Herpetic gingivostomatitis
This form of the disease develops due to the herpes virus type I.
Its symptoms include round ulcers with a white coating, red at the edges, no larger than 0.5 mm in size, covering the mucous membrane of the mouth and gums. Acute gingivostomatitis is characterized by high (up to 38-39 degrees) temperature, bleeding and swollen gums, and inflamed lymph nodes. The number of ulcers sometimes reaches 15-20 pieces. Weakness occurs, problems with eating due to pain, appetite disappears, sleep is disturbed. These symptoms may be accompanied by signs of acute respiratory viral infection or catarrhal tonsillitis.
Other types of gingivostomatitis - allergic, plasmacytic and atypical - are much less common.
Causes of gingivostomatitis
For the development of ulcerative gingivostomatitis, a number of factors are necessary, the main one of which is a decrease in the body’s protective reaction.
The disease usually occurs when one or more of the following factors are present:
— An organism weakened due to illnesses; — Hypothermia, colds: — Chronic infections and diseases; — Inflammatory processes in the mouth, tartar deposits; — Chronic injury to the oral mucosa (for example, due to dentures); — Diseases of the immune system (including HIV); — Lack of vitamins, iron deficiency anemia; — Lack of oral hygiene measures for a long time; - An allergic reaction to toothpaste, medications or any food.
Treatment
Treatment of mild forms of herpetic gingivitis in children is carried out on an outpatient basis under the supervision of a physician. In severe cases of the disease, the patient is hospitalized in a hospital. The patient is prescribed a diet with a predominance of pureed food that does not irritate the oral mucosa. It shouldn't be hot. There is no need to give your child solid food to prevent additional injury to the gums.
For mild forms, local treatment is used.
The following drugs are used:
- antiviral agents (Acicovir, Ganciclovir) - destroy the DNA of the virus, use ointment to lubricate the gums up to five times a day for two weeks;
- local anesthetic gels and ointments (Lidochlor gel, Kamistad) - they anesthetize, disinfect, have an anti-inflammatory effect, are used three times a day, two weeks;
- local antiseptics (Iodinol, Miramistin, Hexoral) - these agents rinse the mouth every four hours, two weeks;
- reparative preparations (Solcoseryl-gel, Methyluracil ointment) - applying ointments to ulcers promotes their epithelization and rapid healing, applied three times a day for two weeks.
Herbal infusions (chamomile, rose hips, calendula, sage, St. John's wort, licorice) are widely used for rinsing when gums are damaged.
In severe cases, the baby is prescribed oral medications.
The following drugs are prescribed:
- antiviral drugs (Famciclovir, Acyclovir, Zovirax) - taken according to the regimen prescribed by the doctor, the drug must be taken to the end, otherwise there will be a relapse;
- antihistamines (Suprastin, Tavegil, Citrine) - reduce swelling of gum tissue and reduce pain;
- antipyretics (Panadol, Nurofen) are used to reduce high fever.
Parents should monitor the baby’s oral hygiene; during illness, it is carried out especially carefully. To prevent gum injury, it is recommended to use toothbrushes with soft bristles. It is necessary to treat toys and objects that the baby uses with antiseptics.
Gingivostomatitis in children
Most often in childhood, gingivostomatitis occurs, caused by the herpes virus.
The disease occurs in an acute form, usually of moderate or severe severity. Gingivostomatitis in a child begins with a sharp rise in temperature, lethargy, and headache. All these symptoms in children appear even before ulcers appear in the mouth, and they can easily be confused with signs of a cold or flu: there is a cough, runny nose, and sometimes diarrhea.
Upon examination, enlarged lymph nodes under the jaw and on the neck and reddened gums are detected. For 2-3 days, the oral mucosa becomes covered with ulcers, which are very painful. The illness lasts one to two weeks.
Treatment of gingivostomatitis consists of aseptic treatment and anesthesia of the oral cavity, as well as antiviral therapy and strengthening the immune system.
