential diagnosis in patients without cirrhosis of the liver must be carried out with a number of diseases leading to a sudden and severe impairment of consciousness (see Table 4).
| Table 4. Causes of acute disturbances of consciousness in patients without signs of portosystemic shunting. | ||
| Disease | Characteristic symptoms and anamnestic data | Emergency treatment |
| Hypoglycemia | History of hypotension, bradycardia, diabetes mellitus or hypoglycemic therapy | Administration of concentrated dextrose |
| Acute alcohol poisoning | Smell of alcohol, hypertension, shortness of breath, facial flushing, tachycardia, indications of alcohol intake | Massive infusion and maintenance therapy |
| Alcohol withdrawal syndrome with delirium | Chronic alcohol abuse, last alcohol intake no more than three to five days ago, acute psychosis with agitation and hallucinations | Administration of mannitol, concentrated glucose and diazepam, maintenance therapy |
| Acute diazepine poisoning | Profound disturbance of consciousness, indication of psycho-emotional problems, suicide attempts | Administration of flumazenil, maintenance therapy |
| Acute paracetamol poisoning | Indication of recent inflammatory disease, psycho-emotional problems, suicide attempts | Administration of acetylcysteine, maintenance therapy |
| Acute opiate poisoning | Indication of drug addiction, symptoms of opiate intoxication | Administration of naloxone, maintenance therapy |
| Wernicke's encephalopathy | Nystagmus, bilateral paresis of the abductor muscles, indications of fasting, history of alcoholism | Administration of thiamine |
| Intracranial pathological processes (trauma, heart attack, aneurysm, meningitis, encephalitis) | Anamnestic indications, characteristic symptoms, lack of effect from emergency treatment of coma | Maintenance therapy, emergency hospitalization |
| Endogenous intoxications and hypoxic conditions (uremia, ARDS, acute infectious diseases) | Anamnestic indications, characteristic symptoms, lack of effect from emergency treatment of coma | Maintenance therapy, emergency hospitalization |
In patients with liver cirrhosis and active portosystemic shunting, the most important diagnostic issue is also to determine the causes that led to the development of PE (see Table 5).
| Table 5. Factors contributing to the development of acute HE in liver cirrhosis. |
Metabolic:
|
Bleeding and blood loss:
|
Influence of chemical and pharmacological factors:
|
Infectious diseases:
|
| Constipation |
| High Protein Diet |
In most cases, any of the above factors either directly suppresses the functions of the central nervous system or disrupts them indirectly - inhibiting liver function, increasing the concentration of nitrogen-containing products in the intestine and the amount of blood flowing bypassing the liver through portocaval anastomoses.
Laboratory data occupy a rather modest place in the diagnosis of PE. It is known that neither liver function tests nor elevated plasma ammonia concentrations directly correlate with the severity of disturbances of consciousness.
Treatment of PE
Treatment of PE has three basic goals:
- identification and immediate elimination of factors provoking PE;
- reducing the amount of ammonia and other toxins formed in the intestines during digestion and the activity of microbial flora;
- normalization of neurotransmitter metabolism.
The treatment of PE (stages III and IV) is schematically presented in Table 6.
| Table 6. Treatment of hepatic encephalopathy. |
|
The scope of therapeutic measures for PE is one of the standard emergency care algorithms verified by clinical practice, since the effectiveness of treatment directly depends on the earliest possible start of therapy. In this sense, pharmacotherapy for PE directly relates to the presumption of emergency medical care. However, in practice it turns out that patients with PE, both at the prehospital stage and in the hospital, often do not receive adequate treatment. Moreover, in many cases, patients are prescribed pharmacotherapy, which can provoke a deterioration in the state of consciousness and disruption of autonomic functions. The most common treatment errors include:
- insufficient infusion of concentrated glucose solutions, which, in addition to energy-carrying activity, also have a strong osmotic effect, which is important for threatening cerebral edema;
- unreasonable and uncontrolled administration of isotonic and other non-concentrated polyionic solutions, which entails a direct threat of the development of cerebral and pulmonary edema;
- underestimation of the importance of the planned administration of osmotic laxatives and emergency bowel cleansing with high osmotic enemas (effectively reduce the absorption of ammonia in the intestine and its bacterial contamination, help reduce portal pressure);
- underestimation of the danger of diuretic therapy, massive laparocentesis and the prescription of sedatives in relation to the deepening of the stage of PE.
