From this article you will learn:
- how to treat aphthous stomatitis in children,
- symptoms and treatment of aphthous stomatitis in adults,
- list of effective drugs.
The article was written by a dentist with more than 19 years of experience.
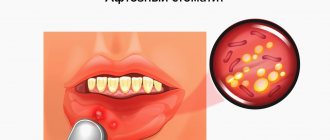
Aphthous stomatitis is a disease in which one or more round ulcerations appear on the oral mucosa, which are covered with a necrotic coating of a gray or yellowish tint. Such ulcers (synonymous with aphthae) are not the result of acute infections, and therefore are not contagious, but nevertheless, such damage to the mucous membrane will require specific therapy.
According to statistics, up to 20% of the population suffers from this form of stomatitis. Young children, as well as adults aged 20 to 30 years, are especially susceptible to this disease. In people of more mature age, there is a dependence: the higher the age, the less likely it is to develop. Aphthous stomatitis has a code according to ICD 10 - K12.0. Below you can see what this disease looks like in children and adults.
Aphthous stomatitis in children: photo
Aphthous stomatitis: photos in adults
The most important thing in treating stomatitis is to first correctly determine its form. Indeed, depending on its form, and it can be either herpetic or aphthous stomatitis, treatment for both adults and children will be completely different. Therefore, if you are not very sure of the diagnosis, it is best to familiarize yourself with the symptoms of both forms before starting treatment.
Causes of stomatitis
Stomatitis is both an independent disease and a manifestation of other diseases. The causes of stomatitis can be:
| CAUSES | A COMMENT | ||
| causes: | Viruses: | a comment: | herpes simplex virus, varicella-zoster virus |
| causes: | Mushrooms: | a comment: | yeast-like fungi of the genus Candida. |
| causes: | Bacteria: | a comment: | fusobacteria, streptococci, gonococci, mycobacterium tuberculosis, mycobacterium leprosy. |
| causes: | Allergy: | a comment: | stomatitis can be a consequence of food, household and drug allergies. |
| causes: | Injuries | ||
| causes: | Hygiene: | a comment: | Poor oral hygiene, this includes both the presence of dental deposits (tartar and plaque), and the presence of many foci of infection (caries and its complications), old fillings and crowns. |
| causes: | A number of diseases: | a comment: | — diseases of the digestive system (Crohn’s disease2, gastroesophageal reflux disease3, gastritis4) — chronic heart failure5 — diabetes mellitus6 — vitamin C hypovitaminosis — chronic tonsillitis — insufficient pancreatic function |
Classification of stomatitis by the World Health Organization7
| CLASSIFICATION | A COMMENT | ||
| classification: | According to the degree of damage to the mucous membrane | a comment: | 1) Superficial (catarrhal, fibrinous) 2) Deep (ulcerative, necrotic) |
| classification: | Due to the occurrence: | a comment: | 1) infectious (viral, bacterial, fungal) 2) traumatic (mechanical, chemical or physical injury) 3) allergic 4) arising from systemic diseases |
| classification: | According to the clinical course: | a comment: | 1) acute 2) chronic |
Catarrhal stomatitis
Characterized by redness, slight swelling, burning of the mucous membrane. It is observed with influenza, acute respiratory viral infections, and drug-induced damage.
Fibrinous stomatitis
It manifests itself as single painful aphthae, which are covered with a white coating. Afta is a superficial defect of the oral mucosa of a round shape. It appears in mild forms of aphthous stomatitis.
Ulcerative stomatitis
manifests itself in the form of deep defects in the oral mucosa - ulcers. Observed in traumatic stomatitis.
Necrotizing stomatitis
Characterized by ulcers that are covered with necrotic plaque. It is observed in ulcerative-necrotizing gingivitis, a complication of measles.
Acute stomatitis
It has pronounced symptoms, as a rule, it appears for the first time or recurs extremely rarely, once every few years. Also occurs due to acute trauma. Patients complain of severe pain, difficulty eating and sometimes even talking, general weakness, fever, and bad breath. Acute stomatitis with incomplete or improper treatment can become chronic.
Chronic stomatitis
Characterized by constant relapses, as a rule, this occurs when the immune system is weakened. May occur as a result of regular, moderate trauma. Clinical manifestations are less pronounced; this type of stomatitis always requires first of all eliminating the cause of the disease.
