The condition of the tongue has long been considered an indicator of human health. Glossitis is a whole group of tongue diseases. There are many clinical variants of glossitis and the causes of its occurrence. In many diseases, a change in the appearance of the tongue is the main manifestation of the disease. Treatment tactics and prognosis depend on timely and correct diagnosis of the type of glossitis and the cause of its occurrence.
Anatomy of the tongue
The tongue is divided into: body, apex and root. The tongue consists of muscles and is covered with epithelium. Also on the back of the tongue there are many special papillae with which we feel taste. The largest grooved papillae are located closer to the root of the tongue. In the center of the tongue there are filiform papillae, on the sides there are leaf-shaped papillae. And in front of the tongue there are mushroom-shaped papillae.
Symptoms of geographic glossitis
It is not always easy to identify the disease, especially if it is at an early stage or in a chronic form. However, the following symptoms may indicate that the patient has desquamative glossitis and will need to consult a dentist:
- burning sensation, itching, tingling (mainly during eating);
- chaotically located red spots with a light rim;
- enlarged lingual papillae;
- the appearance of deep (and often painful) folds and furrows;
- sensation as if there is a foreign body in the mouth;
- in some cases, the appearance of a whitish or yellowish coating;
- discoloration and swelling of the tongue;
- increased salivation.
Attention!
Desquamation appears gradually: first, some areas of the tongue are covered with a light coating, and then it separates, exposing the smooth surface. But after a few days, the epithelium, as a rule, is restored, and the lesion covers another area of the mucosa. Such spots can be of different diameters and located both on the upper and lateral parts of the tongue.
There are 3 forms of the disease
- Superficial, characterized by a slight burning sensation, the appearance of clearly defined spots, and roughness of the tongue.
- Hyperplastic - with hardening of the affected areas, a white-gray coating and a feeling of a foreign body.
- Lichenoid, which usually occurs in the form of increased sensitivity of the tongue due to hypertrophied papillae.
Glossitis: the cause of the disease
Tongue diseases can be caused by infections caused by:
- Bacteria (streptococci, staphylococci, fusobacteria, etc.)
- Mushrooms
- Viruses
The tongue is often affected by common diseases:
- immune system diseases
- blood diseases
- diseases of the digestive system
- with a lack of vitamins, microelements (for example, iron and B12)
Also, the cause of glossitis can be irrational use of antibiotics, which disrupts the microflora of the oral cavity, or bad habits (smoking, alcohol).
Glossitis can occur due to tongue injuries:
- sharp edges of carious or damaged teeth, fillings
- old dentures, crowns
- when biting with teeth
- fish bones and other items
- gunshot and other types of injuries
- chemical irritants (for example, vinegar)
- hot food
- electric shock
Causes of desquamative glossitis
In medicine, there is no clear list of reasons why desquamative glossitis occurs. This disease can be diagnosed separately, or can be caused by certain systemic disorders.
The causes of primary desquamative glossitis include mechanical damage - injury from sharp edges of teeth or poorly fitted orthopedic structures, burns from hot food and chemicals. It is also common in young children as a reaction to the appearance of their first teeth.
Classification of glossitis according to the form of the lesion
- catarrhal form
- desquamative form
- purulent form
- neurogenic diseases of the tongue (impaired sensitivity of the tongue)
Catarrhal form of glossitis
With this form, only the upper layers of the tongue are affected. Areas of redness and swelling appear on the tongue. The tongue is coated, a burning sensation appears, the amount of saliva increases, and the mobility of the tongue is sometimes limited
Desquamative form of glossitis
With this form, only the upper layers of the tongue are affected. Areas of redness and swelling appear on the tongue. The tongue is coated, a burning sensation appears, the amount of saliva increases, and the mobility of the tongue is sometimes limited
Purulent form of glossitis
Its cause is infection, most often through a damaged mucous tongue.
It is characterized by a violation of the general condition, weakness, temperature 38-39°C, and enlarged lymph nodes. The tongue increases in volume and is covered with a gray coating, the saliva is viscous. Bad breath appears, it is difficult to swallow food, and even breathing may be difficult. If you notice the above symptoms, you should urgently seek medical help!
Separately, there are diseases in which only the tongue is affected without the rest of the oral mucosa:
- Desquamative glossitis
- Black hairy tongue
- Folded tongue
- Diamond-shaped glossitis
- Neurogenic diseases of the tongue
Hairy tongue
With this disease, filiform papillae grow and become black. Coloring occurs due to food and microflora. The disease is rare.