One of the most significant reasons for inadequate treatment is often the often unsatisfactory diagnosis of PE. Paradoxically, today in all levels of healthcare, against the backdrop of actually existing documents regulating medical activities, the identification and precise qualification of PE as a life-threatening complication of the underlying liver disease has largely lost its practical meaning. For example, in alcoholic liver disease, both in emergency medical services and in the hospital, PE is often not diagnosed at all, since it is included in the rarely used categories of “acute or subacute liver failure”, “acute hepatitis”, “acute alcohol poisoning” or “withdrawal condition”. In the overwhelming majority of cases, when alcoholic liver disease with impaired consciousness is detected, in practice, diagnoses are made that correspond to the headings K.70.0 - K.70.2, which in the case of PE does not at all reflect the real state of affairs (see Table 7). In addition, the term “PE” during diagnosis is often replaced by the term “toxic (alcoholic) encephalopathy,” which entails an underestimation of the severity of the patient’s condition and the risk of death and a late start of specific treatment.
| Table 7. Definition of alcoholic liver and brain disease according to ICD-10. |
Alcoholic liver disease
Alcohol diseases NS
Mental disorders
|
If PE is detected at the prehospital stage, patients with stages III and IV of impaired consciousness should be immediately hospitalized in the intensive care unit.
PE prognosis
The prognosis of PE depends entirely on the severity of hepatic cellular failure and the time of initiation of treatment. In liver cirrhosis, patients with relatively preserved parenchymal function and intense collateral circulation have a better prognosis, while patients with acute hepatitis have a worse prognosis. The prognosis improves significantly if it is possible to quickly eliminate the factors leading to worsening HE: infection, diuretic overdose or blood loss. However, the most effective way to improve the prognosis is to diagnose PE as accurately as possible and start treatment early.
Literature
- Mayer K.-P. Hepatitis and consequences of hepatitis. - M.: GEOTAR - MED., 2001.
- Sherlock S., Dooley J.. Liver diseases. - M.: GEOTAR - MED., 1999.
- Bailey B., Amre D. K, Gaudreault P. Crit Care Med 2003 Jan; 31(1):299-305.
- Carthy MM, Wilkinson ML BMJ 1999 May; 318:1256-9.
- Fedosiewicz-Wasiluk M. Pol Merkuriusz Lek 2002 Aug; 13(74):151-3.
- DW World J Gastroenterol 2002 Dec;8(6):961-5.
- Helewski KJ, Kowalczyk-Ziomek GI, Konecki JJ Wiad Lek 2002;55(5-6):301-9.
- McGuire BM Semin Gastrointest Dis 2003 Jan;14(1):39-42.
- Kelly DA Postgrad Med J 2002 Nov;78(925):660-7.
- Samuel DJ Gastroenterol Hepatol 2002 Dec;17 Suppl 3:S274-S279.
E. I. Vovk MGMSU, NNPOSMP, Moscow
Diagnostics
In order to determine the cause of halitosis, it is necessary to conduct a number of studies. The liver, stomach, and intestines are examined. The doctor examines the patient, assesses the condition and color of the skin, mucous membranes, and tongue.
A general blood test is required . In case of liver cirrhosis, liver failure and other severe pathologies, the blood changes characteristics, since its composition depends on the quality of purification. If the liver is not functioning sufficiently, this is immediately revealed by the state of the blood.
A stool examination may also be performed , since halitosis may indicate that the stomach or intestines are diseased. Incompletely digested food indicates insufficient functioning of the gastrointestinal tract, and sometimes the liver.
To make an accurate diagnosis, instrumental studies are also carried out. The stomach and gastrointestinal tract organs are examined using fibrogastroduodenoscopy. An ultrasound scan of the liver, pancreas, and gall bladder is performed. In severe cases, histological studies of tissues of the affected organ obtained by biopsy are necessary.
Condition of mucous membranes
If the liver does not function sufficiently, then additional stress is placed on the skin. The skin is able to filter and remove toxins, and when the liver does not cope with its task, this is sure to affect the condition of the skin and mucous membranes.