Types of disease
According to ICD-10, aphthous stomatitis is assigned code K.12. Within the code there are three qualifying diagnoses, including K.12.0 - “recurrent aphthae of the oral cavity,” which also includes aphthous ulcers.
According to the form of occurrence, acute and chronic aphthous stomatitis are distinguished. The first is characterized by the appearance of ulcers and severe hyperemia - swelling, redness of the mucous membranes. Severe pain occurs, especially when eating or talking. Submandibular lymph nodes may enlarge and body temperature may rise.
Chronic recurrent aphthous stomatitis may be the result of improper or untimely treatment, as well as the inability of the immune system to cope with the disease. It is characterized by periodic exacerbations. Outside of exacerbation, symptoms may be erased or completely absent.
The disease is classified into three forms depending on the severity:
- light. From 1 to 2 afts up to 10 mm in size. Moderate pain during mechanical action, relapses occur no more than 2 times a year;
- average. Up to 5 aft, the course of treatment takes up to 3 weeks. The pain is quite pronounced, there is an enlargement of the lymph nodes, relapses up to 2 times a year;
- heavy. Multiple aphthae appear, severe pain. An increase in temperature occurs, and symptoms of general intoxication appear. Treatment takes up to a month, relapses occur up to 6 times a year.
Also, according to the form of occurrence, the following types of inflammatory diseases are distinguished:
- fibrous: blood microcirculation in the upper layer of the mucosa is disrupted, aphthae appear, covered with a fibrous film (plaque). Such ulcers heal completely within 14 days. The disease affects the mucous membrane of the lips, the lateral surfaces of the tongue, and transitional folds. This stomatitis recurs up to 3 times a year;
- necrotic. The epithelium is destroyed, the mucosal area dies. Replacement of tissues with normal epithelium takes from 14 to 30 days. This aphthous stomatitis is not accompanied by acute pain; it is usually observed in patients with severe diseases, including blood pathologies;
- grandular. Damage to the ducts of the minor salivary glands occurs. In this regard, aphthae form close to the glands, and drying of the mucous membranes of the oral cavity occurs due to a decrease in saliva production. Ulcerations are painful and heal within 1–3 weeks;
- scarring. Damage to the cavity of the salivary glands leads to the involvement of connective tissue in inflammation. Aphthae are observed both at the location of the glands and on the mucous membranes of the pharynx and palate. The disease develops into large painful ulcers (up to 1.5 cm). Healing takes up to 12 weeks; after the acute process, pronounced scars remain;
- deforming. The most severe form of the disease, which provokes changes in connective tissue. Aphthae heal extremely slowly, which is accompanied by deformation of the palate, lips, and sometimes narrowing of the oral cavity occurs (if aphthae was observed in the corners of the mouth).
Ask a Question
Viral stomatitis
Herpetic stomatitis
Caused by the herpes virus of the first, less often the second type.
It accounts for 80% of all stomatitis and occurs mainly in children, less often in adults. The prevalence of herpes simplex virus ranges from 65% to 90%8. Infection occurs through airborne droplets and household contact. More common is recurrent herpetic stomatitis, which is manifested by itching, burning, slight soreness in the oral cavity, then vesicles (bubbles) appear, which burst and heal after 7-10 days.
During primary infection, acute herpetic stomatitis occurs; it is characterized by general symptoms such as fever, weakness, aches in the muscles and joints, the degree of these manifestations depends on the severity of the disease. As a rule, the acute form occurs in children.
Varicella zoster virus infection
The mildest form, in which the mucous membrane of the tonsils is affected. The palatine tonsils are not very enlarged, the mucous membrane of the throat is red, there is no plaque or pus.
Stomatitis with measles
Measles is an acute viral, highly contagious disease that is caused by the Polinisa virus and is transmitted by airborne droplets. The disease is extremely contagious. It is characterized by a rise in temperature, symptoms of ARVI, a rash on the face, neck, and then the whole body. In the oral cavity, Filatov-Koplik spots and stomatitis occur, which is characterized by hyperemia, swelling of the mucous membrane and white plaque. Nowadays, thanks to vaccination, this disease practically does not occur.