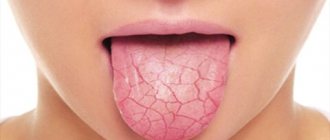
Desquamative glossitis
With this disease, the process of keratinization and changes in the papillae of the tongue are disrupted. More common in children. Part of the tongue is covered with red spots that can migrate to other areas. The disease is accompanied by dryness and impaired taste.
Diamond-shaped glossitis
A chronic disease of unknown cause in which a red or bluish diamond-shaped formation is located in the middle of the tongue in front of the circumvallate papillae. Usually there are no complaints, rarely dryness, pain, burning.
Folded tongue
A congenital disorder of the structure of the tongue, with it there are folds on the tongue, often symmetrical. Sometimes the disease is accompanied by an enlarged tongue. No subjective unpleasant sensations arise; only with insufficient oral hygiene, microorganisms can develop in the folds of the tongue, causing diseases (for example, candidiasis).
Neurogenic diseases of the tongue
Violation of the motor and trophic (nutritional) function of the tongue. They are expressed in impaired sensitivity, mobility, pain, as well as in impaired desquamation (detachment).
Classification and main types of glossitis
There is no uniform classification of forms of the disease. This is due to the variety of clinical variants of glossitis and the causes of their occurrence. According to the mechanism of appearance, primary and secondary forms of glossitis are distinguished. The primary form is an independent disease. Secondary glossitis is a consequence of existing diseases.
According to the leading mechanism of development, several variants of glossitis are distinguished:
- infectious (fungal, bacterial, viral);
- desquamative;
- folded;
- diamond-shaped;
- glossitis with chronic hyperplasia of filiform papillae (black “hairy” tongue);
- atrophic and hypoplastic.
A separate classification is used to describe the severity of the inflammatory process. Glossitis can be simple catarrhal, erosive-ulcerative or phlegmonous. Catarrhal glossitis is characterized by redness and swelling of the tissues of the tongue. In erosive-ulcerative forms of the disease, small cracks (erosions) or deep painful ulcers form on the mucous membrane of the tongue. The most severe form of the infectious-inflammatory process is phlegmon of the tongue (phlegmonous glossitis).
Diagnosis of glossitis
If symptoms of glossitis appear, you should consult a dentist.
The doctor will collect the entire history of the disease, complaints, duration of the disease, the success of previous treatment (if any). The doctor examines not only the tongue, but also the entire oral cavity, including teeth, crowns, and dentures.
In some cases, additional research may be needed:
- Ultrasound examination of the salivary glands
- Smear to identify the pathogen and select appropriate treatment
- Bacteriological culture of saliva
These studies are needed to find the cause of the disease and prevent complications.
Changes in appearance depending on the disease
One of the common types is “geographical tongue,” in which its upper surface resembles a map with the borders of countries and continents. This is the most common form of glossitis, which does not manifest itself in any way and does not require medical intervention unless complications arise (numbness, burning). This form occurs in waves, provoked by rough or spicy food, and hormonal cyclic changes. But the loss of the pattern of the papillae may indicate the presence of hypo- or hyperacid gastritis (that is, with increased or decreased acidity of gastric secretions) - such symptoms are typical for patients with gastroesophageal reflux, when hydrochloric acid and bile are thrown from the stomach into the oral cavity.
"Geographical language"
The second most common type of glossitis is a folded tongue. This is an independent type of glossitis. In this case, the back of the tongue seems to be riddled with deep cracks and it feels like there are folds in it. This form of glossitis sometimes accompanies neurological diseases (for example, Melkerson-Rosenthal syndrome) and is present in people with acromegaly (hormone-active pituitary tumor).
"Folded tongue"
Also characteristic are manifestations of various anemias, which are reflected in the appearance of the organ: iron deficiency anemia can manifest itself as a burning sensation on the tip of the tongue, the appearance of cracks on it and an erased pattern of taste buds. Pernicious anemia (B12 deficiency), in which the tongue has a “varnished” appearance with a smooth, swollen surface, sometimes quite painful, with burning symptoms, is the main cause of Gunther-Miller glossitis.
"Lacquered Tongue"
A large group of pathological conditions of this organ are ENT-associated symptoms associated with chronic tonsillitis - here the symptoms are non-specific, ranging from a dirty coating on the tongue to manifestations of diphtheria with white masses that are difficult to remove.
They also distinguish the formation of ulcers on the tongue - aphthous glossitis, which, as a rule, has a viral cause and goes away on its own. This is a recurrent disease, with more frequent episodes it is necessary to exclude pathology of the immune system.