Primary infection
Most cases of primary infection are asymptomatic, and clinical lesions are observed in a minority of infected individuals. After an incubation period (2–14 days), the disease manifests itself in the form of herpetic gingivostomatitis or dermatitis.
Herpetic gingivostomatitis
The most common clinical manifestation of primary HSV-1 infection is gingivostomatitis in children and young adults. Fever for 2 to 7 days, malaise, myalgia, inability to eat, irritability, and cervical adenopathy are also typical. Exudative or ulcerative pharyngitis may be present. Multiple ulcerations appear in the back of the mouth; lesions on the oral mucosa may persist for 2-3 weeks. The most common complication of infection is dehydration in children due to refusal to take fluids by mouth, which may require hospitalization. In sexually active individuals, HSV-2 can cause a primary infection in the form of oral lesions and pharyngitis, which are associated with moderate to severe pain and systemic symptoms simulating bacterial tonsillitis.
Herpetic dermatitis
The usual localization of rashes is the circumference of the mouth, especially the red border of the lips, nose. In more rare cases, the rash is located in the area of the cheeks, temples, eyelids, ears - this localization is called simple gladiator herpes (Gladiatorum Herpes Simplex Virus), as it is often found in wrestlers. The rashes are grouped hemispherical blisters against a background of erythema and edema. 1–2 days before the rash appears, patients feel a burning sensation, tingling, itching in the places where the rash will appear in the future. The contents of the vesicles are transparent, then become cloudy. Closely located bubbles can merge into a multi-chambered continuous bubble. After the bubbles open, erosions and crusts form.
The process on the skin resolves within 10–14 days. In the case of a secondary infection, relapse continues for up to 3–4 weeks.
Atypical forms of herpetic dermatitis
- Zosteriform herpes simplex is characterized by the appearance of vesicles along one or another nerve of the face, limb, or buttocks. This form differs from herpes zoster in the absence of pain radiating along the nerve.
- The abortive form occurs in areas of skin with a thickened stratum corneum on the skin of the palms and fingers. It manifests itself as barely noticeable vesiculopapular elements, accompanied by itching, burning, and pain along the nerves.
- The edematous form occurs on skin with loose subcutaneous tissue - eyelids, lips. Due to severe swelling, the primary elements are not visible.
- The elephantiasis-like form is an edematous form with the development of persistent lymphostasis in the lesion.
- The ulcerative form is characterized by the formation of small ulcers at the site of ordinary herpetic eruptions. The ulcers slowly increase in size and do not epithelialize for a long time. If they persist for more than 3 months, then they are classified as AIDS-marker diseases.
- The hemorrhagic form is characterized by the appearance of blisters with bloody contents; the rash can be located on any part of the skin.
- The hemorrhagic-necrotic form occurs with necrosis at the site of the rash and the formation of scars.
Complications of primary infection
Common complications of a primary infection are:
- eczema herpetiformis in atopics;
- keratoconjunctivitis;
- autoinoculation;
- dissemination of HSV infection in other skin conditions such as Darier's disease, mycosis fungoides, ichthyosis vulgaris and congenital ichthyosiform erythroderma.
Recurrent infection
Based on the natural history of HSV-1, infection is now defined as a persistent chronic infection of sensory ganglia with varying degrees of epithelial expression. Up to 40% of people infected with HSV-1 have a clinical relapse at some stage. Asymptomatic spread of HSV-1 in saliva has been reported in 1-10% of adult cases.
Factors that provoke reactivation of the virus include:
- exposure to ultraviolet radiation;
- illness with fever;
- stress;
- premenstrual tension;
- surgical procedures;
- dental surgical procedures;
- dermabrasion, including laser therapy;
- neurosurgical interventions.
Most individuals who develop a recurrent infection have a prodromal phase with sensations of burning, itching, numbness and/or pain. This phase occurs over 6-12 hours and is followed by clinical symptoms. Groups of vesicles appear on an erythematous or papular base at the junction of the skin and mucous membranes on the lips and on the internal keratinized areas of the oral cavity, such as the gums and hard palate. The ulceration phase is very short, followed by a long crusting phase with an average duration of 133 hours. The total healing time is 7-10 days.