Features of treatment in children
The dentist will tell you how to treat aphthous stomatitis in a child. You can contact him at the direction of your pediatrician or on your own if you find characteristic ulcers in the oral cavity. The treatment regimen is the same as that used in the treatment of adult patients, but there are some differences: children under a certain age cannot rinse the mouth, so preference is given to drugs for application to mucosal ulcers. Otherwise, the treatment regimen is developed individually, taking into account the severity, symptoms of the disease, frequency of relapses, and the presence or absence of concomitant ailments in the child. Symptomatic therapy can be used to quickly alleviate the baby’s condition.
Specialists at STOMA clinics successfully treat aphthous stomatitis. By contacting us, you will receive qualified assistance, detailed recommendations on the treatment and prevention of relapse of the disease, and comprehensive assistance from dentists of all specializations, if necessary.
Stomatitis caused by fungi
Candidal stomatitis is a fungal disease caused by fungi of the genus Candida.10 Young children and the elderly are more often affected; people with diabetes and xerostomia (dry mouth), pregnant women and people with weakened immune systems are also at risk. Elderly people wearing removable dentures often get sick.
The main symptom of fungal stomatitis is a burning sensation and the presence of a white, cheesy coating, when removed, a swollen, red mucous membrane appears. The general condition of adults with candidal stomatitis is practically not affected.
Bacterial stomatitis
Vincent's ulcerative necrotizing stomatitis
It manifests itself as ulcerations of the mucous membrane, strong odor from the mouth, fever, weakness, pain when eating. In severe forms, ulcerations can occupy almost the entire oral cavity, and the temperature rises above 38°C.
Gonorrheal stomatitis
Caused by Neisser's gonococcus. The mucous membranes of the lips, gums, lateral and lower surfaces of the tongue are mainly affected. The mucous membrane has a brightly hyperemic color and a large amount of gray purulent plaque with an unpleasant odor. But, as a rule, there are no complaints.
Acute streptococcal gingivostomatitis
It is characterized by general damage to the gums, severe pain, fever, enlargement and tenderness of the lymph nodes. The mucous membrane of the mouth and tonsils is hyperemic, abscesses may form.
Traumatic stomatitis
Traumatic stomatitis develops as a result of mechanical, thermal or physical trauma. This type of stomatitis occurs:
- superficial (burn of the mucous membrane by hot tea)
- deep (burn with a strong alkali or acid, strong biting of the mucous membrane)
Acute mechanical stomatitis: rare, it can be caused by trauma to the mucous membrane when biting the cheek, tongue, lip while eating, an attack of epilepsy, a blow, trauma during dental treatment and other traumatic factors.
It is manifested by pain, hyperemia, swelling at the site of injury, erosion. With secondary infection, the wound can develop into long-term non-healing ulcers. Most often, traumatic stomatitis is acute, but can also be chronic, for example, constant biting of the cheeks under stress, chronic injury from braces, a sharp tooth edge, or a bad crown. As a result of trauma, painful erosions or ulcers with jagged edges form on the mucous membrane, which can become infected.
The cause of physical injury is most often a thermal burn due to contact with hot liquid, inhalation of steam, or exposure to fire, the latter, as a rule, accompanied by damage to the respiratory tract. The lesion is most often located on the tip of the tongue, lips, and the front of the palate. The mucous membrane becomes swollen, red, painful, and blisters may form, which then burst. With deep damage, the mucous membrane dies, and the damage involves muscles and even bone.
Chemical stomatitis occurs when burned with acid or alkali. In everyday life, this is most often acetic acid; also at a dental appointment, burns can occur with various drugs (phenol, formaldehyde, alcohol, hydrofluoric acid, etc.). The depth of damage depends on the damaging substance and its concentration, and the duration of exposure. First, the mucous membrane becomes bright red and painful, and with severe lesions, foci of necrosis then appear within a few hours.
In case of burns with acids, alkalis, or thermal burns, it is recommended to call an ambulance!
Allergic stomatitis
They arise as a reaction of the mucous membrane to an allergen. An allergic agent can be toothpastes, mouthwashes, food, medicines, materials for crowns, fillings, etc. Allergies often occur to removable dentures. The mucous membrane is affected precisely at the point of contact with the damaging agent, for example, the hard palate under a removable denture. With allergic stomatitis, the mucous membrane is swollen, red, bubbles appear, which burst with the appearance of painful erosions.
Allergic stomatitis also includes chronic recurrent aphthous stomatitis , it begins with swelling and burning, then a painful aphtha appears, and then a healing period begins. This disease is characterized by constant relapses with a certain frequency.