When visiting a doctor, you will often notice pronounced teeth marks on the side of the tongue - a sign of long-term swelling. This occurs in patients with enterocolitis, kidney disease and cardiovascular diseases. The reason for this condition is water retention in the body.
Imprints from teeth on the lateral surface of the tongue
In the presence of abundant white plaque, accompanied by pronounced redness of the oral mucosa, one should suspect a fungal infection, often of a candidal nature. In this case, HIV must be excluded. Also with HIV, “hairy leukoplakia” occurs, when the tongue appears to have white hairs on the side surface, similar to flames - this condition is specific to HIV.
"White Hairy Tongue"
It is worth noting the existence of a “black hairy tongue”, which is a symptom of gastrointestinal disorders, less commonly a fungus.
"Black Hairy Tongue"
As you can see, our organ of taste reflects deep processes in the body, and it is difficult to single out one specialist responsible for its treatment. It is worth involving doctors of different spectrum in therapy, conducting studies based on data from smears and blood tests. But what general recommendations can we, as doctors, give to patients?
How to treat glossitis?
Treatment of glossitis is always comprehensive and carried out by a dentist. Also, if necessary, the help of a therapist, allergist, gastroenterologist, ENT doctor, endocrinologist is required.
Treatment depends on the course and form of the disease and includes the following measures:
- Elimination of pockets of infection in the mouth (treatment of caries, its complications, replacement of old fillings, crowns)
- Professional oral hygiene – removing plaque and tartar to reduce irritation and reduce the number of microorganisms.
- Teaching the patient how to properly brush teeth at home, selecting appropriate products (paste, brush, brushes)
- Gentle diet (spicy, salty, hot, irritating foods must be excluded)
- If there is a general disease, it must be cured
Care instructions
- Hygiene. We brush our teeth, but forget about our tongue. Thanks to advertising in the media, people are more likely to buy toothbrushes with a special brush for cleaning the tongue - and this is important. After all, bacteria live in the gap between the taste buds and food particles remain that must be removed from there.
- Caring for your oral health. Do not forget about the cleanliness of the palatine tonsils and the presence of reflux of gastric contents into the oral cavity.
- And the most important thing is to monitor your general health, undergo a timely examination by a doctor to identify the cause of inflammation - primarily to the dentist, but if you even consult a therapist or an infectious disease specialist, or an ENT doctor - you will not be mistaken, since there are almost no diseases, which would not affect such an important organ one way or another.
Medicines for the treatment of glossitis
- Antibiotics
- Antifungal medications (to treat fungal infections)
- Antiviral medicines (to treat a viral infection)
- Immunomodulators (to enhance immune system function)
- Antihistamines (to reduce tongue swelling)
- Vitamins
- Applications of healing agents to lesions (Solcoseryl, rosehip oil, vitamin A)
All of these forms of drugs are selected individually, taking into account sensitivity to the identified pathogens. The duration of treatment is determined by the doctor in accordance with the form and severity of the disease.
Hairy black tongue (villous glossitis)
This form of glossitis is characterized by the growth and keratinization of filiform papillae (they become hair-like). The mechanism of development of this disease is not fully understood. According to one version, the development of villous glossitis is facilitated by the influence of local irritating factors, as well as candidiasis that develops while taking antibiotics.
Treatment of this form of glossitis includes mechanical (tweezers) removal of filiform papillae and subsequent treatment of the surface of the tongue with a solution of copper sulfate. For candidiasis, antifungal agents are prescribed.
Prevention of glossitis
- Timely diagnosis and treatment of common diseases. To do this, it is recommended to undergo regular medical examinations.
- Regular and proper brushing of teeth at home twice a day.
- Visit the dentist once every six months for examination and professional hygiene (if necessary).
- Healthy lifestyle. It is important to eat food with sufficient protein, fat, and carbohydrates. It is better to minimize irritating foods (smoked, salted). It is also necessary to normalize your sleep patterns.
- Rejection of bad habits. Tars in tobacco smoke irritate the mucous membrane of the tongue and also impair blood supply.
How is tongue inflammation treated?
The nature of treatment largely depends on the form and type of pathology. Therefore, diagnosing the disease is important when prescribing effective treatment.
In some cases, it is useless to treat glossitis itself until the root cause of the pathology is eliminated - one of the diseases of the internal organs.
Treatment of glossitis has the following general principles:
- A doctor prescribes a procedure to improve the health of the entire oral cavity.
- Using various antiseptics to rinse the mouth, for example, Miramistin, Chlorhexidine, Furacilin. If the disease manifests itself in a child, then the drug Nystatin can be used for treatment.
- When erosive areas and ulcers appear on the surface of the tongue due to glossitis, the patient is prescribed ointments with a healing effect: Kamistad, Malavit, Vinizol.