Atypical forms of recurrent herpes infection
Patients with immunodeficiency and HSV-1 infection have an increased level of viral activation - 70-80%. In such patients, ulcerations develop primarily around the mouth and within the oral cavity, both in keratinized areas and in areas where keratinization is absent.
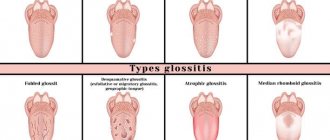
- Herpetic geometric glossitis
was first described in 1993 as a characteristic pattern of HSV infection of the tongue in organ transplant patients and in HIV-infected patients. - A migratory form in which during each relapse the rash is located in new areas.
Complications of orofacial recurrent HSV infection
- eczema herpetiformis;
- recurrent eczema multiforme;
- nosocomial spread of infection, including neonatal herpes;
- herpetic whitlow in dentists and other health care workers.
Symptoms
Clinical features of epiglottitis vary depending on the etiology, age, and severity of the disease.
In young children, respiratory distress syndrome is usually diagnosed - a progressive respiratory disorder, manifested by shortness of breath, chest depression during inspiration, cyanosis, pallor of the skin, and wheezing when breathing. To facilitate breathing, the child takes a sitting position with the body tilted forward, the neck is extended, the chin is pushed forward. Drooling may occur.
In older children, adolescents and adults, epiglottitis is more often manifested by a sore throat and drooling. During pharyngoscopy (examination of the pharynx), there is often no hyperemia and swelling - the oropharynx looks healthy.
Epiglottitis in children is characterized by a sharp onset and rapid progression of the disease. As a rule, 12-24 hours pass from the moment of the first signs to hospitalization.
The main symptoms of the disease in children:
- difficulty breathing (80%);
- stridor - noisy, wheezing breathing (80%);
- muffled voice or hoarseness (79%);
- pharyngitis (73%);
- fever (57%);
- sore throat (50%);
- sensitivity of the anterior surface of the neck (38%);
- cough (30%);
- difficulty swallowing (26%);
- voice change (20%).
The main symptoms of the disease in adults:
- sore throat (90-100%);
- fever ≥37.5°C (26-90%);
- muffled voice (50-80%);
- drooling (15-65%);
- stridor (33%);
- hoarseness (20-40%).
Herpetic stomatitis: symptoms
Taking into account the nature of the disease and the characteristics of its course in the patient, two forms are distinguished: acute and chronic recurrent. In the first form, the symptoms are very pronounced, the disease is more severe, and all signs usually disappear completely after adequate treatment. In the chronic relapsing form, the symptoms are less pronounced, long periods of remission (“rest”) are observed with periodic relapses.
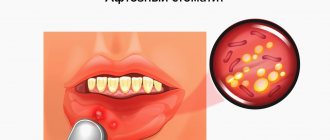
Acute herpetic stomatitis most often occurs in young children and adolescents. In adults, this disease occurs much less frequently, since their immune system works better and more actively than children's. This disease is also called herpetic aphthous stomatitis, due to specific aphthous ulcers in the patient’s mouth. The main signs of stomatitis in children and adults are:
- Swelling and redness of the mucous membranes of the mouth.
- Single or grouped vesicles with serous contents in small areas of the mucous membrane. When such bubbles collapse, erosive spots with a whitish coating in the center are formed. Such erosions are very similar to true aphthae, so the disease was previously classified as herpetic aphthous stomatitis, although in fact we are talking about two different types of the same disease.
- Pain when eating and drinking, burning and itching in the mouth.
- Weakness, fever, nausea, possibly vomiting and diarrhea. These symptoms almost do not appear with mild degrees of the disease; with moderate and severe degrees they are quite pronounced.
What the oral cavity looks like with herpetic stomatitis can be seen in the photo.