Diagnostics
First of all, a visual examination is carried out: the dentist assesses the condition of the mucous membrane, looks for the presence of dentures, fillings and other materials that could become allergens. Then the doctor finds out the time of the first signs of the disease, the patient’s general well-being and possible factors of the disease: heredity, allergies, medication, diet, trips to other countries, contact with animals and insects. If allergic stomatitis is confirmed, tests are performed to clarify the allergen:
- study of the composition of saliva;
- sample from dentures or dental materials;
- immunogram;
- blood and urine tests.
Prevention of stomatitis
Consists of the following items:
- strengthening the immune system, giving up bad habits, hardening, playing sports, eating with a sufficient amount of macros and vitamins (especially vitamin C)
- regular visits to the dentist
- adequate brushing of teeth at home, as well as removal of dental plaque in the dentist’s office once every 6 months
- identifying the allergen and avoiding contact with it
- undergoing medical examination for timely detection of diseases
- treatment of systemic diseases
- taking antibiotics only as prescribed by a doctor, together with a course of probiotics, to avoid dysbiosis
- vaccination (against measles, chickenpox)
Tantum® Propolis
It is worth paying attention to Tantum Propolis, since propolis has an immunostimulating effect, promotes healing, and vitamin C, which is part of it, is responsible for regeneration, participating in the synthesis of collagen.
Propolis also has antiviral and antifungal effects. Therefore, vitamin therapy Tantum Propolis is an effective means of preventing stomatitis.12 Find out more
Features of treatment
The main goal of treating aphthous stomatitis is to completely get rid of the disease or at least reduce the frequency of relapses to a minimum. Therapy is aimed at relieving inflammation, relieving unpleasant symptoms, and accelerating the recovery processes of the mucous membrane.
For each specific case, the doctor will develop a set of measures. The main ones include local and systemic drug treatment.
Rinsing with antiseptics can be done using medications or mouth rinses that contain antibacterial components. An alternative to rinsing is to use a spray. Typically, the treatment regimen includes 2-3 sessions of 1-minute rinsing immediately after brushing your teeth.
Local treatment methods include the application of gels with anti-inflammatory and analgesic effects.
Occlusive agents can reduce pain and speed up the healing of mucous membranes. They form an insoluble film on the ulcer, protecting the affected area from exposure to adverse factors.
Local glucocorticoid therapy is used against the background of immune diseases, as well as when standard measures are ineffective. They eliminate pain and quickly relieve inflammation, shortening the healing period. Such products are used only according to indications and are available with a prescription. In some cases, it is advisable to inject the drug under the base of the ulcer; this is done by a doctor.
Epithelialization drugs are used after acute inflammation has resolved. The specialist will prescribe a gel with an analgesic and healing effect, usually this occurs 5–6 days after the start of complex therapy.
Local laser therapy can relieve pain, speed up the healing process, and minimize the risk of relapse.
Systemic treatment of aphthous stomatitis in adults involves taking the following drugs:
- antihistamines (anti-allergic, anti-edematous effect);
- glucocorticoids (anti-inflammatory, analgesic effect);
- immunomodulators (to stimulate defenses and accelerate recovery).
And if antiallergic drugs can be recommended to any patient even in the absence of information about the exact causes of stomatitis, then other drugs are prescribed only according to indications: in case of acute severe course of the disease, frequent relapses, and the presence of severe systemic pathologies. An additional method of treatment is vitamin therapy - taking vitamins C, group B.
In addition to the main course of treatment, all patients without exception are recommended to adhere to a hypoallergenic diet, avoid taking too hot drinks and dishes, and spicy, irritating foods. It is better to give preference to toothpaste without sodium lauryl sulfate, this component can provoke the disease.
It is important to continue your oral hygiene, even if it is difficult. To make brushing your teeth easier, choose a soft toothbrush. If the disease recurs frequently, it is necessary to pay attention to the general state of health, promptly treat teeth and gums, replace fillings and dental structures.
Treatment of stomatitis
Treatment of stomatitis depends on the severity and cause of the disease and includes the following measures:
1. For bacterial stomatitis, antibacterial drugs are prescribed. For fungal stomatitis - antifungal drugs, for viral ones - antiviral drugs
Important! Antibiotics, antiviral and antifungal drugs are prescribed only by the attending physician!