- After removing the main symptoms of the pathology, treatment of glossitis is usually completed by treating problem areas with various oils of plant origin.
- The last stage is to carry out activities aimed at increasing general and local immunity.
The methods of treatment of tongue diseases listed above are advisory in nature for all. However, they will be quite effective in most cases.
Please note that folded glossitis does not require treatment.
Answers to popular questions about glossitis
Do I need to clean my tongue?
Yes, definitely.
A lot of microorganisms accumulate on the tongue, which leads to bad breath. In case of acute glossitis, the primary task is to relieve inflammation; you can use oral baths or rinses with antiseptic solutions (chlorhexidine, miramistin), a decoction of chamomile has a positive effect (has a calming effect on inflamed tissues of the mucous membrane of the tongue and the oral cavity as a whole). Also, do not forget about careful cleaning of the surface of the tongue.
There are special scrapers (semi-oval) for cleaning the tongue. They are designed to gently cleanse the tongue. Do not clean your tongue with brushes or spoons, as this can cause injury.
Which doctor should I contact to treat glossitis?
If tongue pathology is detected, you can consult a dentist. And, if necessary, the dentist will refer you for consultation to other specialists if this is due to the presence of a general disease.
What diagnostics are carried out before treating glossitis?
The specialist to whom the patient contacted conducts an examination of the oral cavity, collects a medical history, data on the general condition of the body (the presence of chronic organ diseases, etc.), prescribes tests, as well as laboratory diagnostics: a smear or culture of the oral cavity and tongue to determine pathogenic microflora.
Are glossitis inherited?
Yes, some forms can be inherited, for example, a folded tongue.
Is it possible to completely cure glossitis?
Some forms can be successfully treated, but often glossitis is a chronic and congenital disease. But with proper therapy, you can achieve minimal manifestations of the disease.
What is glossitis?
What do we know about the tongue as an organ? We know that it is located in the mouth, which helps us articulate and pronounce words correctly, helps us mix food, feel all the diversity of existing tastes, that they can be shown indignation, and in some African countries, a demonstration of it can be used to declare war.
Such a significant number of different physiological and social functions may one day be compromised. And the name of this threat is glossitis.
Despite the absolutely clear location of this organ, there are big questions about which doctor deals with its problems: a dentist, gastroenterologist, maxillofacial surgeon or otolaryngologist. This is not an easy question, and sometimes you can endlessly go from one specialist to another. But let's finally understand this intriguing matter.
Types of disease
There are three forms of desquamative glossitis. Superficial is the classic form, involving clear, shiny and smooth spots or stripes of bright red color. Where there are no spots, the mucous membrane is healthy and looks normal. The patient with this form experiences a slight burning sensation.
The hyperplastic form of the disease is associated with the occurrence of focal compactions - due to hypertrophy of the papillae of the tongue and plaque. It comes in yellow, white or grey. If you ask the patient what he feels, he will note the feeling of something foreign, unnecessary in the mouth.
There is also a lichenoid form, characterized by migration of lesions, enlargement of fungiform papillae and a distinct burning sensation. More often it is caused by external factors, for example, allergies, hypersensitivity to those materials that were used in prosthetics and dental implants.
Causes of yeast glossitis
In most cases, the disease is a consequence of a weakened immune system. Therefore, more often than others, people who have suffered some kind of serious illness encounter it. Pathology also develops due to dysbiosis resulting from long-term antibiotic therapy, taking hormones or immunosuppressants.
Other reasons include:
- ulcerative glossitis/stomatitis not treated in a timely manner;
- frequent mechanical damage to the mucous membrane covering the tongue;
- deficiency of vitamins and minerals;
- liver dysfunction;
- disruption of the normal quantitative relationship between different fractions of blood proteins;
- thyroid diseases;
- oncology;
- frequent consumption of alcoholic beverages, smoking;
- deficiency of potassium in blood plasma;
- pregnancy, breastfeeding.
Tongue candidiasis also occurs as a result of direct contact with a carrier of the infection. This refers to the transmission of the disease during kissing, when using shared utensils. In newborn children, the cause of pathology is the passage of a sick mother through the birth canal.
Other symptoms and signs
Often desquamative glossitis of the tongue is accompanied by additional symptoms:
- a burning sensation, discomfort in the tongue area;
- tingling;
- irritation while eating;
- problems related to taste.
This disease can significantly reduce the quality of life because it constantly reminds itself, especially during meals.