A yellowish or excessively pale skin color may indicate liver disease. Yellowness is observed in hepatitis and gallbladder diseases, and indicates a high level of bilirubin. White skin color, especially noticeable on the fingertips and face, can also indicate a diseased liver.
In liver pathologies, the mucous membranes and eye sclera also change color. Swelling of the skin and mucous membranes may occur. The skin becomes dry, pustules and pimples appear on them.
Treatment
Treatment of liver diseases is carried out by a hepatologist. Not all medical institutions have such specialists, so if there is no hepatologist, you can contact a gastroenterologist.
Treatment is prescribed based on the diagnostic results. The medications used, regimens and dosages depend on the diagnosis, stage and severity of the disease, the presence of concomitant diseases, and the age of the patient.
If liver inflammation of an infectious etiology is diagnosed, then therapy is carried out using antibacterial or antiviral agents against a specific pathogen. Broad-spectrum antibiotics may also be prescribed.
To restore hepatocyte function, drugs containing essential phospholipids are used . To support and cleanse the body of toxins in case of insufficient liver function, courses of vitamins and lipoic acid are prescribed.
In severe cases, drug therapy may not be effective enough. In case of advanced diseases, the presence of malignant formations in the parenchyma of an organ, doctors are forced to undertake surgical treatment methods.
Features of the disease
If your breath smells unpleasant and strong, this may indicate that there are problems with the liver. It is necessary to examine this organ, as well as the stomach, if the smell is intense and constant, does not depend on the frequency of meals and its quality. The following manifestations are also observed in liver disease:
- changes in the color of the skin, mucous membranes and eye sclera, the skin becomes yellowish due to stagnation of bile,
- a putrid or garlicky smell comes not only from the mouth, but also from the skin,
- the color of the tongue changes, a coating appears on it,
- skin rashes appear that cause serious discomfort,
- dilation of veins, appearance of spider veins on the abdomen,
- dyspeptic symptoms: nausea, flatulence, periodic bowel movements,
- feeling of a bitter taste in the mouth,
- fatigue with little exertion, excessive drowsiness,
- pain in the right side of the abdomen.
If all these signs are observed, then it is necessary to urgently consult a doctor , since this combination indicates a serious illness characterized by insufficient functioning of the liver.
Menu adjustments
When liver pathologies are detected, treatment is necessarily accompanied by the prescription of a special diet. The frequency of food intake, the method of processing it, and the temperature matter.
You need to eat food in small portions at fairly short intervals. Food should not be too cold or hot. You should not eat fried, canned, smoked, overly salted or spicy foods.
These measures help not to overload the liver, distributing the load evenly. You should also avoid eating fatty foods, confectionery, marinades, and sausages. No seasonings are used during cooking; salt is added in minimal quantities. Food is steamed, boiled or baked.
You should stop eating bread. You can eat biscuits or toasted baguette.
If you have liver disease, it is strictly forbidden to drink alcohol, since the diseased organ is simply not able to process it. You can’t drink sweet soda; you need to minimize the consumption of coffee and strong tea. You should drink only natural, non-concentrated juices.
It is useful to eat honey, nuts, dried fruits. Fermented milk products should be consumed with caution, little by little. Whole milk is excluded. Animal fats must be replaced with vegetable fats. Moderate but obligatory consumption of vegetable oils is beneficial for a diseased liver.
What to do?
To get rid of bad breath with cirrhosis of the liver, it is necessary to undergo a full course of treatment for this disease. In particularly advanced cases, drug methods do not lead to the desired results, so doctors are forced to resort to dangerous surgery.
Therefore, if you detect even a slight liver odor from the mouth and a slight yellowing of the tongue, it is recommended to immediately seek medical help.
A qualified hepatologist should direct therapeutic treatment. The liver is an organ that is very sensitive to medications, and the wrong course of treatment (which is a consequence of an incorrect diagnosis) can lead to a catastrophic development of events, even death for the patient.
Diagnosis of liver cirrhosis should be carried out through the following procedures (the patient has the right to request them):
- blood tests - biochemical and general;
- stool, for undigested food debris;