2. For high fever and pain, antipyretic and painkillers are prescribed
3. Vitamin therapy. It is especially important to take vitamins A, C, E
4. Immunomodulatory drugs
5. Antiseptic treatment of the oral cavity. Antiseptics are used in the form of solutions, sprays, tablets, ointments
6. Epithelializing agents are used after acute phenomena have subsided
7. Sanitation of the oral cavity, removal of dental plaque
8. A gentle diet
9. Eliminating allergens and taking antihistamines
Important! Stomatitis is treated by a dentist, in some cases together with a therapist, infectious disease specialist, allergist and dermatologist. If you have symptoms, consult a specialist.
Aphthous stomatitis: treatment, drugs
Aphthous stomatitis in adults is the same as canker sores in children - the treatment is the same, and the treatment strategy described below is suitable for patients of any age. As for the medications listed later in the article, some of them do have age restrictions, which we will also indicate.
Due to the fact that it is usually impossible to clearly identify the specific cause of aphthous stomatitis in a particular patient, treatment will be multifocal, i.e. drugs of several groups are used simultaneously. The choice of treatment strategy and medications will depend on the following 3 factors:
1) on the severity of symptoms, 2) on the frequency of relapses, 3) on identified predisposing factors.
Treatment at the first stage should be aimed at reducing pain and inflammation in the area of ulcers, and at the second and third stages - at speedy epithelization of ulcers and preventing their occurrence in the future. To facilitate the choice of the best treatment option, all patients can be divided into 3 types (according to the criteria - severity of the disease and frequency of relapses).
- Type A - in patients of this type, aphthous stomatitis occurs no more than several times during the year and is characterized by slight pain.
First of all, in such patients it is necessary to identify local predisposing factors and eliminate them (for example, overhanging edges of fillings or hygiene products with sodium lauryl sulfate). It is important to ask the patient about eating habits to evaluate a possible relationship between stomatitis outbreaks and certain foods. The patient is advised to avoid solid foods (eg, crackers, toast), all types of nuts, chocolate, eggs, acidic drinks or foods - fruit or citrus juices, tomatoes, pineapples, salty foods. You should avoid eating spicy foods, any spices, including pepper and curry, as well as alcoholic and carbonated drinks. In type A patients, local symptomatic therapy is mainly used, which includes antiseptic rinses and gel applications for pain and inflammation + antihistamines.
- Type B - in such patients, aphthous stomatitis develops almost monthly, and the ulcers are so painful that they force the patient to change habits (for example, brushing teeth less often due to severe pain). It remains important to identify local and general predisposing factors and, if possible, eliminate them. It is very important to teach patients of this type to feel the first signs of the imminent appearance of ulcers - burning, itching or swelling of the mucous membrane, in order to provide early local treatment even before the formation of the ulcers themselves.
- Type C - in patients of this type, ulcers are very painful, appear so often that while one lesion is healing, the next one appears almost immediately. This group also includes patients in whom local treatment in the oral cavity is completely ineffective, and improvement in their condition occurs only after the use of systemic therapy (we will also discuss such therapy below).
Answers to popular questions
Which doctor treats stomatitis?
The dentist, if necessary, can refer the patient to other doctors.
Do I need to take antibiotics for stomatitis?
Some forms of stomatitis require the use of antibacterial agents, but in most cases this is not only useless, but even dangerous, since it can lead to dysbacteriosis. Antibiotics should be taken only as prescribed by a doctor in the prescribed dosage.
How long does it take to treat stomatitis?
Depends on the severity and form of the disease. On average 7-10 days.
Is stomatitis contagious?
Not all forms of stomatitis are contagious. Traumatic stomatitis is absolutely not contagious. If stomatitis is caused by viruses, such as herpes or measles, the risk of infection is very high.
Systemic pharmacological treatment –
Systemic therapy includes 3 types of drugs - antihistamines, glucocorticoids and immunomodulators. Antihistamines can and should be prescribed to absolutely all patients with aphthous stomatitis (without exception), the cause of which has not been precisely established. As for the drugs of the other 2 groups, they are the second line of defense, after which there are essentially no other treatment options.
1) Antihistamines –
Antihistamines will be an excellent addition to local therapy even for mild cases of aphthous stomatitis. The fact is that aphthous stomatitis can often be caused by unidentified food allergens (or components of hygiene products, for example, parabens). Therefore, it makes sense to start taking 2nd generation antihistamines orally for a course of 7-10 days.