You may also hear the name of the disease as “geographic tongue.” This is due to the fact that the appearance of the surface gives the impression that in front of you is a geographical map - such a bizarre pattern is made up of various uneven foci.
How and with what to treat glossitis of the tongue in adults and children
Treatment of tongue glossitis requires elimination of the diseases that led to its appearance. This refers to anemia, gastrointestinal diseases, syphilis, etc. To minimize pain, you need to rinse your mouth with Furacilin, a solution of Chlorhexidine (0.05%) or potassium permanganate, and avoid eating rough food. In case of severe pain, local applications with anesthetics can be made:
- Trimecaine solution (2%);
- Lidocaine solution;
- Pyromecaine solution.
If the tongue is dry, it should be lubricated with a mixture of glycerin and Anestezin.
For a speedy recovery, the skin of the tongue must be cleaned of plaque using a cotton swab soaked in proteolytic enzymes (Chymotrypsin, Trypsin). If there are painful ulcers, these drugs for the treatment of tongue glossitis can be replaced with applications with Iruksol. After the hygiene procedure, it is important to treat the cleaned lesions with antiseptics. This helps prevent secondary infection and also prevents the development of serious complications.
To speed up regeneration processes, gel and jelly-like medicines with solcoseryl, as well as preparations containing vitamin A, can be used. The mixture formed by rosehip oil and vitamin A heals the affected skin well and relieves pain.
If excessive thickening of the stratum corneum of the epidermis (hyperkeratosis) is observed, surgical intervention is ordered. Antifungal, antibacterial and anti-inflammatory drugs are selected taking into account the severity of the disease and the dominant symptoms.
All patients with glossitis can take immunomodulators. Hormones are used extremely rarely - only for difficulty breathing. To avoid atrophy of taste organ cells, Hydrocortisone and Prednisolone ointments are prescribed in short courses.
How to treat tongue glossitis at home
Treatment of tongue glossitis at home can be carried out using traditional medicine recipes:
- decoction of chamomile flowers. 1 tbsp. pour a glass of boiling water over the flowers. Infuse, strain. Rinse your mouth after every meal;
- bedstraw decoction. 1 tbsp. pour a glass of boiling water. Leave for 30 minutes. Take 50 ml orally after meals and rinse the mouth 3-4 times a day. Similarly, you can use decoctions of sage and basil;
- soda solution. Add 2-3 drops of iodine and a teaspoon of baking soda to a glass of warm water. Rinse your mouth 3 times a day;
- natural honey Slowly dissolve a spoonful of honey;
- propolis. Lubricate the areas of inflammation 5 times a day. Instead of propolis, you can use raw carrot/potato juice or rosehip oil;
- tea tree oil. Dilute in equal proportions with olive, sunflower or sea buckthorn oil. Treat glossitis lesions 5 times a day or keep it in your mouth for several minutes.
Preventive techniques for glossitis
Most often, the disease is much easier to prevent than to treat.
For this reason, dentists advise following the following preventive techniques:
- following the rules of dental and oral hygiene;
- systematic preventive examination in the dental office;
- reducing the use of hot spices that irritate the mucous membrane of the tongue;
- giving up cigarettes and alcoholic beverages.
Timely and high-quality treatment can easily eliminate glossitis, while the complete absence of therapy leads to irreversible and sad consequences.
Diamond tongue
The lesion is localized on the back of the organ; the tissues in this area, due to thickening of the epithelium, acquire a clearly defined oval or diamond-shaped shape. Diamond-shaped glossitis of the tongue, as in the photo, occurs chronically, but with periods of exacerbation. Often recurs. If treatment is not carried out, then neoplasms appear on the affected tissues, similar in appearance to papillomas or warts, covered with keratinized epithelium. May develop into a malignant tumor.
This is what rhomboid glossitis looks like
Diagnostics
Diagnosis of desquamative glossitis of the tongue is not easy, because sometimes it is necessary to exclude many diseases. For this purpose, different methods are used in laboratory studies:
- microbiological;
- biochemical;
- morphological;
- immunological;
- serological.
Patients undergo blood, stool, and saliva tests, and, if necessary, receive consultations from additional specialists. This is a dermatologist, allergist, endocrinologist, gastroenterologist, and often also a psychotherapist.
How to eat during treatment
Candida fungi multiply very quickly if a person eats a lot of sweets. Therefore, until complete recovery you need to stop eating:
- sweets;
- ice cream;
- baking.
Any alcoholic drinks are also prohibited.
Meat lovers should give preference to turkey and chicken. Buckwheat porridge is very useful - it contains many B vitamins. In order not to further irritate or injure the mucous membrane of the tongue, you should eat warm and well-chopped food.