Modern antihistamines are well tolerated and do not have significant side effects, therefore, given the difficulty of identifying the true cause of ulceration, you can start taking them from the first day of the disease, or even better - in the prodromal period, when ulcers have not yet formed, but the patient can already feel at the site of their future occurrence there is a slight burning or itching.
Table No. 1 (examples of 2nd generation antihistamines)
Means for nonspecific hyposensitization - for moderate and severe forms of aphthous stomatitis, when we need to quickly reduce the patient's body's sensitivity to allergens - in this case, the use of drugs for nonspecific hyposensitization is indicated. For example, these could be subcutaneous injections of histoglobulin - 2 ml 2 times a week with an interval of 2-3 days (a total of 10-12 injections per course). Or we can prescribe intravenously - a 30% solution of sodium thiosulfate, 10 ml daily, for a total of 6-8 injections for a course. These are all prescription drugs!
2) Systemic glucocorticoids –
These drugs are a second line of defense and are a lifesaver for patients with acute severe outbreaks of canker sores, but these drugs can only be used as directed by a doctor. Typically, prednisolone tablets are used in adults at an initial dose of 25 mg/day for the first 7 days (followed by a gradual dose reduction). The total duration of the course of therapy is usually 15 days, but in severe cases it can even reach 1-2 months.
However, in a clinical study by Pakfetrat et al. (source) – good results of treatment with prednisolone were achieved when used at a dosage of only 5 mg/day. Prednisolone is an extremely effective drug for the treatment of severe forms of aphthous stomatitis, but its dosage must be selected individually for each patient (taking into account the severity and severity of the disease, as well as the patient’s health condition). Be aware that prednisone may cause long-term side effects.
The search for alternative, safer drugs made it possible to find that the drug "Montelukast" (usually used as an anti-asthmatic drug) - at a dose of 10 mg per day, like prednisolone, reduced the number of lesions, relieved pain and accelerated the healing of ulcers, but at the same time it caused significantly fewer side effects (clinical study - Femiano et al.). It is important that Montelukast can be used even when systemic glucocorticoids are contraindicated.
3) Immunomodulators –
Immunomodulators are also a second line of defense, as are glucocorticoids. Their use is especially indicated in patients who are diagnosed with chronic recurrent aphthous stomatitis (with frequent relapses and an aggressive course of the disease). For children over 1 year of age, this could be, for example, in the form of Thymogen nasal spray, but keep in mind that this is a prescription drug.
For children over 3 years old, the over-the-counter drug “Likopid” 1 mg is suitable, which is taken 1 tablet 3 times a day, for a total of 10 days (for resorption under the tongue or orally). However, despite the over-the-counter availability of this drug, we, in principle, recommend taking drugs from the group of systemic immunomodulators - only after consulting an immunologist.
For adults - in adults, for immunocorrection with recurrent aphthous stomatitis, it is optimal to use either the drug "Timogen" (in the form of intramuscular injections of 100 mg daily for 10 days), or "Levamisole", which restores normal phagocytic activity among macrophages and neutrophils and modulates T-lymphocyte-mediated immunity. It is prescribed - 150 mg 3 times a week (for 6 months).
You can also use the drug "Methyluracil" (1 tablet 0.5 g - 3 times a day, for 1 month). For the most severe outbreaks of aphthous stomatitis, you can use Thalidomide at a dose of 50-100 mg/day, but keep in mind that although with the use of this drug 85% of patients experience complete remission of severe lesions (already in the first 14 days) - it has very strong side effects. Keep in mind that all of the above medications can only be used as prescribed by a doctor!
Both children and adults can also use the over-the-counter drug "Imudon", which is available in the form of tablets for resorption in the oral cavity. But this drug affects only the local immunity of the oral mucosa, without affecting the immune system as a whole. The course of treatment is 6-8 tablets per day for resorption (course duration is from 10 to 20 days - depending on the severity and frequency of relapses of aphthous stomatitis).
4) Means for restoring intestinal microflora –
We have already said above that there is a clear correlation between gastrointestinal diseases and repeated outbreaks of aphthous stomatitis, which is explained by the significant influence of intestinal pathology on the state of the immune system. Therefore, such patients are always advised to take medications (probiotics) that normalize the intestinal microflora. This could be Linex or Bifiform, as well as Hilak-Forte or other similar drugs.
Probiotic Bifiform –